AAM See Aggressive Angiomyxoma (AAM) Abdominal Endometriosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

"General Pathology"
,, ., 1312.. CALIFORNIA TUMOR TISSUE REGISTRY "GENERAL PATHOLOGY" Study Cases, Subscription B October 1998 California Tumor Tissue Registry c/o: Department of l'nthology and Ruman Anatomy Loma Lindn Universily School'oflV.lcdicine 11021 Campus Avenue, AH 335 Lomn Linda, California 92350 (909) 824-4788 FAX: (909) 478-4188 E-mail: cU [email protected] CONTRIBUTOR: Philip G. R obinson, M.D. CASE NO. 1 - OcrOBER 1998 Boynton Beach, FL TISSUE FROM: Stomach ACCESSION #28434 CLINICAL ABSTRACT: This 67-year-old female was thought to have a pancreatic mass, but at surgery was found to have a nodule within the gastric wall. GROSS PATHOLOGY: The specimen consisted of a 5.0 x 5.5 x 4.5 em fragment of gray tissue. The cut surface was pale tan, coarsely lobular with cystic degeneration. SPECIAL STUDIES: Keratin negative Desmin negative Actin negative S-100 negative CD-34 trace to 1+ positive in stromal cells (background vasculature positive throughout) CONTRIBUTOR: Mar k J anssen, M.D. CASE NO. 2 - ocrOBER 1998 Anaheim, CA TISSUE FROM: Bladder ACCESSION #28350 CLINICAL ABSTRACT: This 54-year-old male was found to have a large rumor in his bladder. GROSS PATHOLOGY: The specimen consisted of a TUR of urinary bladder tissue, forming a 7.5 x 7. 5 x 1.5 em aggregate. SPECIAL STUDfES: C)1okeratin focally positive Vimentin highly positive MSA,Desmin faint positivity CONTRIBUTOR: Howard Otto, M.D. CASE NO.3 - OCTOBER 1998 Cheboygan, Ml TISSUE FROM: Appendix ACCESSION #28447 CLINICAL ABSTRACT: This 73-year-old female presented with acute appendicitis and at surgery was felt to have a periappendiceal abscess. -
CASE REPORT Uterine Rupture Due to Invasive Metastatic
UC Irvine Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health Title Uterine Rupture due to Invasive Metastatic Gestational Trophoblastic Neoplasm Permalink https://escholarship.org/uc/item/7064k01v Journal Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health, 14(5) ISSN 1936-900X Authors Bruner, David I Pritchard, Amy M Clarke, Jonathan E Publication Date 2013 DOI 10.5811/westjem.2013.4.15868 License https://creativecommons.org/licenses/by-nc/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California CASE REPORT Uterine Rupture Due to Invasive Metastatic Gestational Trophoblastic Neoplasm David I. Bruner, MD* * Naval Medical Center Portsmouth, Emergency Medicine Program, Portsmouth, Virginia Amy M. Pritchard, DO† † Naval Medical Hospital Camp Pendleton, Oceanside, California Jonathan Clarke, MD‡ ‡ Naval Medical Center Jacksonville, Jacksonville, Florida Supervising Section Editor: Rick McPheetors, DO Submission history: Submitted January 13, 2013; Revision received April 9, 2013; Accepted April 11, 2013 Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.2013.4.15868 While complete molar pregnancies are rare, they are wrought with a host of potential complications to include invasive gestational trophoblastic neoplasia. Persistent gestational trophoblastic disease following molar pregnancy is a potentially fatal complication that must be recognized early and treated aggressively for both immediate and long-term recovery. We present the case of a 21-year-old woman with abdominal pain and presyncope 1 month after a molar pregnancy with a subsequent uterine rupture due to invasive gestational trophoblastic neoplasm. We will discuss the complications of molar pregnancies including the risks and management of invasive, metastatic gestational trophoblastic neoplasia. -

Differential Diagnosis of Ovarian Mucinous Tumours Sigurd F
Differential Diagnosis of Ovarian Mucinous Tumours Sigurd F. Lax LKH Graz II Academic Teaching Hospital of the Medical University Graz Pathology Mucinous tumours of the ovary • Primary ➢Seromucinous tumours ➢Mucinous tumours ➢Benign, borderline, malignant • Secondary (metastatic) ➢Metastases (from gastrointestinal tract) • Metastases can mimic primary ovarian tumour Mucinous tumours: General • 2nd largest group after serous tumours • Gastro-intestinal differentiation (goblet cells) • Endocervical type> seromucinous tumours • Majority is unilateral, particularly cystadenomas and borderline tumours • Bilaterality: rule out metastatic origin • Adenoma>carcinoma sequence reflected by a mixture of benign, atypical proliferating and malignant areas within the same tumour Sero-mucinous ovarian tumours • Previous endocervical type of mucinous tumor • Mixture of at least 2 cell types: mostly serous • Association with endometriosis; multifocality • Similarity with endometrioid and serous tumours, also immunophenotype • CK7, ER, WT1 positive; CK20, cdx2 negativ • Most cystadenoma and borderline tumours • Carcinomas rare and difficult to diagnose Shappel et al., 2002; Dube et al., 2005; Vang et al. 2006 Seromucinous Borderline Tumour ER WT1 Seromucinous carcinoma being discontinued? • Poor reproducibility: Low to modest agreement from 39% to 56% for 4 observers • Immunophenotype not unique, overlapped predominantly with endometrioid and to a lesser extent with mucinous and low-grade serous carcinoma • Molecular features overlap mostly with endometrioid -
CD133 Expression in Placenta Chorioangioma Presenting As a Giant Asymptomatic Mass
medicina Case Report CD133 Expression in Placenta Chorioangioma Presenting as a Giant Asymptomatic Mass Gianluca Di Massa 1,†, Guglielmo Stabile 2,† , Federico Romano 2 , Andrea Balduit 3 , Alessandro Mangogna 2,* , Beatrice Belmonte 4 , Pina Canu 1, Emma Bertucci 5, Giuseppe Ricci 2,6,‡ and Tiziana Salviato 1,‡ 1 Department of Diagnostic, Clinic and Public Health Medicine, University of Modena and Reggio Emilia, 41125 Modena, Italy; [email protected] (G.D.M.); [email protected] (P.C.); [email protected] (T.S.) 2 Institute for Maternal and Child Health, IRCCS Burlo Garofolo, Via dell’Istria, 65/1, 34137 Trieste, Italy; [email protected] (G.S.); [email protected] (F.R.); [email protected] (G.R.) 3 Department of Life Sciences, University of Trieste, 34127 Trieste, Italy; [email protected] 4 Tumor Immunology Unit, Department of Health Promotion, Mother and Child Care, Internal Medicine and Medical Specialties, University of Palermo, 90134 Palermo, Italy; [email protected] 5 Prenatal Medicine Unit, Obstetrics and Gynecology Unit, Department of Medical and Surgical Sciences for Mother, Child and Adult, University of Modena and Reggio Emilia, 41125 Modena, Italy; [email protected] 6 Department of Medical, Surgical and Health Science, University of Trieste, 34129 Trieste, Italy * Correspondence: [email protected]; Tel.: +39-320-612-3370 † These authors contributed equally to this article. Citation: Di Massa, G.; Stabile, G.; ‡ These authors contributed equally to this article. Romano, F.; Balduit, A.; Mangogna, A.; Belmonte, B.; Canu, P.; Abstract: Background: Placental chorioangioma is the most common benign non-trophoblastic neo- Bertucci, E.; Ricci, G.; Salviato, T. -

A Case of Krukenberg Tumor Metastasized from Colon Cancer In
A case of Krukenberg tumor metastasized from colon cancer in pregnancy Oztas E, Ozler S, Ersoy AO, Turker M, Zengın NI, Caglar AT, Danisman N Zekai Tahir Burak Women's Health Education and Research Hospital, Ankara, Turkey Objective Krukenberg tumor refers to gastrointestinal cancer metastatic to the ovaries and has an extremely poor prognosis, with a 5-year survival rate ranging from 12% to 23. 4%. Gastric cancer has been reported as the most frequent primary source of Krukenberg tumor; however, tumors of the colon, appendix, breast, lung, and pancreas have also been reported to metastasize into the ovaries. Krukenberg tumors are usually seen in the fifth decade of life, with an average age of 45 years and cases diagnosed during pregnancy are thus extremely rare. Methods We report a case of a Krukenberg tumor secondary to colon carcinoma in a pregnant woman with acute pelvic pain. The prenatal diagnosis was made at 17 weeks’ gestation. Results A 27-year-old, primigravida with a semisolid right adnexial mass was presented with acute pelvic pain at 17 weeks’ gestation. Ultrasonography revealed a semisolid right adnexial mass of 140×130 mm and ascites, as well as a single live fetus compatible for gestational age. The abdomen was tense, tender and distended so exploratory laparotomy was performed with the suspicion of ovarian torsion. During the operation, ascites, enlarged right ovary with the presence of a necrotic tumor measuring 160×140 mm causing ovarian torsion and omental metastasis were seen. Unilateral oophorectomy and omentectomy were then performed. Histopathological examination of the specimen revealed adenocarcinoma metastasis to the ovary and the omentum probably originating from a primary gastrointestinal carcinoma (Figure-1). -
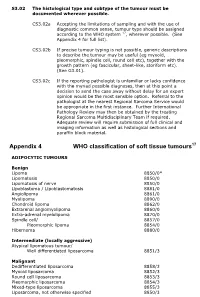
Appendix 4 WHO Classification of Soft Tissue Tumours17
S3.02 The histological type and subtype of the tumour must be documented wherever possible. CS3.02a Accepting the limitations of sampling and with the use of diagnostic common sense, tumour type should be assigned according to the WHO system 17, wherever possible. (See Appendix 4 for full list). CS3.02b If precise tumour typing is not possible, generic descriptions to describe the tumour may be useful (eg myxoid, pleomorphic, spindle cell, round cell etc), together with the growth pattern (eg fascicular, sheet-like, storiform etc). (See G3.01). CS3.02c If the reporting pathologist is unfamiliar or lacks confidence with the myriad possible diagnoses, then at this point a decision to send the case away without delay for an expert opinion would be the most sensible option. Referral to the pathologist at the nearest Regional Sarcoma Service would be appropriate in the first instance. Further International Pathology Review may then be obtained by the treating Regional Sarcoma Multidisciplinary Team if required. Adequate review will require submission of full clinical and imaging information as well as histological sections and paraffin block material. Appendix 4 WHO classification of soft tissue tumours17 ADIPOCYTIC TUMOURS Benign Lipoma 8850/0* Lipomatosis 8850/0 Lipomatosis of nerve 8850/0 Lipoblastoma / Lipoblastomatosis 8881/0 Angiolipoma 8861/0 Myolipoma 8890/0 Chondroid lipoma 8862/0 Extrarenal angiomyolipoma 8860/0 Extra-adrenal myelolipoma 8870/0 Spindle cell/ 8857/0 Pleomorphic lipoma 8854/0 Hibernoma 8880/0 Intermediate (locally -

Eyelid Conjunctival Tumors
EYELID &CONJUNCTIVAL TUMORS PHOTOGRAPHIC ATLAS Dr. Olivier Galatoire Dr. Christine Levy-Gabriel Dr. Mathieu Zmuda EYELID & CONJUNCTIVAL TUMORS 4 EYELID & CONJUNCTIVAL TUMORS Dear readers, All rights of translation, adaptation, or reproduction by any means are reserved in all countries. The reproduction or representation, in whole or in part and by any means, of any of the pages published in the present book without the prior written consent of the publisher, is prohibited and illegal and would constitute an infringement. Only reproductions strictly reserved for the private use of the copier and not intended for collective use, and short analyses and quotations justified by the illustrative or scientific nature of the work in which they are incorporated, are authorized (Law of March 11, 1957 art. 40 and 41 and Criminal Code art. 425). EYELID & CONJUNCTIVAL TUMORS EYELID & CONJUNCTIVAL TUMORS 5 6 EYELID & CONJUNCTIVAL TUMORS Foreword Dr. Serge Morax I am honored to introduce this Photographic Atlas of palpebral and conjunctival tumors,which is the culmination of the close collaboration between Drs. Olivier Galatoire and Mathieu Zmuda of the A. de Rothschild Ophthalmological Foundation and Dr. Christine Levy-Gabriel of the Curie Institute. The subject is now of unquestionable importance and evidently of great interest to Ophthalmologists, whether they are orbital- palpebral specialists or not. Indeed, errors or delays in the diagnosis of tumor pathologies are relatively common and the consequences can be serious in the case of malignant tumors, especially carcinomas. Swift diagnosis and anatomopathological confirmation will lead to a treatment, discussed in multidisciplinary team meetings, ranging from surgery to radiotherapy. -

(12) Patent Application Publication (10) Pub. No.: US 2015/0353527 A1 Zisman (43) Pub
US 20150353527A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2015/0353527 A1 Zisman (43) Pub. Date: Dec. 10, 2015 (54) NON-SELECTIVE KINASE INHIBITORS Publication Classification (71) Applicant: arence ZIAMAN, Slingerlands, NY (51) Int. Cl. (US) C07D 40/12 (2006.01) (72) Inventor: Lawrence S Zisman, Slingerlands, NY C07D 24/20 (2006.01) (US) C07D 403/2 (2006.01) (73) Assignee: PULMOKINE, INC. Slingerlands, NY (52) U.S. Cl. (US) CPC ............ C07D401/12 (2013.01); C07D 403/12 (21) Appl. No.: 14f76O139 (2013.01); C07D 241/20 (2013.01) y x- - - 9 (22) PCT Filed: Jan. 9, 2014 (57) ABSTRACT (86). PCT No.: PCT/US1.4/10778 T.S. ). L. 9, 2015 Disclosed herein are compounds, compositions, and methods e 19 for preventing and treating proliferative diseases associated Related U.S. Application Data with aberrant receptor tyrosine kinase (RTK) activity. The (60) Provisional application No. 61/751.217, filed on Jan. therapeutic indications described herein more specifically 10, 2013, provisional application No. 61/889,887, relate to the non-selective inhibition of RTKs associated with filed on Oct. 11, 2013. vascular and pulmonary disorders. Patent Application Publication Dec. 10, 2015 Sheet 1 of 26 US 2015/0353527 A1 FIG. 1A $: 8:3 $38: Coacentration (nM) FG, B C s C am u was e D 9 9 A. Concentration (nM) Patent Application Publication Dec. 10, 2015 Sheet 2 of 26 US 2015/0353527 A1 F.G. 1 C Concentration (in M) F.G. 1D c C R sa spagh d g e d A. :::::: Concentration (in M) Patent Application Publication Dec. -

Placenta 111 (2021) 33–46
Placenta 111 (2021) 33–46 Contents lists available at ScienceDirect Placenta journal homepage: www.elsevier.com/locate/placenta Review Placental pathology in cancer during pregnancy and after cancer treatment exposure Vera E.R.A. Wolters a, Christine A.R. Lok a, Sanne J. Gordijn b, Erica A. Wilthagen c, Neil J. Sebire d, T. Yee Khong e, J. Patrick van der Voorn f, Fred´ ´eric Amant a,g,* a Department of Gynecologic Oncology and Center for Gynecologic Oncology Amsterdam (CGOA), Netherlands Cancer Institute - Antoni van Leeuwenhoek and University Medical Centers Amsterdam, Plesmanlaan 121, 1066, CX Amsterdam, the Netherlands b Department of Gynaecology and Obstetrics, University of Groningen, University Medical Center Groningen, CB 20 Hanzeplein 1, 9713, GZ Groningen, the Netherlands c Scientific Information Service, Netherlands Cancer Institute - Antoni van Leeuwenhoek, Plesmanlaan 121, 1066, CX Amsterdam, the Netherlands d Department of Paediatric Pathology, NIHR Great Ormond Street Hospital BRC, London, WC1N 3JH, United Kingdom e SA Pathology, Women’s and Children’s Hospital, 72 King William Road, North Adelaide, SA5006, Australia f Department of Pathology, University Medical Centers Amsterdam, Location VU University Medical Center, De Boelelaan 1117, 1081 HV, Amsterdam, the Netherlands g Department of Oncology, KU Leuven, Herestraat 49, 3000, Leuven, Belgium ARTICLE INFO ABSTRACT Keywords: Cancer during pregnancy has been associated with (pathologically) small for gestational age offspring, especially Placenta after exposure to chemotherapy in utero. These infants are most likely growth restricted, but sonographic results Cancer are often lacking. In view of the paucity of data on underlying pathophysiological mechanisms, the objective was Pregnancy to summarize all studies investigating placental pathology related to cancer(treatment). -

Apocrine Hidrocystoma: a Slowly Growing Postauricular Translucent Nodule
Volume 27 Number 1| January 2021 Dermatology Online Journal || Photo Vignette 27(1):16 Apocrine hidrocystoma: a slowly growing postauricular translucent nodule Karan Pandher1 BS, Felipe B Cerci2,3 MD MSc, Stanislav N Tolkachjov4 MD Affiliations: 1Chicago Medical School, Rosalind Franklin University of Medicine and Science, North Chicago, Illinois, USA, 2Department of Dermatology. Hospital de Clínicas da Universidade Federal do Paraná, Curitiba, Brazil, 3Clínica Cepelle. Curitiba, Brazil, 4Epiphany Dermatology, Dallas, Texas, USA Corresponding Author: Stanislav N Tolkachjov MD, Epiphany Dermatology, 1640 FM 544, Suite 100, The Colony, TX 75056, Tel: 972-712- 3131, Email: [email protected] importance of histopathological examination of Abstract cystic tumors on the periauricular area. Apocrine hidrocystoma is a benign, cystic proliferation of the apocrine sweat gland that may present commonly on sun-exposed areas of the head Case Synopsis and neck. However, given its location and features, A middle-aged previously healthy woman presented apocrine hidrocystomas may often be confused with with an asymptomatic right postauricular lesion, that malignant tumors such as basal cell carcinomas or primary cutaneous mucinous carcinomas. Herein, we progressed to a nodule over 10 years (Figure 1A). present an unusual case of an apocrine hidrocystoma Physical examination demonstrated a translucent, presenting in the postauricular region and highlight blue-gray nodule with three rounded projections the importance of histopathological examination of and a fibroelastic consistency in the right cystic tumors on the periauricular area. postauricular region measuring 2.3×2cm in diameter. The well-defined nodule was not adherent to deep planes. A similar papule was present Keywords: apocrine hidrocystoma, dermatology, superiorly. -

Please Bring Your ~Rotocol, but Do Not Bring Slides Or Microscopes to T He Meeting, CALIFORNIA TUMOR TISSUE REGISTRY
CALIFORNIA TUMOR TISSUE REGISTRY FIFTY- SEVENTH SEMI-ANNUAL SLIDE S~IINAR ON TIJMORS OF THE F~IALE GENITAL TRACT MODERATOR: RlCl!AlUJ C, KEMPSON, M, D, ASSOCIATE PROFESSOR OF PATHOLOGY & CO-DIRECTOR OF SURGICAL PATHOLOGY STANFORD UNIVERSITY MEDICAL CEllTER STANFOliD, CALIFORNIA CHAl~lAN : ALBERT HIRST, M, D, PROFESSOR OF PATHOLOGY LOMA LINDA UNIVERSITY MEDICAL CENTER L~.A LINDA, CALIPORNIA SUNDAY, APRIL 21, 1974 9 : 00 A. M. - 5:30 P,M, REGISTRATION: 7:30 A. M. PASADENA HILTON HOTEL PASADENA, CALIFORNIA Please bring your ~rotocol, but do not bring slides or microscopes to t he meeting, CALIFORNIA TUMOR TISSUE REGISTRY ~lELDON K, BULLOCK, M, D, (EXECUTIVE DIRECTOR) ROGER TERRY, ~1. Ii, (CO-EXECUTIVE DIRECTOR) ~Irs, June Kinsman Mrs. Coral Angus Miss G, Wilma Cline Mrs, Helen Yoshiyama ~fr s. Cheryl Konno Miss Peggy Higgins Mrs. Hataie Nakamura SPONSORS: l~BER PATHOLOGISTS AMERICAN CANCER SOCIETY, CALIFORNIA DIVISION CALIFORNIA MEDICAL ASSOCIATION LAC-USC MEDICAL CENlllR REGIONAL STUDY GRaJPS: LOS ANGELES SAN F~ICISCO CEt;TRAL VALLEY OAKLAND WEST LOS ANGELES SOUTH BAY SANTA EARBARA SAN DIEGO INLAND (SAN BERNARDINO) OHIO SEATTLE ORANGE STOCKTON ARGENTINA SACRJIMENTO ILLINOIS We acknowledge with thanks the voluntary help given by JOHN TRAGERMAN, M. D., PATHOLOGIST, LAC-USC MEDICAL CENlllR VIVIAN GILDENHORN, ASSOCIATE PATHOLOGIST, I~TERCOMMUNITY HOSPITAL ROBERT M. SILTON, M. D,, ASSISTANT PATHOLOGIST, CITY OF HOPE tiEDICAL CENTER JOHN N, O'DON~LL, H. D,, RESIDENT IN PATHOLOGY, LAC-USC MEDICAL CEN!ER JOHN R. CMIG, H. D., RESIDENT IN PATHOLOGY, LAC-USC MEDICAL CENTER CHAPLES GOLDSMITH, M, D. , RESIDENT IN PATHOLOGY, LAC-USC ~IEDICAL CEUTER HAROLD AMSBAUGH, MEDICAL STUDENT, LAC-USC MEDICAL GgNTER N~IE-: E, G. -

New Management of Gestational Trophoblastic Diseases; a Continuum of Moles to Choriocarcinoma: a Review Article
©2018 ASP Ins., Afarand Scholarly Publishing Institute, Iran ISSN: 2476-5848; Journal of Obstetrics, Gynecology and Cancer Research. 2018;3(3):123-128. New Management of Gestational trophoblastic diseases; A Continuum of Moles to Choriocarcinoma: A Review Article A R T I C L E I N F O A B S T R A C T Introduction Article Type Gestational trophoblastic diseases (GTD) is the only group of female reproductive neoplasms derived from paternal genetic material (Androgenic origin). GTD Analytical Review Authors is a continuum from benign to malignant; molar pregnancy is benign, but choriocarcinoma 1 MD is malignant. Approximately 45% of patients have metastatic disease when Gestational 1 MD trophoblastic neoplasia (GTN) is diagnosed. GTN is unique in women malignancies because 2 Soheila Aminimoghaddam* MD, PhD it arises from trophoblast but not from genital organs. It is curable with chemotherapy, Nastaran Abolghasem , Tahereh Ashraf- Ganjooie , low-risk GTN completely response to single-agent chemotherapy and does not require Conclusionhistological confirmation. In persistent GTN, clinical staging and workup of metastasis should be performed. The aim of the present study was to review the new management of GTD. In the case of brain, liver, or renal metastases, any woman of reproductive age How to cite this article who presents with an apparent metastatic malignancy of unknown primary site should be screened for the possibility of GTN with a serum HCG level. Excisional biopsy is not indicated to histologically confirm the diagnosis of malignant GTN if the patient is not pregnant and Soheila Aminimoghaddam, Nas- taran Abolghasem, Tahereh As-hraf- has a high HCG value.