Safety Manual Program/Monthly Safety Awearness
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Motion Sickness: Definition
Clinical and physiological characteristics of cybersickness Submitted in fulfilment of the requirements for the degree of Doctor of Philosophy (Human Physiology) School of Biomedical Sciences and Pharmacy Faculty of Health and Medicine University of Newcastle, Australia This research was supported by an Australian Government Research Training Program (RTP) Scholarship. 1 STATEMENT OF ORIGINALITY I hereby certify that the work embodied in the thesis is my own work, conducted under normal supervision. The thesis contains no material which has been accepted, or is being examined, for the award of any other degree or diploma in any university or other tertiary institution and, to the best of my knowledge and belief, contains no material previously published or written by another person, except where due reference has been made. I give consent to the final version of my thesis being made available worldwide when deposited in the University’s Digital Repository, subject to the provisions of the Copyright Act 1968 and any approved embargo. Alireza Mazloumi Gavgani 2 ACKNOWLEDGMENT OF AUTHORSHIP I hereby certify that the work embodied in this thesis contains published paper/s/scholarly work of which I am a joint author. I have included as part of the thesis a written declaration endorsed in writing by my supervisor, attesting to my contribution to the joint publication/s/scholarly work. Alireza Mazloumi Gavgani 3 STATEMENT OF COLLABORATION I hereby certify that some parts of the work embodied in this thesis have been done in collaboration with other researchers. I have included as part of the thesis a statement clearly outlining the extent of collaboration, with whom and under what auspices. -

ANZHMG) & the Hyperbaric Technicians and Nurses Association (HTNA)
The Australian and New Zealand Hyperbaric Medicine Group (ANZHMG) & The Hyperbaric Technicians and Nurses Association (HTNA) COVID-19 Guidelines 1 | ANZHMG/HTNA COVID - 19 v1.1 2020 - 03- 27 Published by the South Pacific Underwater Medicine Society (SPUMS), c/- Australian and New Zealand College of Anaesthetists (ANZCA), 630 St Kilda Road, Melbourne VIC 3004, Australia. E-mail: [email protected] Website: spums.org.au This document is based upon the Australian and New Zealand Intensive Care Society (2020) ANZICS COVID-19 Guidelines. Melbourne: ANZICS, with permission. THE ANZHMG/HTNA COVID-19 Working Group gratefully acknowledge the kindness of the Australian & New Zealand Intensive Care Society in permitting the use of their guidelines as a template for our own. © Australian and New Zealand Hyperbaric Medicine Group 2020. Not for sale. This work may be reproduced, free of charge, in whole or in part for clinical, study, training, research or any other fair purpose, subject to the inclusion of an acknowledgment of the source. SPUMS requests that you attribute this publication (and any material sourced from it) using the following citation: Australian and New Zealand Hyperbaric Medicine Group and the Hyperbaric Technicians and Nurses Association (2020), ANZHMG/HTNA COVID-19 Guidelines. Melbourne: SPUMS. Disclaimer The Australian and New Zealand Hyperbaric Medicine Group (ANZHMG) and Hyperbaric Technicians and Nurses Association (HTNA) COVID-19 Guidelines have been developed to assist hyperbaric clinicians prepare and plan for the maintenance of hyperbaric services during a pandemic, and provide a safe working environment for staff and patients. Considerable effort has been made to ensure the information contained within the recommendations is correct at the time of publication. -

Nursing in a Critical Care Hyperbaric Unit at Merida, Yucatan, Mexico: Report of a Case of an Acute Pediatric Burn Patient
Case Report Page 1 of 6 Nursing in a critical care hyperbaric unit at Merida, Yucatan, Mexico: report of a case of an acute pediatric burn patient Judith Ruiz-Aguilar, Rodrigo Diaz-Ibañez, E. Cuauhtemoc Sanchez-Rodriguez Hyperbaric Medicine Service, Hospital Centro de Especialidades Médicas del Sureste (CEM) and Hospital Agustín O’Horan, Merida, Yucatan, Mexico Correspondence to: Judith Ruiz-Aguilar, RN, MEd. Chief of Nursing, Hyperbaric Medicine Service, Hospital Centro de Especialidades Médicas del Sureste (CEM) and Hospital Agustín O’Horan, Merida, Yucatan, Mexico. Email: [email protected]. Abstract: Hyperbaric oxygen therapy (HBOT) for intensive care unit (ICU) patients places special technical and knowledge-based skills demands on nurses inside hyperbaric chambers. Probably the best clinical contributions of HBOT are in the acute cases, in the ischemia reperfusion injury. Nevertheless in the last years, hyperbaric units have focused more in chronic wounds. The first golden rule to treat an ICU patient in a hyperbaric chamber is that you can maintain the same quality of care inside the chamber as in the ICU. This means that the hyperbaric unit has to have the technology means as well as the proficiency and competency of its personnel to provide intensive care inside the chamber. These require competent nursing personnel. We present a case of a 5-year-old pediatric patient who suffered a deep second-degree thermal burn that compromised 32% of the total body surface; including the face, neck, thorax and both arms. The patient received medical support, HBOT and daily wound care. He received a total of 14 treatments and underwent complete healing of the burned areas. -

Safety Manual Program/Monthly Safety Awearness
2014 Safety Manual/Monthly Safety Awareness Program Serena Group Hyperbaric Medicine Centers Page 1 Confidential and Proprietary Information SerenaGroup Hyperbaric Medical Center Do not copy or distribute 2014 Fire Safety Plan 1. Purpose To provide hyperbaric personnel a predetermined plan in the event of a fire in the hyperbaric area in order to reduce injury and/or catastrophic outcomes. 2. Policy 2.1. In the event of an emergency, the Hyperbaric Medicine Center personnel will be prepared to respond. 2.2. The Safety Director shall be designated by the Program Director / Manager or designee. NOTE: NFPA 99 Health Care Facilities, 1999 edition, (page 131) “19-3.1.3.2 A safety director shall be designated in charge of all hyperbaric equipment. The safety director shall work closely with facility management personnel and the hyperbaric physician(s) to establish procedures for safe operation and maintenance of the hyperbaric facility. He or she shall make necessary recommendations for departmental safety policies and procedures. The safety director shall have the authority to restrict or remove any potentially hazardous supply or equipment items from the chamber.” 2.3. Each plan shall be collaboratively developed with the hospital fire safety policy in conjunction with NFPA standards. 2.4. There will be no smoking or open flames in the hyperbaric area. 2.5. The area will be kept exceptionally clean and free of fire hazards according to the NGPA for Hyperbaric health care facilities. 2.6. The chamber itself will be kept exceptionally clean of lint and dust particles as these are hazardous when inside the chamber. -

(ANZHMG) & the Hyperbaric Technicians and Nurses Association
The Australian and New Zealand Hyperbaric Medicine Group (ANZHMG) & The Hyperbaric Technicians and Nurses Association (HTNA) COVID-19 Guidelines 1 | ANZHMG/HTNA COVID - 19 v1.1 2020 - 03- 27 Published by the South Pacific Underwater Medicine Society (SPUMS), c/- Australian and New Zealand College of Anaesthetists (ANZCA), 630 St Kilda Road, Melbourne VIC 3004, Australia. E-mail: [email protected] Website: spums.org.au This document is based upon the Australian and New Zealand Intensive Care Society (2020) ANZICS COVID-19 Guidelines. Melbourne: ANZICS, with permission. THE ANZHMG/HTNA COVID-19 Working Group gratefully acknowledge the kindness of the Australian & New Zealand Intensive Care Society in permitting the use of their guidelines as a template for our own. © Australian and New Zealand Hyperbaric Medicine Group 2020. Not for sale. This work may be reproduced, free of charge, in whole or in part for clinical, study, training, research or any other fair purpose, subject to the inclusion of an acknowledgment of the source. SPUMS requests that you attribute this publication (and any material sourced from it) using the following citation: Australian and New Zealand Hyperbaric Medicine Group and the Hyperbaric Technicians and Nurses Association (2020), ANZHMG/HTNA COVID-19 Guidelines. Melbourne: SPUMS. Disclaimer The Australian and New Zealand Hyperbaric Medicine Group (ANZHMG) and Hyperbaric Technicians and Nurses Association (HTNA) COVID-19 Guidelines have been developed to assist hyperbaric clinicians prepare and plan for the maintenance of hyperbaric services during a pandemic, and provide a safe working environment for staff and patients. Considerable effort has been made to ensure the information contained within the recommendations is correct at the time of publication. -

June 18-20, 2015 Annual Scientific Meeting
UNDERSEA & HYPERBARIC MEDICAL SOCIETY ANNUAL SCIENTIFIC MEETING HOTEL BONAVENTURE MONTREAL, CANADA JUNE 18-20, 2015 2015 UHMS Scientific Meeting June 18-20 Montreal, Canada TABLE OF CONTENTS Subject Page No. Disclosures ................................................................................................................................................................ 6-7 Schedule .................................................................................................................................................................. 8-13 Continuing Education ................................................................................................................................................ 13 Associates’ Breakout Schedule .................................................................................................................................. 14 Evaluation / MOC Credit Information ....................................................................................................................... 15 Committee Meetings .................................................................................................................................................. 16 Exhibitors .............................................................................................................................................................. 17-20 SESSIONS/ABSTRACTS THURSDAY GENERAL SESSION .............................................................................................................. 22-63 PRESIDENT’S -

The Kent Hospital Wound Recovery and Hyperbaric Medicine Center: a Brief Overview, 1998–2013
CONTRIBUTION The Kent Hospital Wound Recovery and Hyperbaric Medicine Center: A Brief Overview, 1998–2013 LISA J. GOULD, MD, PhD; CATHERINE DECIANTIS, RN, CHRN; RONALD P. ZINNO, MD; GEORGE A. PERDRIZET, MD, PhD 13 17 EN ABSTRACT cannot devote the necessary time and effort required in the A brief description of the Wound Recovery and Hyperbaric management of these patients. Wound centers add value to Medicine Center, now in its second decade of service, the institutions and communities in which they serve. will inform the general medical community of this As the field has expanded, the science of chronic wound valuable asset. care has also grown. The increased utilization of hyperbaric Demand for wound care services is predicted to grow oxygen therapy (HBOT) is one example of this new growth. steadily over the next several decades. Kent Hospital’s vi- Approximately 10-15% of patients presenting to wound care sion for wound care is embodied in its thriving Wound centers will qualify for HBOT. Oxygen deficiency is a criti- Recovery and Hyperbaric Medicine Center. New cost- cal component of many wound types for which HBOT may effective wound healing therapies must be developed provide the cure or substantially boost other healing inter- and evidence-based practices established. New physi- ventions. Under the direction of Dr. Stephen Cummings, cians and support staff must be trained. Only through a Kent Hospital acquired three hyperbaric chambers in March blending of high quality clinical care with research and 2002, prompting a name change to the Kent Wound Recov- education will these objectives be achieved and future ery and Hyperbaric Medicine Center (KWRHMC) (Figure 1). -

Hyperthermia & Heat Stroke: Heat-Related Conditions
Hyperthermia & Heat Stroke: Heat-Related Conditions Joseph Rampulla, MS, APRN,BC eat-related conditions occur when excess heat taxes or overwhelms the body’s thermoregulatory mechanisms. Heat illness is preventable and occurs more Hcommonly than most clinicians realize. Heat illness most seriously affects the poor, urban-dwellers, young children, those with chronic physical and mental illnesses, substance abusers, the elderly, and people who engage in excessive physical The exposure to activity under harsh conditions. While considerable overlap occurs, the important the heat and the concrete during the syndromes are: heat stroke, heat exhaustion, and heat cramps. Heat stroke is a life- hot summer months places many rough threatening emergency and occurs when the loss of thermoregulatory control results sleepers at great risk in hyperpyrexia (very high fever) and severe damage to many internal organs. for heat stroke and hyperthermia. Photo by Epidemiology Sharon Morrison RN Heat illness is generally underreported, and the deaths than all other natural disasters combined in true incidence is unknown. Death rates from other the USA. The elderly, the very poor, and socially causes (e.g. cardiovascular, respiratory) increase isolated individuals are disproportionately affected during heat waves but are generally not reflected in by heat waves. For example, death records during the morbidity and mortality statistics related to heat heat waves invariably include many elders who died illness. Nonetheless, heat waves account for more alone in hot apartments. Age 65 years, chronic The Health Care of Homeless Persons - Part II - Hyperthermia and Heat Stroke 199 illness, and residence in a poor neighborhood are greater than 65. -

Hypothermia Hyperthermia Normothemic
Means normal body temperature. Normal body core temperature ranges from 99.7ºF to 99.5ºF. A fever is a Normothemic body temperature of 99.5 to 100.9ºF and above. Humans are warm-blooded mammals who maintain a constant body temperature (euthermia). Temperature regulation is controlled by the hypothalamus in the base of the brain. The hypothalamus functions as a thermostat for the body. Temperature receptors (thermoreceptors) are located in the skin, certain mucous membranes, and in the deeper tissues of the body. When an increase in body temperature is detected, the hypothalamus shuts off body mechanisms that generate heat (for example, shivering). When a decrease in body temperature is detected, the hypothalamus shuts off body mechanisms designed to cool the body (for example, sweating). The body continuously adjusts the metabolic rate in order to maintain a constant CORE Hypothermia Core body temperatures of 95ºF and lower is considered hypothermic can cause the heart and nervous system to begin to malfunction and can, in many instances, lead to severe heart, respiratory and other problems that can result in organ damage and death.Hannibal lost nearly half of his troops while crossing the Pyrenees Alps in 218 B.C. from hypothermia; and only 4,000 of Napoleon Bonaparte’s 100,000 men survived the march back from Russia in the winter of 1812 - most dying of starvation and hypothermia. During the sinking of the Titanic most people who entered the 28°F water died within 15–30 minutes. Symptoms: First Aid : Mild hypothermia: As the body temperature drops below 97°F there is Call 911 or emergency medical assistance. -

Malignant Hyperthermia.Pdf
Malignant Hyperthermia Matthew Alcusky PharmD, MS Student University of Rhode Island July, 2013 Financial Disclosure I have no financial obligations to disclose. Outline • Introduce malignant hyperthermia including its causes and implications • Describe the underlying pathophysiology • Detail the clinical presentation of MH • Summarize the necessary pharmacological and non-pharmacological treatment of MH • Highlight necessary considerations with the use of dantrolene • Discuss recrudescence Malignant Hyperthermia • A life threatening reaction that is most often triggered by the use of inhalational anesthetics • Estimated incidence of 1 in 5,000 to 1 in 100,000 anesthesia inductions • Early recognition and treatment is essential in reducing morbidity and mortality • Screening patients for past anesthesia history and family history, as well as conducting testing on at risk individuals is necessary to reduce MH occurrence Rosenberg H, Davis M, James D, Pollock N, Stowell K. Malignant hyperthermia. Orphanet J Rare Dis. 2007 Apr 24;2:21. Review. Drugs Triggering Malignant Hyperthermia • Desflurane • Succinylcholine- • Enflurane only non-inhalational • Halothane anesthetic that triggers MH • Isoflurane • Nitrous Oxide- only • Methoxyflurane inhalational anesthetic • Sevoflurane that does not cause MH Hopkins PM. Malignant hyperthermia: pharmacology of triggering. Br J Anaesth. 2011 Jul;107(1):48-56. doi: 10.1093/bja/aer132. Epub 2011 May 30. Review. Pathophysiology • MH partially attributed to a dominant mutation in the ryanodine receptror 1 (RYR1) – Ryanodine receptors are activated by elevated Ca2+ levels, known as store overload induced calcium release (SOICR) – Mutant receptors are activated by lower Ca2+ levels – Volatile anesthetics further lower the SOICR threshold MacLennan DH, Chen SR. Store overload-induced Ca2mutations + release as a triggering mechanism for CPVT and MH episodes caused by in RYR and CASQ genes. -

Guidelines for Management of a Malignant Hyperthermia (MH) Crisis
Guidelines for the management of a Malignant Hyperthermia Crisis Successful treatment of a Malignant Hyperthermia (MH) crisis depends on early diagnosis and aggressive treatment. The onset of a reaction can be within minutes of induction or may be more insidious. Previous uneventful anaesthesia does not exclude MH. The steps below are intended as an aide memoire. Presentation may vary and treatment should be modified accordingly. Know where the dantrolene is stored in your theatre. Treatment can be optimised by teamwork. Call for help Diagnosis - consider MH if: 1 1. Unexplained, unexpected increase in end-tidal CO2 together with 2. Unexplained, unexpected tachycardia together with 3. Unexplained, unexpected increased in oxygen consumption Masseter muscle spasm, and especially more generalised muscle rigidity after suxamethonium, indicate a high risk of MH susceptibility but are usually self-limiting. Take measures to halt the MH process: 2 1. Remove trigger drugs, turn off vaporisers, use high fresh gas flows (oxygen), use a new, clean non-rebreathing circuit, hyperventilate. Maintain anaesthesia with intravenous agents such as propofol until surgery completed. 2. Dantrolene; give 2-3 mg.kg-1 i.v. initially and then 1 mg.kg-1 PRN. 3. Use active body cooling but avoid vasoconstriction. Convert active warming devices to active cooling, give cold 3 intravenous infusions, cold peritoneal lavage, extracorporeal heat exchange. Monitor: 4 ECG, SpO2, end-tidal CO2, invasive arterial BP, CVP, core and peripheral temperature, urine output and pH, arterial blood gases, potassium, haematocrit, platelets, clotting indices, creatine kinase (peaks at 12-24h). Treat the effects of MH: 5 1. Hypoxaemia and acidosis: 100% O2, hyperventilate, sodium bicarbonate. -
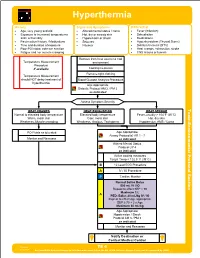
TE 04 Hyperthermia Protocol Final 2017 Editable.Pdf
Hyperthermia History Signs and Symptoms Differential • Age, very young and old • Altered mental status / coma • Fever (Infection) • Exposure to increased temperatures • Hot, dry or sweaty skin • Dehydration and / or humidity • Hypotension or shock • Medications • Past medical history / Medications • Seizures • Hyperthyroidism (Thyroid Storm) • Time and duration of exposure • Nausea • Delirium tremens (DT's) • Poor PO intake, extreme exertion • Heat cramps, exhaustion, stroke • Fatigue and / or muscle cramping • CNS lesions or tumors Remove from heat source to cool Temperature Measurement environment Procedure if available Cooling measures Remove tight clothing Temperature Measurement should NOT delay treatment of Blood Glucose Analysis Procedure hyperthermia Age Appropriate Diabetic Protocol AM 2 / PM 2 as indicated Assess Symptom Severity Toxic HEAT CRAMPS HEAT EXHAUSTION HEAT STROKE Normal to elevated body temperature Elevated body temperature Fever, usually > 104°F (40°C) Warm, moist skin Cool, moist skin Hot, dry skin - Weakness, Muscle cramping Weakness, Anxious, Tachypnea Hypotension, AMS / Coma Section Environmental Protocol PO Fluids as tolerated Age Appropriate Airway Protocol(s) AR 1 - 7 Monitor and Reassess as indicated Altered Mental Status Protocol UP 4 as indicated Active cooling measures Target Temp < 102.5° F (39°C) B 12 Lead ECG Procedure A IV / IO Procedure P Cardiac Monitor A Age Appropriate Hypotension / Shock Protocol AM 5 / PM 3 as indicated Monitor and Reassess Notify Destination or Contact Medical Control Revised TE 4 09/29/2017 Any local EMS System changes to this document must follow the NC OEMS Protocol Change Policy and be approved by OEMS Hyperthermia Toxic - Environmental Protocol Environmental Section Protocol Pearls • Recommended Exam: Mental Status, Skin, HEENT, Heart, Lungs, Neuro • Extremes of age are more prone to heat emergencies (i.e.