Mycobacterium Africanum
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Phylogenomic Analysis of the Species of the Mycobacterium Tuberculosis
Phylogenomic analysis of the species of the Mycobacterium tuberculosis complex demonstrates that Mycobacterium africanum, Mycobacterium bovis, Mycobacterium caprae, Mycobacterium microti and Mycobacterium pinnipedii are later heterotypic synonyms of Mycobacterium tuberculosis Marco Riojas, Katya Mcgough, Cristin Rider-Riojas, Nalin Rastogi, Manzour Hernando Hazbón To cite this version: Marco Riojas, Katya Mcgough, Cristin Rider-Riojas, Nalin Rastogi, Manzour Hernando Hazbón. Phy- logenomic analysis of the species of the Mycobacterium tuberculosis complex demonstrates that My- cobacterium africanum, Mycobacterium bovis, Mycobacterium caprae, Mycobacterium microti and Mycobacterium pinnipedii are later heterotypic synonyms of Mycobacterium tuberculosis. Inter- national Journal of Systematic and Evolutionary Microbiology, Microbiology Society, 2018, 68 (1), pp.324-332. 10.1099/ijsem.0.002507. pasteur-01986654 HAL Id: pasteur-01986654 https://hal-riip.archives-ouvertes.fr/pasteur-01986654 Submitted on 18 Jan 2019 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. RESEARCH ARTICLE Riojas et al., Int J Syst Evol Microbiol 2018;68:324–332 DOI 10.1099/ijsem.0.002507 Phylogenomic analysis of the species of the Mycobacterium tuberculosis complex demonstrates that Mycobacterium africanum, Mycobacterium bovis, Mycobacterium caprae, Mycobacterium microti and Mycobacterium pinnipedii are later heterotypic synonyms of Mycobacterium tuberculosis Marco A. -

A Simple and Efficient Multiplex PCR Assay for the Identification of Mycobacteriumgenus and Mycobacterium Tuberculosis Complex T
http://dx.doi.org/10.3349/ymj.2013.54.5.1220 Original Article pISSN: 0513-5796, eISSN: 1976-2437 Yonsei Med J 54(5):1220-1226, 2013 A Simple and Efficient Multiplex PCR Assay for the Identification ofMycobacterium Genus and Mycobacterium tuberculosis Complex to the Species Level Yeun Kim,1 Yeonim Choi,1 Bo-Young Jeon,1 Hyunwoo Jin,1,2 Sang-Nae Cho,3 and Hyeyoung Lee1 1Department of Biomedical Laboratory Science, College of Health Sciences, Yonsei University, Wonju; 2Department of Clinical Laboratory Science, College of Health Sciences, Catholic University of Pusan, Busan; 3Department of Microbiology, Yonsei University College of Medicine, Seoul, Korea. Received: September 19, 2012 Purpose: The Mycobacterium tuberculosis complex comprises M. tuberculosis, Revised: October 25, 2012 M. bovis, M. bovis bacillus Calmette-Guérin (BCG) and M. africanum, and causes Accepted: October 29, 2012 tuberculosis in humans and animals. Identification of Mycobacterium spp. and M. Corresponding author: Dr. Hyeyoung Lee, tuberculosis complex to the species level is important for practical use in microbi- Department of Biomedical Laboratory Science, College of Health Sciences, Yonsei University, ological laboratories, in addition to optimal treatment and public health. Materials 1 Yonseidae-gil, Wonju 220-710, Korea. and Methods: A novel multiplex PCR assay targeting a conserved rpoB sequence Tel: 82-33-760-2740, Fax: 82-33-760-2561 in Mycobacteria spp., as well as regions of difference (RD) 1 and RD8, was devel- E-mail: [email protected] oped and evaluated using 37 reference strains and 178 clinical isolates. Results: All mycobacterial strains produced a 518-bp product (rpoB), while other bacteria ∙ The authors have no financial conflicts of produced no product. -

Nontuberculous Mycobacterial Species and Mycobacterium Tuberculosis Complex Coinfection in Patients with Pulmonary Tuberculosis in Dr
[Downloaded free from http://www.ijmyco.org on Saturday, September 28, 2019, IP: 210.57.215.50] Original Research Article Nontuberculous Mycobacterial Species and Mycobacterium Tuberculosis Complex Coinfection in Patients with Pulmonary Tuberculosis in Dr. Soetomo Hospital, Surabaya, Indonesia Ni Made Mertaniasih1,2, Deby Kusumaningrum1,2, Eko Budi Koendhori1,2, Soedarsono3, Tutik Kusmiati3, Desak Nyoman Surya Suameitria Dewi2 Departments of 1Clinical Microbiology and 3Pulmonology, Faculty of Medicine, Airlangga University, Dr. Soetomo Hospital, Surabaya 60131, 2Institute of Tropical Disease, Airlangga University, Surabaya 60115, Indonesia Abstract Objective/Background: The aim of this study was to analyze the detection of nontuberculous mycobacterial (NTM) species derived from sputum specimens of pulmonary tuberculosis (TB) suspects. Increasing prevalence and incidence of pulmonary infection by NTM species have widely been reported in several countries with geographical variation. Materials and Methods: Between January 2014 and September 2015, sputum specimens from chronic pulmonary TB suspect patients were analyzed. Laboratory examination of mycobacteria was conducted in the TB laboratory, Department of Clinical Microbiology, Dr. Soetomo Hospital, Surabaya. Detection and identification of mycobacteria were performed by the standard culture method using the BACTEC MGIT 960 system (BD) and Lowenstein–Jensen medium. Identification of positive Mycobacterium tuberculosis complex (MTBC) was based on positive acid-fast bacilli microscopic smear, positive niacin accumulation, and positive TB Ag MPT 64 test results (SD Bioline). If the growth of positive cultures and acid-fast bacilli microscopic smear was positive, but niacin accumulation and TB Ag MPT 64 (SD Bioline) results were negative, then the isolates were categorized as NTM species. MTBC isolates were also tested for their sensitivity toward first-line anti-TB drugs, using isoniazid, rifampin, ethambutol, and streptomycin. -

Nucleic Acid Sequences Specific for Mycobacterium Kansasii
Europaisches Patentamt 19 European Patent Office Office europeen des brevets (n) Publication number : 0 669 402 A2 12 EUROPEAN PATENT APPLICATION @ Application number: 95301106.1 @ Int. CI.6: C12Q 1/68, // (C12Q1/68, C12R1 .32) (§) Date of filing : 21.02.95 (30) Priority : 28.02.94 US 203534 @ Inventor : Spears, Patricia A. 8605 Carol ingian Court @ Date of publication of application : Raleigh, North Carolina 27615 (US) 30.08.95 Bulletin 95/35 Inventor : Shank, Daryl D. 1213 Basil Court @ Designated Contracting States : Bel Air, Maryland 21014 (US) DE FR GB IT NL SE (74) Representative : Ruffles, Graham Keith (7i) Applicant : Becton Dickinson and Company MARKS & CLERK, One Becton Drive 57-60 Lincoln's Inn Fields Franklin Lakes, New Jersey 07417-1880 (US) London WC2A 3LS (GB) (54) Nucleic acid sequences specific for mycobacterium kansasii. (57) Oligonucleotide probes and primers which exhibit M. /ransas/f-specificity in nucleic acid hybridization assays and in nucleic acid amplifi- cation reactions. The full-length M. kan- sasff-specific sequence, identified herein as o o clone MK7, is 493 base pairs in length and has a I GC content of 63%. Several M. kansasii-spec\f\c subsequences of MK7 are also provided. The > probes and primers are useful in assays for > species-specific detection and identification of M. kansasii. oa o > >CD o > CM < CM <~> O O o> CO CO LU Jouve, 18, rue Saint-Denis, 75001 PARIS EP 0 669 402 A2 FIELD OF THE INVENTION The present invention relates to oligonucleotide probes and amplification primers, and particularly relates to oligonucleotide probes and primers which hybridize in a species-specific manner to Mycobacterium kansasii 5 nucleic acids. -

Association of Mycobacterium Africanum Infection with Slower Disease Progression Compared with Mycobacterium Tuberculosis in Malian Patients with Tuberculosis
Am. J. Trop. Med. Hyg., 102(1), 2020, pp. 36–41 doi:10.4269/ajtmh.19-0264 Copyright © 2020 by The American Society of Tropical Medicine and Hygiene Association of Mycobacterium africanum Infection with Slower Disease Progression Compared with Mycobacterium tuberculosis in Malian Patients with Tuberculosis Bocar Baya,1* Bassirou Diarra,1 Seydou Diabate,1 Bourahima Kone,1 Drissa Goita,1 Yeya dit Sadio Sarro,1 Keira Cohen,2 Jane L. Holl,3 Chad J. Achenbach,3 Mohamed Tolofoudie,1 Antieme Combo Georges Togo,1 Moumine Sanogo,1 Amadou Kone,1 Ousmane Kodio,1 Djeneba Dabitao,1 Nadie Coulibaly,1 Sophia Siddiqui,4 Samba Diop,1 William Bishai,2 Sounkalo Dao,1 Seydou Doumbia,1 Robert Leo Murphy,3 Souleymane Diallo,1 and Mamoudou Maiga1,3 1University Clinical Research Center (UCRC)–SEREFO Laboratory-University of Sciences, Techniques and Technologies of Bamako (USTTB), Bamako, Mali; 2Johns Hopkins University School of Medicine, Baltimore, Maryland; 3Northwestern University, Chicago, Illinois; 4National Institutes of Allergic and Infectious Diseases (NIAID), Rockville, Maryland Abstract. Mycobacterium africanum (MAF) is known to endemically cause up to 40–50% of all pulmonary TB in West Africa. The aim of this study was to compare MAF with Mycobacterium tuberculosis (MTB) with regard to time from symptom onset to TB diagnosis, and clinical and radiological characteristics. A cross-sectional study was conducted in Bamako, Mali, between August 2014 and July 2016. Seventy-seven newly diagnosed pulmonary TB patients who were naive to treatment were enrolled at Mali’s University Clinical Research Center. Sputum cultures were performed to confirm the diagnosis and spoligotyping to identify the mycobacterial strain. -
The Impact of Chlorine and Chloramine on the Detection and Quantification of Legionella Pneumophila and Mycobacterium Spp
The impact of chlorine and chloramine on the detection and quantification of Legionella pneumophila and Mycobacterium spp. Maura J. Donohue Ph.D. Office of Research and Development Center of Environmental Response and Emergency Response (CESER): Water Infrastructure Division (WID) Small Systems Webinar January 28, 2020 Disclaimer: The views expressed in this presentation are those of the author and do not necessarily reflect the views or policies of the U.S. Environmental Protection Agency. A Tale of Two Bacterium… Legionellaceae Mycobacteriaceae • Legionella (Genus) • Mycobacterium (Genus) • Gram negative bacteria • Nontuberculous Mycobacterium (NTM) (Gammaproteobacteria) • M. avium-intracellulare complex (MAC) • Flagella rod (2-20 µm) • Slow grower (3 to 10 days) • Gram positive bacteria • Majority of species will grow in free-living • Rod shape(1-10 µm) amoebae • Non-motile, spore-forming, aerobic • Aerobic, L-cysteine and iron salts are required • Rapid to Slow grower (1 week to 8 weeks) for in vitro growth, pH: 6.8 to 7, T: 25 to 43 °C • ~156 species • ~65 species • Some species capable of causing disease • Pathogenic or potentially pathogenic for human 3 NTM from Environmental Microorganism to Opportunistic Opponent Genus 156 Species Disease NTM =Nontuberculous Mycobacteria MAC = M. avium Complex Mycobacterium Mycobacterium duvalii Mycobacterium litorale Mycobacterium pulveris Clinically Relevant Species Mycobacterium abscessus Mycobacterium elephantis Mycobacterium llatzerense. Mycobacterium pyrenivorans, Mycobacterium africanum Mycobacterium europaeum Mycobacterium madagascariense Mycobacterium rhodesiae Mycobacterium agri Mycobacterium fallax Mycobacterium mageritense, Mycobacterium riyadhense Mycobacterium aichiense Mycobacterium farcinogenes Mycobacterium malmoense Mycobacterium rufum M. avium, M. intracellulare, Mycobacterium algericum Mycobacterium flavescens Mycobacterium mantenii Mycobacterium rutilum Mycobacterium alsense Mycobacterium florentinum. Mycobacterium marinum Mycobacterium salmoniphilum ( M. fortuitum, M. -

Complications in the Study of Ancient Tuberculosis: Presence of Environmental Bacteria in Human Archaeological Remains
Journal of Archaeological Science 68 (2016) 5e11 Contents lists available at ScienceDirect Journal of Archaeological Science journal homepage: http://www.elsevier.com/locate/jas Complications in the study of ancient tuberculosis: Presence of environmental bacteria in human archaeological remains * Romy Müller a, Charlotte A. Roberts b, Terence A. Brown a, a Faculty of Life Sciences, Manchester Institute of Biotechnology, University of Manchester, 131 Princess Street, Manchester M1 7DN, UK b Department of Archaeology, Durham University, South Road, Durham DH1 3LE, UK article info abstract Article history: There are many reports of ancient DNA from bacteria of the Mycobacterium tuberculosis complex (MTBC) Received 16 October 2015 being present in skeletons with and without osteological indications of tuberculosis. A possible Received in revised form complication in these studies is that extracts might also contain DNA from the microbiome of the in- 22 February 2016 dividual whose remains are being analysed and/or from environmental bacteria that have colonised the Accepted 1 March 2016 skeleton after death. These contaminants might include ‘mycobacteria other than tuberculosis’ (MOTT), which are common in the environment, but which are not normally associated with clinical cases of tuberculosis. In this paper we show that MOTT of various types, as well as bacteria of related genera, are Keywords: Ancient DNA present in most if not all archaeological remains. Our results emphasise the complications inherent in the fi Authenticity of sequence data biomolecular study of archaeological human tuberculosis. The speci city of any polymerase chain re- Mycobacteria other than tuberculosis action directed at the MTBC cannot be assumed and, to confirm that an amplification is authentic, a Mycobacterium tuberculosis complex sequencing strategy must be applied that allows characterisation of the PCR product. -

Mycobacterium Tuberculosis
JOURNAL OF CLINICAL MICROBIOLOGY, Oct. 1990, p. 2200-2204 Vol. 28, No. 10 0095-1137/90/102200-05$02.00/0 Copyright © 1990, American Society for Microbiology Polymerase Chain Reaction for Detection of Mycobacterium tuberculosis ULF SJOBRING,l MICHAEL MECKLENBURG,"2 ASE BENGÂRD ANDERSEN,3 AND HÂKAN MIORNERl* Department of Medical Microbiologyl and Department ofPure and Applied Biochemistry,2 University ofLund, Lund, Sweden, and Mycobacteria Department, Statens Seruminstitut, Copenhagen, Denmark3 Received 6 March 1990/Accepted 25 June 1990 A polymerase chain reaction for the specific detection of mycobacteria belonging to the Mycobacterium tuberculosis complex was developed. Using a single primer pair derived from the nucleotide sequence of protein antigen b of M. tuberculosis, we achieved specific amplification of a 419-base-pair DNA fragment in M. tuberculosis and M. bovis. After DNA was extracted from mycobacteria by using a simple, safe lysis procedure, we detected the 419-base-pair sequence in samples containing few mycobacteria. Preliminary data suggested that this technique could be applied to clinical specimens for early and specific diagnosis of tuberculosis. Several mycobacterial species are associated with dis- to detect DNAs extracted from various mycobacteria (3, 7). eases in humans. Tuberculosis is caused by Mycobacterium The latter application is based on the sequences of the heat tuberculosis, Mycobacterium africanum, or Mycobacterium shock proteins of M. bovis bacillus Calmette-Guérin (BCG) bovis and is a major health problem, particularly in devel- (21) and M. tuberculosis (18). These sequences are shared by oping countries. The number of cases of tuberculosis world- many other species, and labeled probes are required to wide is estimated to be some 30 million, with an annual identify amplified DNA specific for M. -

Sulfatase-Activated Fluorophores for Rapid Discrimination Of
Sulfatase-activated fluorophores for rapid discrimination of mycobacterial species and strains Kimberly E. Beattya,1, Monique Williamsb,c, Brian L. Carlsona, Benjamin M. Swartsa, Robin M. Warrenb, Paul D. van Heldenb, and Carolyn R. Bertozzia,d,2 aDepartments of Chemistry and Molecular and Cell Biology, and dHoward Hughes Medical Institute, University of California, Berkeley, CA 94720-1460; bDivision of Molecular Biology and Human Genetics, National Research Foundation Centre of Excellence for Biomedical Tuberculosis Research/Medical Research Council Centre for Molecular and Cellular Biology, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town 7505, South Africa; and cMedical Research Council/National Health Laboratory Service/University of Cape Town Molecular Mycobacteriology Research Unit, Institute of Infectious Diseases and Molecular Medicine, University of Cape Town, Cape Town 7925, South Africa Edited by Laura L. Kiessling, University of Wisconsin-Madison, Madison, WI, and approved June 7, 2013 (received for review January 4, 2013) Most current diagnostic tests for tuberculosis do not reveal the colorimetric sulfatase substrate phenolphthalein disulfate (17). species or strain of pathogen causing pulmonary infection, which Species and strain identification using this and other sulfatase can lead to inappropriate treatment regimens and the spread of probes [e.g., p-nitrophenyl sulfate (p-NPS) (18) and 4-methyl- disease. Here, we report an assay for mycobacterial strain assign- umbelliferyl sulfate (4-MUS) (19); structures are shown in SI ment based on genetically conserved mycobacterial sulfatases. We Appendix, Fig. S1] have been largely ineffective due to slow re- developed a sulfatase-activated probe, 7-hydroxy-9H-(1,3-dichloro- action kinetics, a high detection limit with these substrates, and 9,9-dimethylacridin-2-one)–sulfate, that detects enzyme activity in the lack of a simple platform to resolve strain-specific enzymes. -
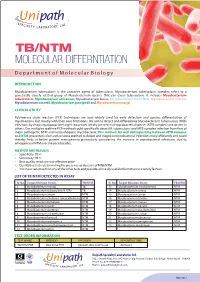
TB/NTM MOLECULAR DIFFERNTIATION D E P a R T M E N T O F M O L E C U L a R B I O L O G Y
TB/NTM MOLECULAR DIFFERNTIATION D e p a r t m e n t o f M o l e c u l a r B i o l o g y INTRODUCTION Mycobacterium tuberculosis is the causative agent of tuberculosis. Mycobacterium tuberculosis complex refers to a genetically closely related group of Mycobacterium species that can cause tuberculosis. It includes Mycobacterium tuberculosis, Mycobacterium africanum, Mycobacterium bovis, Mycobacterium bovis BCG, Mycobacterium microti, Mycobacterium canettii, Mycobacterium pinnipedii and Mycobacterium mungi. CLINICAL UTILITY Polymerase chain reaction (PCR) techniques are now widely used for early detection and species differentiation of mycobacteria, but mostly with their own limitations. We aim to detect and differentiate Mycobacterium tuberculosis (Mtb) infections by choosing appropriate target sequences, ideally present in all mycobacterial species (MTB complex) and absent in others. Our multiplex realtime PCR method could specifically detect M. tuberculosis and MTB complex infection from that of major pathogenic NTM and nonpathogenic mycobacteria. This method, by well distinguishing between MTB complex and NTM, presented a fast and accurate method to detect and diagnose mycobacterial infections more efficiently and could thereby help in better patient management particularly considering the increase in mycobacterial infections due to emergence of NTM over the past decades. METHOD AND RESULTS • Specificity: 99 % • Sensitivity: 98 % • Best quality results in cost-effective price • Qualitative test is determining the presence or absence of MTB/NTM. • It is more sensitive than any of the other tests and provides clinically useful information in a timely fashion LIST OF TB/NTM DETECTED IN ASSAY Sr No. Target Microbe Strain TB/NTM Sr No. -

Tuberculosis in Nonhuman Primates - the Disease 2 3 K
1 Tuberculosis in Nonhuman Primates - the disease 2 3 K. Mätz-Rensing and F.-J. Kaup 4 {German Primate Centre, Göttingen, Germany} 5 Correspondence to: K. Mätz-Rensing ([email protected]) 6 7 1 Introduction 8 Simian tuberculosis is one of the most important bacterial diseases of nonhuman primates 9 because of its ubiquitous and insidious nature and its ability to spread rapidly. Outbreaks of 10 tuberculosis have been reported in nonhuman primate colonies almost as long as primates 11 have been used as experimental animals or kept in zoological gardens. The tuberculous 12 monkey is a health hazard especially to other monkeys in the group, but (re)transmission of 13 the infection to humans has been reported as well. Significant progress has been made in 14 reducing the incidence of tuberculosis in captive nonhuman primates. In spite of reasonable 15 precautions, outbreaks continue to occur and tuberculosis remains a serious threat to the 16 health of nonhuman primates and their caretakers. Outbreaks have severe economic 17 consequences due to animal losses, disruption of research and costs related to disease control. 18 Therefore, persons working with nonhuman primates should be familiar with the disease and 19 preventive measurements. 20 21 2 The agent 22 Tuberculosis and mycobacteriosis are fatal diseases of New and Old World monkeys causing 23 high morbidity and mortality (Bennett et al., 1998; Brack, 1987). Simian tuberculosis is a 24 disease most often contracted from humans. Most of the clinical cases are induced by 25 Mycobacterium (M.) tuberculosis, but the incidence of M. bovis infections is increasing (Keet 26 et al., 1996; Stetter et al., 1995; Thorel et al., 1998; Zumpe et al., 1980). -

M. Bovis and M
UNIVERSIDAD COMPLUTENSE DE MADRID FACULTAD DE VETERINARIA Departamento de Sanidad Animal CENTRO DE VIGILANCIA SANITARIA VETERINARIA (VISAVET) Servicio de Micobacterias TESIS DOCTORAL EPIDEMIOLOGÍA MOLECULAR DE MYCOBACTERIUM BOVIS Y MYCOBACTERIUM CAPRAE EN ESPAÑA MEMORIA PARA OPTAR AL GRADO DE DOCTOR EUROPEO PRESENTADA POR Sabrina Rodríguez Campos Bajo la dirección de los doctores: Alicia Aranaz Martín Ana Mateos García Lucas Domínguez Rodríguez Madrid, 2012 ISBN: 978-84-616-1980-1 © Sabrina Rodríguez Campos Dña. Alicia Aranaz Martín, Profesora Contratada Doctor, Dña. Ana Mateos García, Profesora Titular, y D. Lucas Domínguez Rodríguez, Catedrático, del Departamento de Sanidad Animal de la Facultad de Veterinaria de la Universidad Complutense CERTIFICAN: Que la tesis doctoral que lleva por título “Epidemiología molecular de Mycobacterium bovis y Mycobacterium caprae en España” ha sido realizada por la licenciada en Veterinaria Dña. Sabrina Rodríguez Campos en el Departamento de Sanidad Animal de la Facultad de Veterinaria y en el Centro de Vigilancia Sanitaria Veterinaria de la Universidad Complutense bajo nuestra dirección, y estimamos que reúne los requisitos exigidos para optar al título de Doctor Europeo por la Universidad Complutense. Fdo. Alicia Aranaz Fdo. Ana Mateos Fdo. Lucas Domínguez En muchas ocasiones se ha hecho énfasis en la importancia de la colaboración entre científicos y políticos para el avance de los programas de erradicación (Task Force Bovine Tuberculosis Subgroup, 2006; Proceedings of the 4th International Conference on Mycobacterium bovis, 2006); la presente tesis doctoral es el resultado de la implicación y dedicación de muchas personas e instituciones, destacando el Ministerio de Medio Ambiente y Medio Rural y Marino y la Red Española de Vigilancia y Control de la Tuberculosis en Animales.