Here As a Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Getting to the Western General Hospital
gettinggetting toto TheThe WesternWestern GeneralGeneral HospitalHospital atat CreweCrewe RoadRoad SthSth University Hospitals Division How to find your way around The following floor markings will help you find your way. I Junction of the North Corridor and the Link Corridor G Junction of the Link Corridor with the South Corridor L Junction of the South Corridor with the West Corridor AREA FLOOR BUILDING Oncology Outpatients.........................................Ground Floor ..............Edinburgh Cancer Centre Acute Receiving Unit ..........................................Ground Floor ..............Outpatient Building Outpatient Clinics (A,B,D)..................................1st Floor.....................Outpatient Building Body Scanner.......................................................Lower Ground.............Outpatient Building Outpatient Clinics................................................Lower Ground.............Anne Ferguson Bldg Breast Unit .............................................................................................As shown on the map Paediatric Clinics .................................................Lower Ground.............Outpatient Building Cardiac Lab Appointments .................................Ground Floor ..............Anne Ferguson Bldg Pathology.............................................................1st Floor.....................Alexander Donald Bldg Cardiology Day Unit ...........................................Ground Floor ..............Anne Ferguson Bldg Pharmacy..............................................................Ground -

LHB37 LOTHIAN HEALTH BOARD Introduction 1 Agenda of Meetings of Lothian Health Board, 1987-1995 2 Agenda of Meetings of Lothia
LHB37 LOTHIAN HEALTH BOARD Introduction 1 Agenda of Meetings of Lothian Health Board, 1987-1995 2 Agenda of Meetings of Lothian Health Board Committees, 1987-1989 2A Minutes of Board, Standing Committees and Sub-Committees, 1973-1986 2B Draft Minutes of Board Meetings, 1991-2001 2C [not used] 2D Area Executive Group Minutes, 1973-1986 2E Area Executive Group Agendas and Papers, 1978-1985 2F Agenda Papers for Contracts Directorate Business Meetings, 1993-1994 2G Agenda Papers of Finance, Manpower and Establishment Committee, 1975-1979 2H Agenda papers of the Policy and Commissioning Team Finance and Corporate Services Sub- Group, 1994-1995 2I [not used] 2J Minutes and Papers of the Research Ethics Sub-Committees, 1993-1995 3 Annual Reports, 1975-2004 4 Annual Reports of Director of Public Health, 1989-2008 5 Year Books, 1977-1992 6 Internal Policy Documents and Reports, 1975-2005 7 Publications, 1960-2002 8 Administrative Papers, 1973-1994 8A Numbered Administrative Files, 1968-1993 8B Numbered Registry Files, 1970-1996 8C Unregistered Files, 1971-1997 8D Files of the Health Emergency Planning Officer, 1978-1993 9 Annual Financial Reviews, 1974-1987 10 Annual Accounts, 1976-1992 10A Requests for a major item of equipment, 1987-1990 LHB37 LOTHIAN HEALTH BOARD 11 Lothian Medical Audit Committee, 1988-1997 12 Records of the Finance Department, 1976-1997 13 Endowment Fund Accounts, 1972-2004 14 Statistical Papers, 1974-1990 15 Scottish Health Service Costs, 1975-1987 16 Focus on Health , 1982-1986 17 Lothian Health News , 1973-2001 18 Press -

Diabetes and Endocrinology
Diabetes and Endocrinology Specialty Induction Guide OPD2 Royal Infirmary of Edinburgh 51, Little France Crescent Edinburgh EH16 4SA Metabolic Unit Anne Ferguson Building Western General Hospital Crewe Road Edinburgh EH4 2XU July 2017 Induction information July 2017 Updated July 2017 Page 0 ENDOCRINOLOGY AND DIABETES IN EDINBURGH CONTENTS Contents ……………………………………………... Page 1 Introduction ………………………………………….. Page 2 RIE Who’s Who ……………………………….. Page 3-4 Unit meetings ……………………………... Page 4 Clinic timetable …………………………… Page 4-6 OPD2 information ………………………… Page 7 Diabetes clinic referral forms …………….... Page 7-8 Information for ST trainees…..…………...... Page 9 Roodlands Hospital Haddington.…………. Page 11 GP placement information ………………… Page 11 WGH Who’s Who ……………………………….... Page 12 Unit meetings ………………………………. Page 13 Clinic timetable …………………………….. Page 13-15 Information for ST trainees……………........ Page 16-18 Leith Community Treatment Centre ………. Page 18 GP placement information ………………… Page 19 CMT information …………………………... Page 19 General information SCI-Diabetes ……………………………….. Page 20-26 Diasend .......................................................... Page 27-31 CSII downloads on Carelink ......................... Page 32 ECED website and resources for T1DM ...... Page 33 Mental Health …………………………........ Page 34-35 IT systems for logging on call work ………. Page 36-37 Clinical outcoming ………………………… Page 38-40 Confidentiality and safe Email transmission . Page 41-43 Social media policy ………………………… Page 44-49 Computer Network Access application -

Services for Older People in the City of Edinburgh
Services for older people in the city of Edinburgh December 2018 Progress review following a joint inspection Contents 1. Background to this progress review 3 2. How we conducted this progress review 3 3. Progress made: what we found overview 4 4. Progress on recommendations for improvement 6 5. Conclusion and what happens next 38 Appendix 1: city of Edinburgh health and social care partnership 39 locality operational structure Appendix 2: city of Edinburgh health and social care partnership 40 planning and governance structure This report should be read alongside our original inspection report on which this progress review is based on. This can be found at: www.careinspectorate.com/images/documents/3831/Edinburgh%20services%20for %20older%20people%20joint%20inspection%20report%20May%202017.pdf The Care Inspectorate and Healthcare Improvement Scotland jointly publish this progress review report. To find out more go to www.careinspectorate.com/ or www.healthcareimprovementscotland.org/ Services for older people in the city of Edinburgh Page 2 of 40 1. Background to this progress review The Care Inspectorate and Healthcare Improvement Scotland jointly carried out an inspection of services for older people in the city of Edinburgh between October and December 2016. We published a joint inspection report in May 2017, which is available on both scrutiny bodies’ websites. The purpose of the joint inspection was to find out how well the partnership achieved good personal outcomes for older people and their unpaid carers1. The report highlighted important weaknesses and where performance was unsatisfactory. We stated that we would monitor improvement and return to the partnership to review progress in 2018. -

Group B 09-10
Supervisor Supervisor Address Supervisor Email Project Title Room S1642, RIE, 51 A systematic review of Little France Crescent, cognitive impairment in Dr Gillian Mead Edinburgh [email protected] patients with atrial Cardiology, RIE, 51 The Role of Endothelial Little France Cres, Progenitor Cells in Prof David Newby Edinburgh [email protected] Abdominal Aortic Dept of Cardiology, Diagnosis and Dr Muhammad Royal Hospital for Sick [email protected] Management of Walayat Children, Edinburgh, hs.uk Cardiomyopathy Endocrinology Unit, Centre for Cardiovascular Science, Queen's Effects of obesity in Dr Mandy Drake Medical Research [email protected] pregnancy Room S1642, RIE, 51 Post-stroke fatigue: the Dr Gillian Mead Little France Cres, [email protected] patient's prespective Dept of Urology, Optimisation of novel Western General markers of hypoxia in Mr Grant Stewart Hospital, Crewe Road, [email protected] prostate cancer Cardiology, RIE, 51 Pulse wave velocity Dr Nick Boon Little France Cres, [email protected] analysis Room E2.46, Centre for Changes in Inflammation Research, microvasculature Queen's Medical associated with chronic Research Institute, 47 graft injury following renal Ms Lorna Marson Little France Crescent, [email protected] transplantation Public Health Sciences, International child health Prof Harry Campbell Teviot Place, Edinburgh [email protected] development Division of Clinical A Systematic Review of Neurosciences, the effects of genetic Western General polymorphisms on the Dr Cathie Sudlow Hospital, Crewe Road, [email protected] outcome of stroke Community Child An audit of health services Dr Patricia D. -

A Feasibility Study to Investigate the Clinical Application of Functional
Edinburgh Research Explorer A Feasibility Study to Investigate the Clinical Application of Functional Electrical Stimulation (FES), for Dropped Foot, During the Sub-Acute Phase of Stroke - A Randomized Controlled Trial Citation for published version: Salisbury, L, Shiels, J, Todd, I & Dennis, M 2013, 'A Feasibility Study to Investigate the Clinical Application of Functional Electrical Stimulation (FES), for Dropped Foot, During the Sub-Acute Phase of Stroke - A Randomized Controlled Trial', Physiotherapy Theory and Practice, vol. 29, no. 1, pp. 31-40. https://doi.org/10.3109/09593985.2012.674087 Digital Object Identifier (DOI): 10.3109/09593985.2012.674087 Link: Link to publication record in Edinburgh Research Explorer Document Version: Peer reviewed version Published In: Physiotherapy Theory and Practice Publisher Rights Statement: © Salisbury, L., Shiels, J., Todd, I., & Dennis, M. (2013). A Feasibility Study to Investigate the Clinical Application of Functional Electrical Stimulation (FES), for Dropped Foot, During the Sub-Acute Phase of Stroke - A Randomized Controlled Trial. Physiotherapy Theory and Practice, 29(1), 31-40 doi: 10.3109/09593985.2012.674087 General rights Copyright for the publications made accessible via the Edinburgh Research Explorer is retained by the author(s) and / or other copyright owners and it is a condition of accessing these publications that users recognise and abide by the legal requirements associated with these rights. Take down policy The University of Edinburgh has made every reasonable effort to ensure that Edinburgh Research Explorer content complies with UK legislation. If you believe that the public display of this file breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. -

A Brief Look at the History of the Deaconess Hospital, Edinburgh
J R Coll Physicians Edinb 2018; 48: 78–84 | doi: 10.4997/JRCPE.2018.118 PAPER A brief look at the history of the Deaconess Hospital, Edinburgh, 1894–1990 HistoryER McNeill1, D Wright2, AK Demetriades 3& Humanities The Deaconess Hospital, Edinburgh, opened in 1894 and was the rst Correspondence to: establishment of its kind in the UK, maintained and wholly funded as it E McNeill Abstract was by the Reformed Church. Through its 96-year lifetime it changed and Chancellor’s Building evolved to time and circumstance. It was a school: for the training of nurses 48 Little France Crescent and deaconesses who took their practical skills all over the world. It was a Edinburgh EH16 45B sanctum: for the sick-poor before the NHS. It was a subsidiary: for the bigger UK hospitals of Edinburgh after amalgamation into the NHS. It was a specialised centre: as the Urology Department in Edinburgh and the Scottish Lithotripter centre. And now it is currently Email: student accommodation. There is no single source to account for its history. Through the use [email protected] of original material made available by the Lothian Health Services Archives – including Church of Scotland publications, patient records, a doctor’s casebook and annual reports – we review its conception, purpose, development and running; its fate on joining the NHS, its identity in the latter years and nally its closure. Keywords: Charteris, Church of Scotland, Deaconess Hospital, Pleasance Declaration of interests: No confl ict of interests declared Introduction Figure 1 Charteris Memorial Church, St Ninian’s and the Deaconess Hospital, 1944 On a November morning in 1888, two men stood in the Pleasance area of Edinburgh looking across the street to an old house, which 200 years before had been the town residence of Lord Carnegie. -

Peter Goes Back to the Floor
THE NEWSPAPER FOR NHS LOTHIAN STAFF MAY/JUNE 2008 ISSUE 26 ConnectionsYOUR AWARD-WINNING NEWSPAPER PETER GOES BACK WIN A FABULOUS TO THE FLOOR PAMPER SESSION! PAGE 14 PAGE 15 £8M CASH BOOST FOR PUBLIC HEALTH SERVICES Government cash will help board tackle alcohol and tobacco misuse NHS Lothian has been awarded dependent drinkers, more treatment £8 million to deal with specific and prevention/education services public health issues such as and appropriate recording systems. alcohol misuse, sexual health The second largest sum of THANK YOU: auxiliary nurse Fay Watt, left, has a very special reason for presenting and stopping smoking money has been awarded for flowers to her nursing colleagues – turn to page 3 to read their heart-warming tale… programmes. prevention of blood-borne viruses. Just over £3.4m has been A continuing £2.52m is to be used awarded for alcohol misuse. to reduce the spread of HIV and The Scottish Government has hepatitis. tobacco control efforts. The Scottish Government acknowledges increased alcohol misuse funding Revised performance This being the case, funding by almost 150 per cent compared management arrangements to of £911,000 is being continued for that very significant progress has to 2007/08. ensure NHS boards use the NHS Lothian to provide stop been made in reducing smoking through The additional money is to help money effectively will be provided smoking services that help NHS boards meet targets for by the end of May. people quit. comprehensive tobacco control reducing consumption and related The Scottish Government The money allocated is to go harm and the Government expects acknowledges that very towards reducing smoking in help improve the sexual programme, which tackles considerable work to be done in significant progress has been made the adult population to 22 per health of Lothian’s population, health inequalities that are this area. -

NHS Lothian Job Packs
NHS LOTHIAN Post: Band 2 Health Care Support Worker Discharge Lounge WGH PERSON SPECIFICATION In order to be shortlisted you must demonstrate you meet all the essential criteria and as much of the desirable as possible. When a large volume of applications are received for a vacancy and most applicants meet the essential criteria then the desirable criteria is used to produce the shortlist. How Criteria Essential Desirable assessed Personal Traits Caring, respectful, polite, A, I, R compassionate Good communication skills Well presented Flexible with shift pattern Qualifications Must have a good educational Healthcare qualification e.g. A, C, I and Training background and a high standard SVQ level II or III in health of written and verbal and social care communication. Experience and Evidence of ability to work within a team Previous experience within a A, I, R Knowledge Awareness of confidentiality within the caring or healthcare job remit environment Skills and/or Ability to carry out assigned tasks IT skills A, I, R Abilities effectively in a busy environment Enthusiasm to learn and Contribute and work as part of a wider develop team of healthcare professionals Good interpersonal skills particularly dealing with people either in person or on the telephone. Specific Job Ability to undertake further Evidence of further A, C, R Requirements training in SVQ II. education To work within standards set out in HCSW code of conduct Good time keeping and flexibility Involves direct contact with body fluids, on a number of occasions per shift. Key – how assessed A = Application form I = Interview C = Copies of certificates T= Test or exercise P = Presentation R = References JOB DESCRIPTION CLINICAL SUPPORT WORKER SVQ CARE LEVEL 2 (QUALIFIED) Band 2 HCSW Job Specification for General surgery – September 2013 V1 1. -
Work Experience Application Form
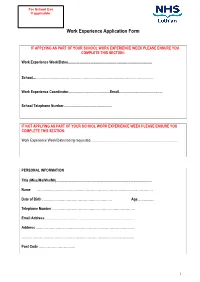
For School Use If applicable: Work Experience Application Form IF APPLYING AS PART OF YOUR SCHOOL WORK EXPERIENCE WEEK PLEASE ENSURE YOU COMPLETE THIS SECTION: Work Experience Week/Dates........................................................................................... School....……………………………………………………………………………………………. Work Experience Coordinator.............................................Email............................................... School Telephone Number.................................................... IF NOT APPLYING AS PART OF YOUR SCHOOL WORK EXPERIENCE WEEK PLEASE ENSURE YOU COMPLETE THIS SECTION: Work Experience Week/Dates being requested............................................................................................. PERSONAL INFORMATION Title (Miss/Ms/Mrs/Mr)....................................................................................................... Name …………………………………………………………………………………………… Date of Birth ……………………………………………………… Age.................. Telephone Number ………………………………………………………………… Email Address ……………………………………………………………………… Address ……………………………………………………………………………… ………………………………………………………………………………………… Post Code …………………………… 1 PLEASE INDICATE YOUR CHOSEN CAREER PATH …………………………………………………………………………………………. Please indicate your choice of placement and list your 1. preference in order (e.g. midwifery, cardiology) 2. 3. PLEASE INDICATE THE LOCATIONS YOU CAN CONSIDER Placement Location: using numbers (1 being your first choice, 2 being your second choice, etc) please mark all the areas that you could -

Referral to Hospital a Guide to Referral and Waiting Times
You have been referred to: __________________________________ Midlothian Health & Social Care Partnership Referral to hospital A guide to referral and waiting times This information sheet tells you about what Your appointment happens when your doctor makes a hospital You should be given seven days notice of your referral for you. It covers waiting times, appointment. changing appointments and who to contact for more information. What to do if you can’t make your Making a referral appointment or have a query If the doctor is referring you to hospital, Please contact the department, using the phone she or he will contact the relevant hospital number on your appointment letter, as soon as department shortly after they have seen you can. Then they can give your appointment to you. At this point, it is really important to someone else and agree a more suitable time with you. make sure that the practice has your current address and phone number, so Turning down appointments that we can pass on the correct details to Please remember that if you turn down two the hospital. reasonable offers of appointment, the hospital From this point onwards, the hospital will be dealing may send you back to your GP and your waiting directly with you, usually by letter. Make sure you time will start again. ask your doctor which department and which hospital your are being referred to in case you need Going on holiday? to get in touch with them later on. If you are waiting to hear about an appointment Waiting times and you are about to go on holiday, please let the The hospital department will try to make your hospital know when you will be away. -

Lothian NHS Board Waverley Gate 2-4 Waterloo Place Edinburgh EH1 3EG
Lothian NHS Board Waverley Gate 2-4 Waterloo Place Edinburgh EH1 3EG Telephone: 0131 536 9000 www.nhslothian.scot.nhs.uk www.nhslothian.scot.nhs.uk Date: 14/10/2020 Your Ref: Our Ref: 4687 Enquiries to : Richard Mutch Extension: 35687 Direct Line: 0131 465 5687 [email protected] [email protected] Dear FREEDOM OF INFORMATION –THEATRES I write in response to your request for information in relation to theatres within NHS Lothian. Question: 1. Please list the number of surgical theatres (including day case) at each of the following hospital sites. Answer: Royal Infirmary of Edinburgh 28 Liberton Hospital 0 Western General Hospital 9 St John’s Hospital 13 Question: 2. Please list the number of induction rooms (including day case) at each of the following hospital sites. Answer: Royal Infirmary of Edinburgh 28 Liberton Hospital 0 Western General Hospital 9 St John’s Hospital 12 Question: 3. Please provide a list detailing the manufacturer, model and year of purchase for all anaesthesia machines currently in operation at each of the following hospital sites. Answer: Royal Infirmary of Edinburgh Enclosed table Liberton Hospital 0 Western General Hospital Enclosed table St John’s Hospital Enclosed table 4687 – Theatres - October 2020 Question: 4. Please provide the name of the clinical equipment lead for anaesthetic machines? (Usually an anaesthetist). Please could you provide the information broken down to each Hospital named above and not Trust wide. Answer: Royal Infirmary of Edinburgh , Anaesthetic Clinical Director Liberton Hospital N/A Western General Hospital , Anaesthetic Clinical Director St John’s Hospital , Anaesthetic Clinical Director I hope the information provided helps with your request.