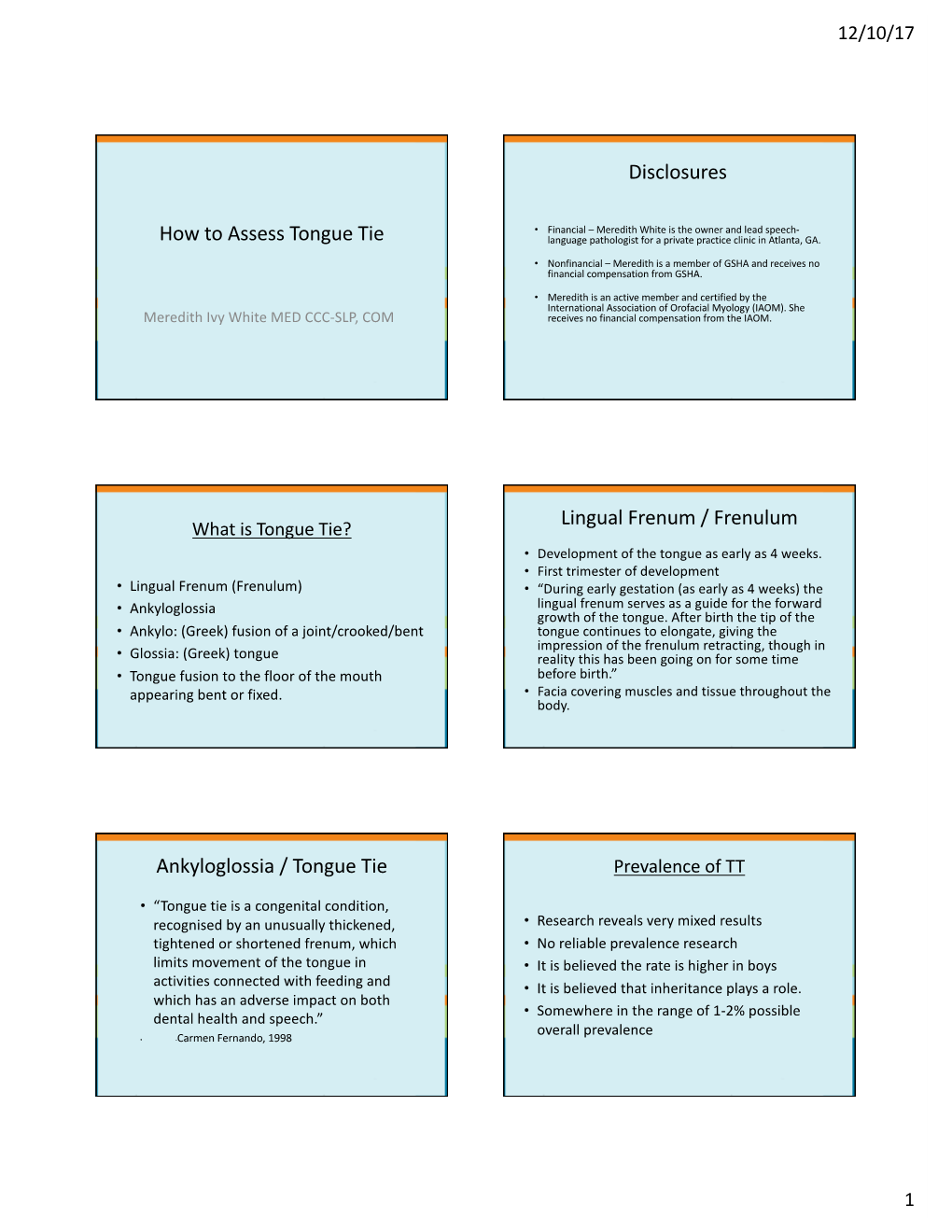
How to Assess Tongue Tie Language Pathologist for a Private Practice Clinic in Atlanta, GA
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Selecting Different Approaches for Palate and Pharynx Surgery
SPECIAL ISSUE 4: INVITED ARTICLE Selecting Different Approaches for Palate and Pharynx Surgery: Palatopharyngeal Arch Staging System Rodolfo Lugo-Saldaña1 , Karina Saldívar-Ponce2 , Irina González-Sáez3 , Daniela Hernández-Sirit4 , Patricia Mireles-García5 ABSTRACT The examination of the anatomical structures involved in the upper airway collapse in patients with the obstructive sleep apnea-hypopnea syndrome (OSAHS) is a key for integrated evaluation of patients. Our proposal is for a noninvasive classification system that guides us about the presence of anatomical differences between the palatopharyngeal muscle (PFM). The functions of the PFM are narrowing the isthmus, descending the palate, and raising the larynx during swallowing; these characteristics give the PFM a special role in the collapse of the lateral pharyngeal wall. Complete knowledge of the anatomy and classification of different variants can guide us to choose the appropriate surgical procedures for the lateral wall collapse. Until now there is not a consensus about description of the trajectory or anatomical variants of the PFM into oropharynx, the distance between both muscles, and the muscle tone. Here we also present the relationship between the lateral wall surgeries currently available (lateral pharyngoplasty by Cahali, expansion sphincteroplasty by Pang, relocation pharyngoplasty by Li, Roman blinds pharyngoplasty by Mantovani, and barbed sutures pharyngoplasty by Vicini) with the proposed classification of the palatopharyngeal arch staging system (PASS). Keywords: -

Abbreviations - Diagnosis
Abbreviations - Diagnosis AB abrasion AT attrition CA caries CFL cleft lip CFP cleft palate CLL cervical line lesion - See TR CMO craniomandibular osteopathy DT deciduous (primary) tooth DTC dentigerous cyst E enamel E/D enamel defect E/H enamel hypocalcification or hypoplasia FB foreign body FORL feline odontoclastic resorptive lesion - See TR FX fracture (tooth or jaw) G granuloma G/B buccal granuloma (cheek chewing lesion) G/L sublingual granuloma (tongue chewing lesion) G/E/L eosinophilic granuloma - lip G/E/P eosinophilic granuloma - palate G/E/T eosinophilic granuloma - tongue GH gingival hyperplasia GR gingival recession LAC laceration LAC/B laceration buccal (cheek) LAC/L laceration lip LAC/T laceration tongue MAL malocclusion MAL/1 class 1 malocclusion (neutroclusion - normal jaw relationship, specific teeth are incorrectly positioned) MAL/2 class 2 malocclusion (mandibular distoclusion - mandible shorter than maxilla) MAL/3 class 3 malocclusion (mandibular mesioclusion - maxilla shorter than mandible) BV buccoversion (crown directed towards cheek) CXB caudal crossbite DV distoversion (crown directed away from midline of dental arch) LABV labioversion (crown directed towards lip) LV linguoversion (crown directed towards tongue) MV mesioversion (crown directed towards midline of dental arch) OB open bite RXB rostral crossbite MN mandible or mandibular MN/FX mandibular fracture MX maxilla or maxillary MX/FX maxillary fracture OM oral mass OM/AD adenocarcinoma OM/EPA acanthomatous ameloblastoma (epulis) OM/EPF fibromatous epulis -

Lecture 2 – Bone
Oral Histology Summary Notes Enoch Ng Lecture 2 – Bone - Protection of brain, lungs, other internal organs - Structural support for heart, lungs, and marrow - Attachment sites for muscles - Mineral reservoir for calcium (99% of body’s) and phosphorous (85% of body’s) - Trap for dangerous minerals (ex:// lead) - Transduction of sound - Endocrine organ (osteocalcin regulates insulin signaling, glucose metabolism, and fat mass) Structure - Compact/Cortical o Diaphysis of long bone, “envelope” of cuboid bones (vertebrae) o 10% porosity, 70-80% calcified (4x mass of trabecular bone) o Protective, subject to bending/torsion/compressive forces o Has Haversian system structure - Trabecular/Cancellous o Metaphysis and epiphysis of long bone, cuboid bone o 3D branching lattice formed along areas of mechanical stress o 50-90% porosity, 15-25% calcified (1/4 mass of compact bone) o High surface area high cellular activity (has marrow) o Metabolic turnover 8x greater than cortical bone o Subject to compressive forces o Trabeculae lined with endosteum (contains osteoprogenitors, osteoblasts, osteoclasts) - Woven Bone o Immature/primitive, rapidly growing . Normally – embryos, newborns, fracture calluses, metaphyseal region of bone . Abnormally – tumors, osteogenesis imperfecta, Pagetic bone o Disorganized, no uniform orientation of collagen fibers, coarse fibers, cells randomly arranged, varying mineral content, isotropic mechanical behavior (behavior the same no matter direction of applied force) - Lamellar Bone o Mature bone, remodeling of woven -

Vestibule Lingual Frenulum Tongue Hyoid Bone Trachea (A) Soft Palate
Mouth (oral cavity) Parotid gland Tongue Sublingual gland Salivary Submandibular glands gland Esophagus Pharynx Stomach Pancreas (Spleen) Liver Gallbladder Transverse colon Duodenum Descending colon Small Jejunum Ascending colon intestine Ileum Large Cecum intestine Sigmoid colon Rectum Appendix Anus Anal canal © 2018 Pearson Education, Inc. 1 Nasopharynx Hard palate Soft palate Oral cavity Uvula Lips (labia) Palatine tonsil Vestibule Lingual tonsil Oropharynx Lingual frenulum Epiglottis Tongue Laryngopharynx Hyoid bone Esophagus Trachea (a) © 2018 Pearson Education, Inc. 2 Upper lip Gingivae Hard palate (gums) Soft palate Uvula Palatine tonsil Oropharynx Tongue (b) © 2018 Pearson Education, Inc. 3 Nasopharynx Hard palate Soft palate Oral cavity Uvula Lips (labia) Palatine tonsil Vestibule Lingual tonsil Oropharynx Lingual frenulum Epiglottis Tongue Laryngopharynx Hyoid bone Esophagus Trachea (a) © 2018 Pearson Education, Inc. 4 Visceral peritoneum Intrinsic nerve plexuses • Myenteric nerve plexus • Submucosal nerve plexus Submucosal glands Mucosa • Surface epithelium • Lamina propria • Muscle layer Submucosa Muscularis externa • Longitudinal muscle layer • Circular muscle layer Serosa (visceral peritoneum) Nerve Gland in Lumen Artery mucosa Mesentery Vein Duct oF gland Lymphoid tissue outside alimentary canal © 2018 Pearson Education, Inc. 5 Diaphragm Falciform ligament Lesser Liver omentum Spleen Pancreas Gallbladder Stomach Duodenum Visceral peritoneum Transverse colon Greater omentum Mesenteries Parietal peritoneum Small intestine Peritoneal cavity Uterus Large intestine Cecum Rectum Anus Urinary bladder (a) (b) © 2018 Pearson Education, Inc. 6 Cardia Fundus Esophagus Muscularis Serosa externa • Longitudinal layer • Circular layer • Oblique layer Body Lesser Rugae curvature of Pylorus mucosa Greater curvature Duodenum Pyloric Pyloric sphincter antrum (a) (valve) © 2018 Pearson Education, Inc. 7 Fundus Body Rugae of mucosa Pyloric Pyloric (b) sphincter antrum © 2018 Pearson Education, Inc. -

Basic Histology (23 Questions): Oral Histology (16 Questions
Board Question Breakdown (Anatomic Sciences section) The Anatomic Sciences portion of part I of the Dental Board exams consists of 100 test items. They are broken up into the following distribution: Gross Anatomy (50 questions): Head - 28 questions broken down in this fashion: - Oral cavity - 6 questions - Extraoral structures - 12 questions - Osteology - 6 questions - TMJ and muscles of mastication - 4 questions Neck - 5 questions Upper Limb - 3 questions Thoracic cavity - 5 questions Abdominopelvic cavity - 2 questions Neuroanatomy (CNS, ANS +) - 7 questions Basic Histology (23 questions): Ultrastructure (cell organelles) - 4 questions Basic tissues - 4 questions Bone, cartilage & joints - 3 questions Lymphatic & circulatory systems - 3 questions Endocrine system - 2 questions Respiratory system - 1 question Gastrointestinal system - 3 questions Genitouirinary systems - (reproductive & urinary) 2 questions Integument - 1 question Oral Histology (16 questions): Tooth & supporting structures - 9 questions Soft oral tissues (including dentin) - 5 questions Temporomandibular joint - 2 questions Developmental Biology (11 questions): Osteogenesis (bone formation) - 2 questions Tooth development, eruption & movement - 4 questions General embryology - 2 questions 2 National Board Part 1: Review questions for histology/oral histology (Answers follow at the end) 1. Normally most of the circulating white blood cells are a. basophilic leukocytes b. monocytes c. lymphocytes d. eosinophilic leukocytes e. neutrophilic leukocytes 2. Blood platelets are products of a. osteoclasts b. basophils c. red blood cells d. plasma cells e. megakaryocytes 3. Bacteria are frequently ingested by a. neutrophilic leukocytes b. basophilic leukocytes c. mast cells d. small lymphocytes e. fibrocytes 4. It is believed that worn out red cells are normally destroyed in the spleen by a. neutrophils b. -

Opinion of Trustees Resolution of Dispute Case No
Opinion of Trustees Resolution of Dispute Case No. 88-122 Page 1 _____________________________________________________________________________ OPINION OF TRUSTEES _____________________________________________________________________________ In Re Complainant: Employee Respondent: Employer ROD Case No: 88-122 - October 3, 1989 Board of Trustees: Joseph P. Connors, Sr., Chairman; Paul R. Dean, Trustee; William Miller, Trustee; Donald E. Pierce, Jr., Trustee; Thomas H. Saggau, Trustee. Pursuant to Article IX of the United Mine Workers of America ("UMWA") 1950 Benefit Plan and Trust, and under the authority of an exemption granted by the United States Department of Labor, the Trustees have reviewed the facts and circumstances of this dispute concerning the provision of health benefits coverage for orthodontic treatment under the terms of the Employer Benefit Plan. Background Facts An oral surgeon states that the Employee's daughter began experiencing pain and popping in the right temporomandibular joint after being hit in the area of the right mandible during a fight in March 1985. She was treated by a physical therapist and had splint therapy to correct her temporomandibular joint problems for about six months. In August 1985, the Employee's daughter suffered a second injury to the right side of the head. She continued having pain and popping in the right temporomandibular joint, and surgery, an arthroplasty of the joint, was performed in December 1986. The Employer provided coverage for the physical therapy, the splint therapy and the surgery to correct her temporomandibular joint problems. In March 1988, an oral surgeon recommended orthodontic treatment to alleviate all of the Employee's daughter's symptoms. The Employee's daughter was examined by an orthodontist on May 10, 1988; he noted that she had reciprocal clicking in both temporomandibular joints, lack of proper chewing motion, limited mobility of the mandible, frequent headaches, and tenderness in the right jaw joint. -

Oral-Peripheral Examination
Oral-Peripheral Examination SCSD 632 Week 2 Phonological Disorders 3. General Cautions Relating to the Oral-Peripheral Examination a. Use your initial impressions of the child’s speech and facial characteristics to guide your examination. b. Remember that one facial or oral abnormality may be associated with others. c. If you suspect an abnormality in structure or function you may want to get a second opinion from a more experienced SLP or an SLP who specializes in craniofacial or motor-speech disorders before initiating referrals to other professionals. d. Remember that in the case of most “special” conditions, it is not your role to diagnose the condition; rather it is your responsibility to make appropriate referrals. e. Remember that in Canada you cannot usually refer directly to a specialist; be sensitive in your approach to the family doctor or referring physician. f. Be sensitive about how you present your results to parents, especially when you are recommending referrals to other professionals. The parents have the right to refuse the referral. g. An oral-peripheral examination is at least as important for your young patients as for your older patients. 1 Oral-Peripheral Examination | Oral and Facial Structure z Face z Lips z Teeth z Hard palate z Soft palate z Tongue When you perform an oral-peripheral examination what are you looking for when you examine each of the following structures? a. Facial Characteristics: overall expression and appearance, size, shape and overall symmetry of the head and facial structures b. Teeth: maxillary central incisors should extend just slightly over the mandibular central incisors; the lower canine tooth should be half-way between the upper lateral incisor and the upper canine tooth c. -

Pharyngeal Flap
Cincinnati Children’s Hospital Medical Center Craniofacial Center and VPI Clinic Pharyngeal Flap What is Velopharyngeal Insufficiency (VPI)? During normal speech, the soft palate (also called velum) raises and closes against the back wall of the throat (also called pharynx or pharyngeal wall). This closes off the nose from the mouth for speech. If the soft palate is not long enough to firmly close against the back of the throat during speech, sound and air can leak into the nose through the gap. This condition is called velopharyngeal insufficiency (VPI). VPI can affect resonance, which is the quality of the voice. The voice may sound hypernasal because there is too much sound in the nose during speech. (Hyponasality is the opposite problem. It is due to blockage in the nose and occurs when the person has a bad cold.) VPI can also affect speech sound production. The child may not have enough air pressure in the mouth to make certain speech sounds. Also, a leak of air through the nose may be heard during speech. To correct VPI for normal speech, the opening between the nose and mouth must be closed. The Furlow Z-plasty can correct VPI, particularly for children with a history of cleft palate or submucous cleft (where the muscles under the skin of the soft palate have not come together properly). Procedure: The pharyngeal flap is done by taking a flap of tissue from the back of the throat (pharyngeal wall) and attaching it to the soft palate (velum). This flap forms a “bridge” to close the gap between the back of the throat and the soft palate. -

AN OVERVIEW of VESICOBULLOUS CONDITIONS AFFECTING the ORAL MUCOSA EMMA HAYES, STEPHEN J CHALLACOMBE Prim Dent J
AN OVERVIEW OF VESICOBULLOUS CONDITIONS AFFECTING THE ORAL MUCOSA EMMA HAYES, STEPHEN J CHALLACOMBE Prim Dent J. 2016; 5(1):46-50 in the palate, buccal mucosa and labial ABSTRACT mucosa there is an underlying submucosa. The epithelium is formed of several layers, Vesicobullous diseases are characterised by the presence of vesicles or bullae at the deepest being the layer of progenitor varying locations in the mucosa. The most common occurring in the oral cavity cells forming the stratum germinativum, are mucous membrane pemphigoid (MMP) and pemphigus vulgaris (PV). Both adjacent to the lamina propria. are autoimmune diseases with a peak age onset of over 60 years and females Keratinocytes increase in size and flatten are more commonly affected than men. This paper reviews the structure of the as they move through the stratum spinosum oral mucosa, with specific reference to the basement membrane zone, as well and stratum granulosum to the stratum as bullous conditions affecting the mucosa, including PV and pemphigoid, their corneum (in keratinized mucosa) where the aetiology, clinical presentation, and management. desmosomes, which hold the cells together, weaken – therefore allowing normal Learning outcomes desquamation. • Understand the common presentation of vesicobullous diseases. • Appreciate the role of investigations in diagnosis and its interpretation. In addition to desmosomes, epithelial • Appreciate the roles of both primary and secondary care in patient management. cell-cell contact occurs via occludens (tight junctions), and nexus junctions (gap junctions), with each having a complex structure. Desmosomes are small adhesion Introduction proteins (0.2µm) 1 which guarantee the Vesicobullous diseases are characterised by integrity of the epidermis by linking the the presence of vesicles or bullae at varying intermediate filaments within cells to the locations in the mucosa. -

Albany Med Conditions and Treatments
Albany Med Conditions Revised 3/28/2018 and Treatments - Pediatric Pediatric Allergy and Immunology Conditions Treated Services Offered Visit Web Page Allergic rhinitis Allergen immunotherapy Anaphylaxis Bee sting testing Asthma Drug allergy testing Bee/venom sensitivity Drug desensitization Chronic sinusitis Environmental allergen skin testing Contact dermatitis Exhaled nitric oxide measurement Drug allergies Food skin testing Eczema Immunoglobulin therapy management Eosinophilic esophagitis Latex skin testing Food allergies Local anesthetic skin testing Non-HIV immune deficiency disorders Nasal endoscopy Urticaria/angioedema Newborn immune screening evaluation Oral food and drug challenges Other specialty drug testing Patch testing Penicillin skin testing Pulmonary function testing Pediatric Bariatric Surgery Conditions Treated Services Offered Visit Web Page Diabetes Gastric restrictive procedures Heart disease risk Laparoscopic surgery Hypertension Malabsorptive procedures Restrictions in physical activities, such as walking Open surgery Sleep apnea Pre-assesment Pediatric Cardiothoracic Surgery Conditions Treated Services Offered Visit Web Page Aortic valve stenosis Atrial septal defect repair Atrial septal defect (ASD Cardiac catheterization Cardiomyopathies Coarctation of the aorta repair Coarctation of the aorta Congenital heart surgery Congenital obstructed vessels and valves Fetal echocardiography Fetal dysrhythmias Hypoplastic left heart repair Patent ductus arteriosus Patent ductus arteriosus ligation Pulmonary artery stenosis -

Tongue-Ties and Sleep Issues (And More!) by Richard Baxter, DMD, MS, DABLS
LASERfocus Tongue-Ties and Sleep Issues (and More!) by Richard Baxter, DMD, MS, DABLS tongue-tie is a thick, tight, or short string of tissue under the tongue that restricts the tongue’s movement and causes a A functional issue. Collectively, tongue-ties and lip-ties are referred to as tethered oral tissues. They are often misdiagnosed or misunderstood, and they are quite common. The frequency with which anterior tongue-ties occur is estimated to range from 4-10% in the general population, and posterior tongue-ties have been reported in as many as 32.5% of infants in a recent study.1 flat palate, the baby is born with a high arched For a tight piece of tissue to qualify as a tongue-tie, it must have or “bubble” palate which leaves less room for a functional impact on nursing, speech, feeding, or sleep. Infant the base of the nose and less volume available problems arising from tongue-ties include painful and prolonged for the nasal cavity. Tongue-ties also lead to several of the main causes of breastfeeding nursing episodes, poor stimulation of maternal milk production, cessation, including nipple pain, trouble reflux, slow weight gain, gassiness, and a host of other issues for latching, and concerns that the baby is not mom and/or baby. As babies advance to eating solids, tongue- getting enough milk.3 It has been demon- strated in many controlled studies that releas- ties can lead to gagging, refusing food, spitting out food, and ing tongue-ties, whether classic near-the-tip picky eating. -

Bruce R. Maddern M.D., P.A. Post Frenuloplasty (Procedure to Resolve
Bruce R. Maddern M.D., P.A. Post Frenuloplasty (procedure to resolve “tongue-tie”) Instructions Ankyloglossia (“tongue-tie”) is a condition present from birth in which movement of the tongue tip is restricted due to an unusually short and/or thick frenulum. A frenulum is a band of tissue that anchors the tongue to the floor of the mouth behind the teeth. When the frenulum is too short or tight, the tongue tip is unable to move freely. This may result in difficulty with early bottle or breast-feeding or future speech articulation. The most common reason to perform frenuloplasty in a newborn is difficulty with feeding or latching. It is often possible to perform the procedure in office for infants under 6 months of age with a local anesthetic. The baby can feed immediately following the procedure. In toddlers it may be necessary to perform a frenuloplasty because of speech articulation issues. If a frenuloplasty is required for this age group the procedure occurs in the operating room under a brief general anesthesia. The entire procedure usually is complete with in 15 minutes. Speech therapy is necessary to ensure improved mobility of the tongue for older children. General risks from frenuloplasty include bleeding, pain, scarring, and infection. General Information • The patient may resume normal activity following surgery, including normal feeding schedule (bottle, breast, or soft food). • The patient may return to daycare the next day. • Some discomfort or tongue swelling is expected following this procedure. You may treat your child with Tylenol or Ibuprofen. • For infants the normal movements of the tongue during breast of bottle feeding is adequate stretching • Ice pops are a good way to numb the area.