An Important Tool for the Occupational Therapy Tool Box
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hub South East Scotland Territory Annual Report 2016-2017
Hub South East Scotland Territory Annual Report 2016-2017 ‰ Hub South East: Your Development Partner of Choice Our achievements : 2010 onwards HUB PROJECTS VALUE OF VALUE IN SOUTH EAST SCOTLAND PROPORTION of CONSTRUCTION WORK PACKAGES AWARDED to £563m SCOTTISH SMEs £ 349 197m OPEN and OPERATIONAL NEW JOBS % £185m IN CONSTRUCTION created 87 £181m IN DEVELOPMENT GRADUATE & TRAINING EDUCATIONAL SUPPORT New and existing Site, School School and FE 290APPRENTICESHIP and FE Visits Work Placements and trainee places + + 27,000 3,300 Professional Employment persons days 110 including GRADUATES Figures correct at end July 2017 ‰ 2 ‰ Foreword – Chairs 4 ‰ Territory Programme Director’s Report 7 ‰ Hub South East Chief Executive’s Report 10 ‰ Projects Completed 13 ‰ Contents Under Construction 23 ‰ In Development 33 ‰ Strategic Support Services 39 ‰ Performance 43 ‰ Added Value through Hub South East 50 ‰ Abstract of Accounts 53 ‰ ‰ 3 ‰ Foreword Welcome to the 2016/17 Annual Report for the South East Territory, The Territory’s Strategic vision is to work together to provide enhanced local services covering the reporting period August 2016 to July 2017. and achieve tangible benefits for partners and communities in the Lothians and Borders and we have been making real headway in delivering it. This is our seventh year in operation, and we have continued to work together to improve local services by delivering modern, high quality This year in the South East Territory, we handed over our biggest completed project, community infrastructure across the Territory. Phase 1 of the development of the Royal Edinburgh Hospital campus (P18) and broke ground on our highest value revenue funded project at the East Lothian With eight projects on site and more in development, we are sustaining a Community Hospital (P28) - the largest project to date in the Hub programme across good level of activity. -

LHB37 LOTHIAN HEALTH BOARD Introduction 1 Agenda of Meetings of Lothian Health Board, 1987-1995 2 Agenda of Meetings of Lothia
LHB37 LOTHIAN HEALTH BOARD Introduction 1 Agenda of Meetings of Lothian Health Board, 1987-1995 2 Agenda of Meetings of Lothian Health Board Committees, 1987-1989 2A Minutes of Board, Standing Committees and Sub-Committees, 1973-1986 2B Draft Minutes of Board Meetings, 1991-2001 2C [not used] 2D Area Executive Group Minutes, 1973-1986 2E Area Executive Group Agendas and Papers, 1978-1985 2F Agenda Papers for Contracts Directorate Business Meetings, 1993-1994 2G Agenda Papers of Finance, Manpower and Establishment Committee, 1975-1979 2H Agenda papers of the Policy and Commissioning Team Finance and Corporate Services Sub- Group, 1994-1995 2I [not used] 2J Minutes and Papers of the Research Ethics Sub-Committees, 1993-1995 3 Annual Reports, 1975-2004 4 Annual Reports of Director of Public Health, 1989-2008 5 Year Books, 1977-1992 6 Internal Policy Documents and Reports, 1975-2005 7 Publications, 1960-2002 8 Administrative Papers, 1973-1994 8A Numbered Administrative Files, 1968-1993 8B Numbered Registry Files, 1970-1996 8C Unregistered Files, 1971-1997 8D Files of the Health Emergency Planning Officer, 1978-1993 9 Annual Financial Reviews, 1974-1987 10 Annual Accounts, 1976-1992 10A Requests for a major item of equipment, 1987-1990 LHB37 LOTHIAN HEALTH BOARD 11 Lothian Medical Audit Committee, 1988-1997 12 Records of the Finance Department, 1976-1997 13 Endowment Fund Accounts, 1972-2004 14 Statistical Papers, 1974-1990 15 Scottish Health Service Costs, 1975-1987 16 Focus on Health , 1982-1986 17 Lothian Health News , 1973-2001 18 Press -

The Scottish Genealogist
THE SCOTTISH GENEALOGY SOCIETY THE SCOTTISH GENEALOGIST INDEX TO VOLUMES LIX-LXI 2012-2014 Published by The Scottish Genealogy Society The Index covers the years 2012-2014 Volumes LIX-LXI Compiled by D.R. Torrance 2015 The Scottish Genealogy Society – ISSN 0330 337X Contents Please click on the subject to be visited. ADDITIONS TO THE LIBRARY APPRECIATIONS ARTICLE TITLES BOOKMARKS BOOK REVIEWS CONTRIBUTORS FAMILY TREES GENERAL INDEX ILLUSTRATIONS INTRODUCTION QUERIES INTRODUCTION Where a personal or place name is mentioned several times in an article, only the first mention is indexed. LIX, LX, LXI = Volume number i. ii. iii. iv = Part number 1- = page number ; - separates part numbers within the same volume : - separates volume numbers BOOKMARKS The contents of this CD have been bookmarked. Select the second icon down at the left-hand side of the document. Use the + to expand a section and the – to reduce the selection. If this icon is not visible go to View > Show/Hide > Navigation Panes > Bookmarks. Recent Additions to the Library (compiled by Joan Keen & Eileen Elder) LIX.i.43; ii.102; iii.154: LX.i.48; ii.97; iii.144; iv.188: LXI.i.33; ii.77; iii.114; Appreciations 2012-2014 Ainslie, Fred LIX.i.46 Ferguson, Joan Primrose Scott LX.iv.173 Hampton, Nettie LIX.ii.67 Willsher, Betty LIX.iv.205 Article Titles 2012-2014 A Call to Clan Shaw LIX.iii.145; iv.188 A Case of Adultery in Roslin Parish, Midlothian LXI.iv.127 A Knight in Newhaven: Sir Alexander Morrison (1799-1866) LXI.i.3 A New online Medical Database (Royal College of Physicians) -

Services for Older People in the City of Edinburgh
Services for older people in the city of Edinburgh December 2018 Progress review following a joint inspection Contents 1. Background to this progress review 3 2. How we conducted this progress review 3 3. Progress made: what we found overview 4 4. Progress on recommendations for improvement 6 5. Conclusion and what happens next 38 Appendix 1: city of Edinburgh health and social care partnership 39 locality operational structure Appendix 2: city of Edinburgh health and social care partnership 40 planning and governance structure This report should be read alongside our original inspection report on which this progress review is based on. This can be found at: www.careinspectorate.com/images/documents/3831/Edinburgh%20services%20for %20older%20people%20joint%20inspection%20report%20May%202017.pdf The Care Inspectorate and Healthcare Improvement Scotland jointly publish this progress review report. To find out more go to www.careinspectorate.com/ or www.healthcareimprovementscotland.org/ Services for older people in the city of Edinburgh Page 2 of 40 1. Background to this progress review The Care Inspectorate and Healthcare Improvement Scotland jointly carried out an inspection of services for older people in the city of Edinburgh between October and December 2016. We published a joint inspection report in May 2017, which is available on both scrutiny bodies’ websites. The purpose of the joint inspection was to find out how well the partnership achieved good personal outcomes for older people and their unpaid carers1. The report highlighted important weaknesses and where performance was unsatisfactory. We stated that we would monitor improvement and return to the partnership to review progress in 2018. -

Astley Ainslie Hospital 1
Astley Ainslie Hospital Community Consultation Disposal Commitment Introduction The Astley Ainslie Hospital has now been declared surplus to NHS Lothian clinical strategy requirements. Services are being relocated as part of the closure process, the majority most within the nearby Royal Edinburgh Hospital campus. As part of the process of disposing of surplus assets NHS Lothian is committing to engaging with all key stakeholders, including the general public, MSP's Councilors, CEC planning department, Historic Environment Scotland and other interest groups to collate ideas and issues that are of importance to the community. Purpose of document With service re-provision still at the planning stage there is a substantial period available for community engagement prior to any disposal route being implemented. Meetings have already been held with local Community Council representatives, MSP's and the general public. The purpose of this document is to confirm NHS Lothian’s commitment to on-going engagement and to suggest a plan for the nature of this engagement and the documentation that will demonstrate the prioritised outcomes which will inform a disposal. This information will be used to create the criteria which all parties will use to establish the re-use of the land and buildings. It will form the basis of a document creating the most important development parameters for the site. This document will be formalised by way of a Development Brief containing all main development aspects and will be offered to CEC planning department for endorsement Engagement commitment • Inclusion – NHS Lothian is seeking to engage with all stakeholders to provide the widest range of interests the opportunity to provide their opinions. -

Peter Goes Back to the Floor
THE NEWSPAPER FOR NHS LOTHIAN STAFF MAY/JUNE 2008 ISSUE 26 ConnectionsYOUR AWARD-WINNING NEWSPAPER PETER GOES BACK WIN A FABULOUS TO THE FLOOR PAMPER SESSION! PAGE 14 PAGE 15 £8M CASH BOOST FOR PUBLIC HEALTH SERVICES Government cash will help board tackle alcohol and tobacco misuse NHS Lothian has been awarded dependent drinkers, more treatment £8 million to deal with specific and prevention/education services public health issues such as and appropriate recording systems. alcohol misuse, sexual health The second largest sum of THANK YOU: auxiliary nurse Fay Watt, left, has a very special reason for presenting and stopping smoking money has been awarded for flowers to her nursing colleagues – turn to page 3 to read their heart-warming tale… programmes. prevention of blood-borne viruses. Just over £3.4m has been A continuing £2.52m is to be used awarded for alcohol misuse. to reduce the spread of HIV and The Scottish Government has hepatitis. tobacco control efforts. The Scottish Government acknowledges increased alcohol misuse funding Revised performance This being the case, funding by almost 150 per cent compared management arrangements to of £911,000 is being continued for that very significant progress has to 2007/08. ensure NHS boards use the NHS Lothian to provide stop been made in reducing smoking through The additional money is to help money effectively will be provided smoking services that help NHS boards meet targets for by the end of May. people quit. comprehensive tobacco control reducing consumption and related The Scottish Government The money allocated is to go harm and the Government expects acknowledges that very towards reducing smoking in help improve the sexual programme, which tackles considerable work to be done in significant progress has been made the adult population to 22 per health of Lothian’s population, health inequalities that are this area. -

NHS Lothian Job Packs
NHS LOTHIAN Post: Band 2 Health Care Support Worker Discharge Lounge WGH PERSON SPECIFICATION In order to be shortlisted you must demonstrate you meet all the essential criteria and as much of the desirable as possible. When a large volume of applications are received for a vacancy and most applicants meet the essential criteria then the desirable criteria is used to produce the shortlist. How Criteria Essential Desirable assessed Personal Traits Caring, respectful, polite, A, I, R compassionate Good communication skills Well presented Flexible with shift pattern Qualifications Must have a good educational Healthcare qualification e.g. A, C, I and Training background and a high standard SVQ level II or III in health of written and verbal and social care communication. Experience and Evidence of ability to work within a team Previous experience within a A, I, R Knowledge Awareness of confidentiality within the caring or healthcare job remit environment Skills and/or Ability to carry out assigned tasks IT skills A, I, R Abilities effectively in a busy environment Enthusiasm to learn and Contribute and work as part of a wider develop team of healthcare professionals Good interpersonal skills particularly dealing with people either in person or on the telephone. Specific Job Ability to undertake further Evidence of further A, C, R Requirements training in SVQ II. education To work within standards set out in HCSW code of conduct Good time keeping and flexibility Involves direct contact with body fluids, on a number of occasions per shift. Key – how assessed A = Application form I = Interview C = Copies of certificates T= Test or exercise P = Presentation R = References JOB DESCRIPTION CLINICAL SUPPORT WORKER SVQ CARE LEVEL 2 (QUALIFIED) Band 2 HCSW Job Specification for General surgery – September 2013 V1 1. -

Consultant Medical Oncologist (Breast/Renal) in Cancer Services
JOB TITLE: Consultant Medical Oncologist (Breast/Renal) in Cancer Services JOB REFERENCE: CG 2054 JOBTRAIN REFERENCE: 044290 CLOSING DATE: 03 April 2021 INTERVIEW DATE: 06 May 2021 http://careers.nhslothian.scot.nhs.uk Contents Section Section 1: Person Specification Section 2: Introduction to Appointment Section 3: Departmental and Directorate Information Section 4: Main Duties and Responsibilities Section 5: Job Plan Section 6: Contact Information Section 7: Working for NHS Lothian Section 8: Terms and Conditions of Employment Section 9: General Information for Candidates Unfortunately we cannot accept CV’s as a form of application and only application forms completed via the Jobtrain system will be accepted. Please visit https://apply.jobs.scot.nhs.uk for further details on how to apply. You will receive a response acknowledging receipt of your application. This post requires the post holder to have a PVG Scheme membership/record. If the successful applicant is not a current PVG member for the required regulatory group i.e. child and/or adult, then an application will need to be made to Disclosure Scotland and deemed satisfactory before the successful post holder can commence work. All NHS Scotland and NHS Lothian Medical vacancies are advertised on our medical jobs microsite: www.medicaljobs.scot.nhs.uk Please visit our Careers website for further information on what NHS Lothian has to offer http://careers.nhslothian.scot.nhs.uk http://careers.nhslothian.scot.nhs.uk Section 1: Person Specification REQUIREMENTS ESSENTIAL DESIRABLE -

Notice of Meeting and Agenda
Planning Committee 10am, Thursday 7 August 2014 Grange Conservation Area Character Appraisal – Final Version Item number Report number Executive/routine Executive Wards Meadows/Morningside, Southside/Newington Executive summary The Grange Conservation Area Character Appraisal is the first of a series to be revised to reflect changing circumstances, community concerns and to produce a more user- friendly document. The document has resulted from an intensive programme of engagement with local community organisations and consultation within the Council. Feedback on the draft appraisal has been generally very positive. Detailed comments, concerns and suggestions have been reflected in the final version. The final version of the document is presented here for approval. Links Coalition pledges P40 Council outcomes CO19, CO23 Single Outcome Agreement SO4 Report Grange Conservation Area Character Appraisal – Final Version Recommendations 1.1 It is recommended that the committee approves the attached final version of the Grange Conservation Area Character Appraisal. Background 2.1 On 27 February 2014, the Planning Committee approved the revised Grange Conservation Area Character Appraisal in draft for consultation. Main report 3.1 Consultation on the draft appraisal ran from 12 March to 14 April 2014. An exhibition in Newington Library ran from 17 to 30 March and received about 40 visitors over the two sessions which were staffed by planning officers. Direct consultations were sent to 43 local and national interest groups. 3.2 The consultation generated 36 responses in total, 33 via the online survey and 3 directly by email. The majority of responses (31) were from individuals, mostly residents in the area. The Grange Association, Grange and Prestonfield Community Council, NHS Lothian, Falcon Bowling and Tennis Club and Carlton Cricket Club sent detailed responses. -
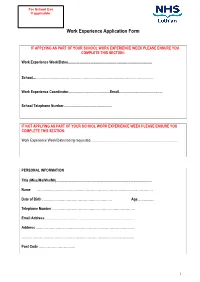
Work Experience Application Form
For School Use If applicable: Work Experience Application Form IF APPLYING AS PART OF YOUR SCHOOL WORK EXPERIENCE WEEK PLEASE ENSURE YOU COMPLETE THIS SECTION: Work Experience Week/Dates........................................................................................... School....……………………………………………………………………………………………. Work Experience Coordinator.............................................Email............................................... School Telephone Number.................................................... IF NOT APPLYING AS PART OF YOUR SCHOOL WORK EXPERIENCE WEEK PLEASE ENSURE YOU COMPLETE THIS SECTION: Work Experience Week/Dates being requested............................................................................................. PERSONAL INFORMATION Title (Miss/Ms/Mrs/Mr)....................................................................................................... Name …………………………………………………………………………………………… Date of Birth ……………………………………………………… Age.................. Telephone Number ………………………………………………………………… Email Address ……………………………………………………………………… Address ……………………………………………………………………………… ………………………………………………………………………………………… Post Code …………………………… 1 PLEASE INDICATE YOUR CHOSEN CAREER PATH …………………………………………………………………………………………. Please indicate your choice of placement and list your 1. preference in order (e.g. midwifery, cardiology) 2. 3. PLEASE INDICATE THE LOCATIONS YOU CAN CONSIDER Placement Location: using numbers (1 being your first choice, 2 being your second choice, etc) please mark all the areas that you could -

Lothian NHS Board Waverley Gate 2-4 Waterloo Place Edinburgh EH1 3EG
Lothian NHS Board Waverley Gate 2-4 Waterloo Place Edinburgh EH1 3EG Telephone: 0131 536 9000 www.nhslothian.scot.nhs.uk www.nhslothian.scot.nhs.uk Date: 14/10/2020 Your Ref: Our Ref: 4687 Enquiries to : Richard Mutch Extension: 35687 Direct Line: 0131 465 5687 [email protected] [email protected] Dear FREEDOM OF INFORMATION –THEATRES I write in response to your request for information in relation to theatres within NHS Lothian. Question: 1. Please list the number of surgical theatres (including day case) at each of the following hospital sites. Answer: Royal Infirmary of Edinburgh 28 Liberton Hospital 0 Western General Hospital 9 St John’s Hospital 13 Question: 2. Please list the number of induction rooms (including day case) at each of the following hospital sites. Answer: Royal Infirmary of Edinburgh 28 Liberton Hospital 0 Western General Hospital 9 St John’s Hospital 12 Question: 3. Please provide a list detailing the manufacturer, model and year of purchase for all anaesthesia machines currently in operation at each of the following hospital sites. Answer: Royal Infirmary of Edinburgh Enclosed table Liberton Hospital 0 Western General Hospital Enclosed table St John’s Hospital Enclosed table 4687 – Theatres - October 2020 Question: 4. Please provide the name of the clinical equipment lead for anaesthetic machines? (Usually an anaesthetist). Please could you provide the information broken down to each Hospital named above and not Trust wide. Answer: Royal Infirmary of Edinburgh , Anaesthetic Clinical Director Liberton Hospital N/A Western General Hospital , Anaesthetic Clinical Director St John’s Hospital , Anaesthetic Clinical Director I hope the information provided helps with your request. -

The Scottish Genealogist
THE SCOTTISH GENEALOGY SOCIETY THE SCOTTISH GENEALOGIST INDEX TO VOLUMES LIX-LXI 2012-2014 Published by The Scottish Genealogy Society The Index covers the years 2012-2014 Volumes LIX-LXI Compiled by D.R. Torrance 2015 The Scottish Genealogy Society – ISSN 0330 337X Contents Appreciations 1 Article Titles 1 Book Reviews 3 Contributors 4 Family Trees 5 General Index 9 Illustrations 6 Queries 5 Recent Additions to the Library 5 INTRODUCTION Where a personal or place name is mentioned several times in an article, only the first mention is indexed. LIX, LX, LXI = Volume number i. ii. iii. iv = Part number 1- = page number ; - separates part numbers within the same volume : - separates volume numbers Appreciations 2012-2014 Ainslie, Fred LIX.i.46 Ferguson, Joan Primrose Scott LX.iv.173 Hampton, Nettie LIX.ii.67 Willsher, Betty LIX.iv.205 Article Titles 2012-2014 A Call to Clan Shaw LIX.iii.145; iv.188 A Case of Adultery in Roslin Parish, Midlothian LXI.iv.127 A Knight in Newhaven: Sir Alexander Morrison (1799-1866) LXI.i.3 A New online Medical Database (Royal College of Physicians) LX.iv.177 A very short visit to Scotslot LIX.iii.144 Agnes de Graham, wife of John de Monfode, and Sir John Douglas LXI.iv.129 An Octogenarian Printer’s Recollections LX.iii.108 Ancestors at Bannockburn LXI.ii.39 Andrew Robertson of Gladsmuir LIX.iv.159: LX.i.31 Anglo-Scottish Family History Society LIX.i.36 Antiquarian is an odd name for a society LIX.i.27 Balfours of Balbirnie and Whittinghame LX.ii.84 Battle of Bannockburn Family History Project LXI.ii.47 Bothwells’ Coat-of-Arms at Glencorse Old Kirk LX.iv.156 Bridges of Bishopmill, Elgin LX.i.26 Cadder Pit Disaster LX.ii.69 Can you identify this wedding party? LIX.iii.148 Candlemakers of Edinburgh LIX.iii.139 Captain Ronald Cameron, a Dungallon in Morven & N.