Sleep Medicine: a Guide to Sleep and Its Ciated with Excessive Daytime Sleepiness
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Management of Chronic Insomnia Disorder and Obstructive Sleep
VA/DoD CLINICAL PRACTICE GUIDELINES The Management of Chronic Module A: Screening for Sleep Disorders Module B: Management of Chronic Insomnia Disorder Insomnia Disorder and 1 11 Adults with a provisional diagnosis of 15 Adult patient 14 Obstructive Sleep Apnea chronic insomnia disorder Refer to trained CBT-I or BBT-I Did the patient 2 provider, either in-person or using complete CBT-I or Sidebar 1: Clinical Features of OSA and Chronic Insomnia Disorder Does the patient, their bed 12 telehealth BBT-I? 3 OSA (see Appendix D in the full CPG for detailed ICSD -3 diagnostic criteria): partner, or their healthcare No Confirm diagnosis and then use SDM and encourage 20 Initiate short-term Yes • Sleepiness provider have complaints Exit algorithm behaviorally-based interventions for chronic insomnia No and/or concerns about the (i.e., CBT-I or BBT-I) (See Sidebar 3) pharmacotherapy • Loud, bothersome snoring patient’s sleep? treatment and/or CIH • Witnessed apneas 16 Yes 13 Was CBT-I or • Nightly gasping/choking 4 Is the patient ablea and willing Yes BBT-I 2 b • Obesity (BMI >30 kg/m ) Perform a clinical assessment, to complete CBT-I or BBT-I? 21 effective? Yes • Treatment resistant hypertension including use of validated screening No No Did insomnia remit after 17 Chronic Insomnia Disorder (see Appendix D in the full CPG for detailed tools (e.g., ISI and STOP 18 Is short-term pharmacotherapy Yes treatment with CIH or short- ICSD-3 diagnostic criteria): questionnaire) (See Sidebar 1) and/or CIH appropriate? (See Refer to sleep term pharmacotherapy with • Difficulty initiating sleep, difficulty maintaining sleep, or early -morning Sidebars 4 and 5) specialist for further no additional medication No assessment awakenings 6 No 5 19 required? • The sleep disturbance causes clinically significant distress or impairment in Are screening, history, Manage the important areas of functioning and/or physical exam No diagnosed sleep Reassess or reconsider behavioral treatments as needed. -

Diagnosis, Management and Pathophysiology of Central Sleep Apnea in Children ⇑ Anya T
Paediatric Respiratory Reviews 30 (2019) 49–57 Contents lists available at ScienceDirect Paediatric Respiratory Reviews Review Diagnosis, management and pathophysiology of central sleep apnea in children ⇑ Anya T. McLaren a, Saadoun Bin-Hasan b, Indra Narang a,c, a Division of Respiratory Medicine, The Hospital for Sick Children, 555 University Avenue, Toronto, ON M5G1X8, Canada b Department of Pediatrics, Division of Respiratory Medicine, Farwaniya Hospital, Kuwait c Faculty of Medicine, University of Toronto, Toronto, Ontario, Canada Educational aims The reader will be able to: Identify the different types of pediatric central sleep apnea (CSA) Describe the clinical presentation of CSA in children Discuss the pathophysiology of CSA Understand the evaluation of CSA in the pediatric population article info summary Keywords: Central sleep apnea (CSA) is thought to occur in about 1–5% of healthy children. CSA occurs more com- Central sleep apnea monly in children with underlying disease and the presence of CSA may influence the course of their dis- Sleep disordered breathing ease. CSA can be classified based on the presence or absence of hypercapnia as well as the underlying Hypoventilation condition it is associated with. The management of CSA needs to be tailored to the patient and may Children include medication, non-invasive ventilation, and surgical intervention. Screening children at high risk will allow for earlier diagnosis and timely therapeutic interventions for this population. The review will highlight the pathophysiology, prevalence and diagnosis of CSA in children. An algorithm for the manage- ment of CSA in healthy children and children with underlying co-morbidities will be outlined. Ó 2018 Elsevier Ltd. -

Sleep Bruxism and Sleep-Disordered Breathing
CRITICAL APPRAISAL Sleep Bruxism and Sleep-Disordered Breathing Author STEVEN D BENDER, DDS*, Associate Editor EDWARD J. SWIFT JR., DMD, MS ABSTRACT Sleep bruxism (SB) is a repetitive jaw muscle activity with clenching or grinding of the teeth during sleep. SB is characterized by what is known as rhythmic masticatory muscle activity (RMMA). RMMA is the laboratory polysomnographic finding that differentiates SB from other oromandibular movements seen during sleep. Most often RMMA episodes are associated with sleep arousal. Some patients will report similar complaints related to both SB and sleep disordered breathing (SDB). There are some reports that would suggest that SB is a result of SDB. It has has been postulated that SB is a compensatory mechanism to re establish muscle tone of the upper airway. While these disorders do in fact often present concomitantly, the relationship between the two is yet to be fully elucidated. This Critical Appraisal reviews 3 recent publications with the intent to better define what relationships may exists between SDB and SB. While the current evidence appears to support the notion that these are often concomitant disorders, it also makes clear that evidence to support the hypothesis that SDB is causative for SB is currently lacking. (J Esthet Restor Dent 00:000–000, 2016) Sleep Bruxismin Patients with Sleep-disordered Breathing T.T. SJOHOLM,€ A.A. LOWE, K. MIYAMOTO, A. FLEETHAM, C.F. RYAN Archives of Oral Biology 2000 (45:889–96) ABSTRACT index of more than five per hour of sleep were excluded. Sleep breathing parameters were measured Objective: The primary objective was to determine the using polysomnagraphic (PSG) recordings. -

Sleep Apnea Sleep Apnea
Health and Safety Guidelines 1 Sleep Apnea Sleep Apnea Normally while sleeping, air is moved at a regular rhythm through the throat and in and out the lungs. When someone has sleep apnea, air movement becomes decreased or stops altogether. Sleep apnea can affect long term health. Types of sleep apnea: 1. Obstructive sleep apnea (narrowing or closure of the throat during sleep) which is seen most commonly, and, 2. Central sleep apnea (the brain is causing a change in breathing control and rhythm) Obstructive sleep apnea (OSA) About 25% of all adults are at risk for sleep apnea of some degree. Men are more commonly affected than women. Other risk factors include: 1. Middle and older age 2. Being overweight 3. Having a small mouth and throat Down syndrome Because of soft tissue and skeletal alterations that lead to upper airway obstruction, people with Down syndrome have an increased risk of obstructive sleep apnea. Statistics show that obstructive sleep apnea occurs in at least 30 to 75% of people with Down syndrome, including those who are not obese. In over half of person’s with Down syndrome whose parents reported no sleep problems, sleep studies showed abnormal results. Sleep apnea causing lowered oxygen levels often contributes to mental impairment. How does obstructive sleep apnea occur? The throat is surrounded by muscles that are active controlling the airway during talking, swallowing and breathing. During sleep, these muscles are much less active. They can fall back into the throat, causing narrowing. In most people this doesn’t affect breathing. However in some the narrowing can cause snoring. -

Obstructive Sleep Apnea Obstructive Sleep Apnea (OSA) Is a Condition That Develops Due to Blockage of the Ability to Breathe During Sleep
Snoring and Obstructive Sleep Apnea Obstructive sleep apnea (OSA) is a condition that develops due to blockage of the ability to breathe during sleep. Snoring is the most prevalent sign of sleep apnea, but it is not present in everyone with OSA. Patients with mild obstruction may not receive a diagnosis of OSA, but snoring may be a severe problem in those patients. When the obstruction is more sever, the patient may be diagnosed with OSA. Treatment is needed for OSA for several reasons. Symptoms of OSA include snoring, bedwetting (in children), morning headaches, high blood pressure, excessive sleepiness during the day. In general, the more severe the sleep apnea is, the worse the symptoms are. If you or your loved one tends to wake others up with their snoring, you should be evaluated. Evaluation of OSA is done by a test called a polysomnography, otherwise known as a sleep study. Basically, the patient goes to a sleep lab to spend a few hours sleeping. Monitors are attached to monitor breathing, loudness of snoring, oxygen levels in the blood, heart rate, and many other parameters. The results of the test are studied to see how severe the problem is. Treatment is needed for OSA for several reasons. Most immediately, it helps people feel better with less daytime sleepiness. This is especially important in those who operate heavy machinery, eg. truck drivers, crane operators, etc.. Furthermore, long term sleep apnea can result in heart problems, stroke, and uncontrolled hypertension. Treatment of OSA can help to prevent these problems. Treatment for this disorder can involve surgery, but the surgery is very painful and long term results can be disappointing. -

Obstructive Sleep Apnea in Adults? NORMAL AIRWAY OBSTRUCTED AIRWAY
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES What Is Obstructive Sleep Apnea in Adults? NORMAL AIRWAY OBSTRUCTED AIRWAY Obstructive sleep apnea (OSA) is a common problem that affects a person’s breathing during sleep. A person with OSA has times during sleep in which air cannot flow normally into the lungs. The block in CPAP DEVICE airflow (obstruction) is usually caused by the collapse of the soft tissues in the back of the throat (upper airway) and tongue during sleep. Apnea means not breathing. In OSA, you may stop ■■ Gasping breathing for short periods of time. Even when you are or choking trying to breathe, there may be little or no airflow into sounds. the lungs. These pauses in airflow (obstructive apneas) ■■ Breathing pauses observed by someone watching can occur off and on during sleep, and cause you to you sleep. wake up from a sound sleep. Frequent apneas can cause ■■ Sudden or jerky body movements. many problems. With time, if not treated, serious health ■■ Restless tossing and turning. problems may develop. ■■ Frequent awakenings from sleep. OSA is more common in men, women after menopause CLIP AND COPY AND CLIP Common symptoms you may have while awake: and people who are over the age of 65. OSA can also ■■ Wake up feeling like you have not had enough sleep, occur in children. Also see ATS Patient Information Series even after sleeping many hours. fact sheet on OSA in Children. People who are at higher ■■ Morning headache. risk of developing sleep apnea include those with: ■■ Dry or sore throat in the morning from breathing ■■ enlarged tonsils and/or adenoids through your mouth during sleep. -

Sleep Apnea Facts and Figures
Sleep Apnea Facts and Figures What is sleep-disordered breathing (SDB)? Classification of sleep apnea SDB describes a number of breathing disorders Apnea–hypopnea index (AHI) that occur during sleep ■■ Number of apneas and/or hypopneas per hour of sleep (or study time) ■■ Obstructive sleep apnea (OSA) ■■ Reflects the severity of sleep apnea ■■ Central sleep apnea (CSA) AHI = 0–5 Normal range ■■ Nocturnal hypoventilation AHI = 5–15 Mild sleep apnea ■■ Cheyne–Stokes respiration (CSR) AHI = 15–30 Moderate sleep apnea AHI > 30 Severe sleep apnea What is obstructive sleep apnea (OSA)? ■■ A partial or complete collapse of the upper airway caused by Prevalence of sleep apnea relaxation of the muscles controlling the soft palate and tongue ■■ Approximately 42 million American adults have SDB1 ■■ Person experiences apneas, hypopneas and flow limitation ■■ 1 in 5 adults has mild OSA2 —■ Apnea: a cessation of airflow for ≥10 seconds ■■ 1 in 15 has moderate to severe OSA2 —■ Hypopnea: a decrease in airflow lasting ≥10 seconds ■■ 9% of middle-aged women and 25% of middle-aged men with a 30% oxygen reduction in airflow and with at least suffer from OSA3 a 4% oxygen desaturation from baseline ■■ Prevalence similar to asthma (20 million) and diabetes —■ Flow limitation: narrowing of the upper airway and an (23.6 million) of US population4 indication of an impending upper airway closure ■■ 75% of severe SDB cases remain undiagnosed5 Prevalence of Sleep Apnea in Comorbidities Drug-Resistant Hypertension 83% 6 Obesity 77% 7 Congestive Heart Failure 76% 8 -

Sleep Review of Systems ISNORED.Qxd
SLEEP REVIEW OF SYSTEMS “ISNORED” Incorporate a Sleep Review of Systems into your General Review O—OLDER (see SNORING above) or OBESE. of Systems. It' s easy to remember the phrase: "I SNORED." (Modified from I SNORED by Edward F. Haponik, M.D., Wake R—RESTORATIVE or REFRESHING SLEEP. Normal per- Forest University School of Medicine) sons who have adequate sleep time in awakening feeling refreshed with a high energy level. Sleep has many functions including I - Insomnia memory consolidation, tissue repair, and many other physiologi- S - Snoring and Sleep Quality cal consequences. Many of the more than 88 sleep disorders may N - Not Breathing result in non-restorative sleep because of multiple nocturnal O - Older or Obese awakenings or disruption of the normal sleep architecture. R - Restorative or Refreshing Sleep E - Excessive Daytime Sleepiness E—EXCESSIVE DAYTIME SLEEPINESS. Excessive day- D - Drugs or Alcohol time sleepiness is when people have the strong urge to sleep dur- ing inappropriate times or even drift into sleep. Patients report "I SNORED" will help you to remember to ask about sleep dis- falling asleep doing inactive tasks such as reading or watching tel- orders in your practice. Sleep disorders afflict millions of evision. There are subjective measures of daytime sleepiness Americans and remain undiagnosed in a significant number of including the Epworth Sleepiness Scale, Stanford Sleepiness individuals, partially because their physicians don't inquire about Scale, and a Linear Analog Scale. It's important to ask whether sleep problems or excessive daytime sleepiness. the patient falls asleep while driving since this may lead to mor- bidity and mortality and patients should be instructed to refrain I—INSOMNIA is very common, and a recent Gallup Poll from driving their sleep disorder is diagnosed and adequately showed that 9% of respondents had chronic insomnia and 27% treated. -

Obesity Hypoventilation Syndrome: a State-Of-The-Art Review
Obesity Hypoventilation Syndrome: A State-of-the-Art Review Babak Mokhlesi MD MSc Historical Perspective Definition Epidemiology Clinical Presentation and Diagnosis Morbidity and Mortality Quality of Life Morbidity Mortality Pathophysiology The Excessive Load on the Respiratory System Blunted Central Respiratory Drive Predictors of Hypercapnia in Obese Patients With OSA Treatment Treatment of Sleep-Disordered Breathing Surgical Interventions Pharmacologic Respiratory Stimulation Summary Obesity hyoventilation syndrome (OHS) is defined as the triad of obesity, daytime hypoventilation, and sleep-disordered breathing in the absence of an alternative neuromuscular, mechanical or metabolic explanation for hypoventilation. During the last 3 decades the prevalence of extreme obesity has markedly increased in the United States and other countries. With such a global epidemic of obesity, the prevalence of OHS is bound to increase. Patients with OHS have a lower quality of life, with increased healthcare expenses, and are at higher risk of developing pulmonary hypertension and early mortality, compared to eucapnic patients with sleep-disordered breathing. OHS often remains undiagnosed until late in the course of the disease. Early recognition is impor- tant, as these patients have significant morbidity and mortality. Effective treatment can lead to significant improvement in patient outcomes, underscoring the importance of early diagnosis. This review will include disease definition and epidemiology, clinical characteristics of the syndrome, pathophysiology, and morbidity and mortality associated with it. Lastly, treatment modalities will be discussed in detail. Key words: obesity hypoventilation syndrome; Pickwickian syndrome; hypercap- nia; hypoventilation; sleep apnea; sleep-disordered breathing; CPAP; bi-level PAP. [Respir Care 2010; 55(10):1347–1362. © 2010 Daedalus Enterprises] Babak Mokhlesi MD MSc is affiliated with the Section of Pulmonary and Dr Mokhlesi has disclosed a relationship with Philips/Respironics. -

Clinical Guide for Sleep Specialists: Diagnosing Narcolepsy
CLINICIAN GUIDE 1 This brochure can help you: Table of Contents RECOGNIZE Narcolepsy Overview..................................................................... 4 possible manifestations of excessive daytime sleepiness, Narcolepsy Symptoms.................................................................... 5 1-3 the cardinal symptom of narcolepsy Pathophysiology of Narcolepsy.................................................. 6 SCREEN Neurobiology of Normal Wakefulness...................................... 6 all patients with manifestations of excessive daytime sleepiness Pathophysiology of Narcolepsy................................................... 6 for narcolepsy using validated screening tools4-7 Recognizing Potential Narcolepsy Patients............................. 8 DIAGNOSE Recognizing Excessive Daytime Sleepiness........................... 8 narcolepsy through a complete clinical interview Recognizing Cataplexy................................................................... 9 and sleep laboratory testing1 Screening Your Patients................................................................ 10 Epworth Sleepiness Scale.............................................................. 10 Swiss Narcolepsy Scale...................................................................11 Diagnosing Narcolepsy..................................................................12 Clinical Interview............................................................................... 12 Sleep Laboratory Testing.............................................................. -

Co-Morbid Insomnia and Sleep Apnea (COMISA): Prevalence, Consequences, Methodological Considerations, and Recent Randomized Controlled Trials
brain sciences Review Co-Morbid Insomnia and Sleep Apnea (COMISA): Prevalence, Consequences, Methodological Considerations, and Recent Randomized Controlled Trials Alexander Sweetman 1,* , Leon Lack 2 and Célyne Bastien 3 1 The Adelaide Institute for Sleep Health: A Flinders Centre of Research Excellence, Box 6 Mark Oliphant Building, 5 Laffer Drive, Bedford Park, Flinders University, Adelaide 5042, South Australia, Australia 2 The Adelaide Institute for Sleep Health: A Flinders Centre of Research Excellence, College of Education Psychology and Social Work, Flinders University, Adelaide 5042, South Australia, Australia; leon.lack@flinders.edu.au 3 School of Psychology, Félix-Antoine-Savard Pavilion, 2325, rue des Bibliothèques, local 1012, Laval University, Quebec City, QC G1V 0A6, Canada; [email protected] * Correspondence: alexander.sweetman@flinders.edu.au; Tel.: +61-8-7421-9908 Received: 15 November 2019; Accepted: 10 December 2019; Published: 12 December 2019 Abstract: Co-morbid insomnia and sleep apnea (COMISA) is a highly prevalent and debilitating disorder, which results in additive impairments to patients’ sleep, daytime functioning, and quality of life, and complex diagnostic and treatment decisions for clinicians. Although the presence of COMISA was first recognized by Christian Guilleminault and colleagues in 1973, it received very little research attention for almost three decades, until the publication of two articles in 1999 and 2001 which collectively reported a 30%–50% co-morbid prevalence rate, and re-ignited research interest in the field. Since 1999, there has been an exponential increase in research documenting the high prevalence, common characteristics, treatment complexities, and bi-directional relationships of COMISA. Recent trials indicate that co-morbid insomnia symptoms may be treated with cognitive and behavioral therapy for insomnia, to increase acceptance and use of continuous positive airway pressure therapy. -
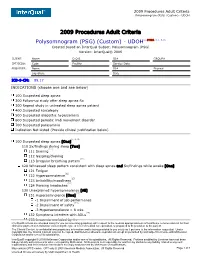
Polysomnogram (PSG) (Custom) - UDOH
2009 Procedures Adult Criteria Polysomnogram (PSG) (Custom) - UDOH 2009 Procedures Adult Criteria Polysomnogram (PSG) (Custom) - UDOH(1, 2*MDR, 3, 4, 5, 6) Created based on InterQual Subset: Polysomnogram (PSG) Version: InterQual® 2009 CLIENT: Name D.O.B. ID# GROUP# CPT/ICD9: Code Facility Service Date PROVIDER: Name ID# Phone# Signature Date ICD-9-CM: 89.17 INDICATIONS (choose one and see below) 100 Suspected sleep apnea 200 Follow-up study after sleep apnea Rx 300 Repeat study in untreated sleep apnea patient 400 Suspected narcolepsy 500 Suspected idiopathic hypersomnia 600 Suspected periodic limb movement disorder 700 Suspected parasomnia Indication Not Listed (Provide clinical justification below) (7, 8, 9) 100 Suspected sleep apnea [One] 110 Sx/findings during sleep [Two] (10) 111 Snoring 112 Gasping/choking (11) 113 Irregular breathing pattern 120 Witnessed sleep pattern consistent with sleep apnea and Sx/findings while awake [One] 121 Fatigue (12) 122 Hypersomnolence (13) 123 Irritability/moodiness (14) 124 Morning headaches 130 Unexplained hypersomnolence [All] (12) 131 Hypersomnolence [One] -1 Impairment of job performance (15) -2 Impairment of safety -3 Hypersomnolence > 8 wks (16) 132 Symptoms interfere with ADLs 133 Insomnia excluded by Hx InterQual® criteria are intended solely for use as screening guidelines with respect to the medical appropriateness of healthcare services and not for final clinical or payment determination concerning the type or level of medical care provided, or proposed to be provided, to the patient. The Clinical Content is confidential and proprietary information and is being provided to you solely as it pertains to the information requested. Under copyright law, the Clinical Content may not be copied, distributed or otherwise reproduced except as permitted by and subject to license with McKesson Corporation and/or one of its subsidiaries.