Vitiligo Treatment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Drug Name Plate Number Well Location % Inhibition, Screen Axitinib 1 1 20 Gefitinib (ZD1839) 1 2 70 Sorafenib Tosylate 1 3 21 Cr
Drug Name Plate Number Well Location % Inhibition, Screen Axitinib 1 1 20 Gefitinib (ZD1839) 1 2 70 Sorafenib Tosylate 1 3 21 Crizotinib (PF-02341066) 1 4 55 Docetaxel 1 5 98 Anastrozole 1 6 25 Cladribine 1 7 23 Methotrexate 1 8 -187 Letrozole 1 9 65 Entecavir Hydrate 1 10 48 Roxadustat (FG-4592) 1 11 19 Imatinib Mesylate (STI571) 1 12 0 Sunitinib Malate 1 13 34 Vismodegib (GDC-0449) 1 14 64 Paclitaxel 1 15 89 Aprepitant 1 16 94 Decitabine 1 17 -79 Bendamustine HCl 1 18 19 Temozolomide 1 19 -111 Nepafenac 1 20 24 Nintedanib (BIBF 1120) 1 21 -43 Lapatinib (GW-572016) Ditosylate 1 22 88 Temsirolimus (CCI-779, NSC 683864) 1 23 96 Belinostat (PXD101) 1 24 46 Capecitabine 1 25 19 Bicalutamide 1 26 83 Dutasteride 1 27 68 Epirubicin HCl 1 28 -59 Tamoxifen 1 29 30 Rufinamide 1 30 96 Afatinib (BIBW2992) 1 31 -54 Lenalidomide (CC-5013) 1 32 19 Vorinostat (SAHA, MK0683) 1 33 38 Rucaparib (AG-014699,PF-01367338) phosphate1 34 14 Lenvatinib (E7080) 1 35 80 Fulvestrant 1 36 76 Melatonin 1 37 15 Etoposide 1 38 -69 Vincristine sulfate 1 39 61 Posaconazole 1 40 97 Bortezomib (PS-341) 1 41 71 Panobinostat (LBH589) 1 42 41 Entinostat (MS-275) 1 43 26 Cabozantinib (XL184, BMS-907351) 1 44 79 Valproic acid sodium salt (Sodium valproate) 1 45 7 Raltitrexed 1 46 39 Bisoprolol fumarate 1 47 -23 Raloxifene HCl 1 48 97 Agomelatine 1 49 35 Prasugrel 1 50 -24 Bosutinib (SKI-606) 1 51 85 Nilotinib (AMN-107) 1 52 99 Enzastaurin (LY317615) 1 53 -12 Everolimus (RAD001) 1 54 94 Regorafenib (BAY 73-4506) 1 55 24 Thalidomide 1 56 40 Tivozanib (AV-951) 1 57 86 Fludarabine -

Patent Application Publication ( 10 ) Pub . No . : US 2019 / 0192440 A1
US 20190192440A1 (19 ) United States (12 ) Patent Application Publication ( 10) Pub . No. : US 2019 /0192440 A1 LI (43 ) Pub . Date : Jun . 27 , 2019 ( 54 ) ORAL DRUG DOSAGE FORM COMPRISING Publication Classification DRUG IN THE FORM OF NANOPARTICLES (51 ) Int . CI. A61K 9 / 20 (2006 .01 ) ( 71 ) Applicant: Triastek , Inc. , Nanjing ( CN ) A61K 9 /00 ( 2006 . 01) A61K 31/ 192 ( 2006 .01 ) (72 ) Inventor : Xiaoling LI , Dublin , CA (US ) A61K 9 / 24 ( 2006 .01 ) ( 52 ) U . S . CI. ( 21 ) Appl. No. : 16 /289 ,499 CPC . .. .. A61K 9 /2031 (2013 . 01 ) ; A61K 9 /0065 ( 22 ) Filed : Feb . 28 , 2019 (2013 .01 ) ; A61K 9 / 209 ( 2013 .01 ) ; A61K 9 /2027 ( 2013 .01 ) ; A61K 31/ 192 ( 2013. 01 ) ; Related U . S . Application Data A61K 9 /2072 ( 2013 .01 ) (63 ) Continuation of application No. 16 /028 ,305 , filed on Jul. 5 , 2018 , now Pat . No . 10 , 258 ,575 , which is a (57 ) ABSTRACT continuation of application No . 15 / 173 ,596 , filed on The present disclosure provides a stable solid pharmaceuti Jun . 3 , 2016 . cal dosage form for oral administration . The dosage form (60 ) Provisional application No . 62 /313 ,092 , filed on Mar. includes a substrate that forms at least one compartment and 24 , 2016 , provisional application No . 62 / 296 , 087 , a drug content loaded into the compartment. The dosage filed on Feb . 17 , 2016 , provisional application No . form is so designed that the active pharmaceutical ingredient 62 / 170, 645 , filed on Jun . 3 , 2015 . of the drug content is released in a controlled manner. Patent Application Publication Jun . 27 , 2019 Sheet 1 of 20 US 2019 /0192440 A1 FIG . -

Pharmaceuticals As Environmental Contaminants
PharmaceuticalsPharmaceuticals asas EnvironmentalEnvironmental Contaminants:Contaminants: anan OverviewOverview ofof thethe ScienceScience Christian G. Daughton, Ph.D. Chief, Environmental Chemistry Branch Environmental Sciences Division National Exposure Research Laboratory Office of Research and Development Environmental Protection Agency Las Vegas, Nevada 89119 [email protected] Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada Why and how do drugs contaminate the environment? What might it all mean? How do we prevent it? Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada This talk presents only a cursory overview of some of the many science issues surrounding the topic of pharmaceuticals as environmental contaminants Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada A Clarification We sometimes loosely (but incorrectly) refer to drugs, medicines, medications, or pharmaceuticals as being the substances that contaminant the environment. The actual environmental contaminants, however, are the active pharmaceutical ingredients – APIs. These terms are all often used interchangeably Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada Office of Research and Development Available: http://www.epa.gov/nerlesd1/chemistry/pharma/image/drawing.pdfNational -

Vitiligo AHM
Vitiligo AHM Clinical indication Any one of the following established methods for the treatment of Vitiligo is considered medically necessary : o Excimer laser (e.g., XTRAC, PhotoMedex, Radnor, PA; EX-308, Ra Medical Systems, Inc., Carlsbad, CA) o Narrow-band ultraviolet B (UVB) o Topical and oral psoralen photochemotherapy (PUVA) Note: Continued PUVA or narrow-band UVB therapy is not medically necessary unless there is significant follicular pigmentation after 6 months of therapy (8 to 10 treatments per month) o Topical and systemic corticosteroids Indications considered Not Medically Necessary Treatments for vitiligo are considered cosmetic if they do not affect the underlying condition and do not result in improved protection against skin cancer; specifically micropigmentation (tattooing) and depigmentation (with monobenzylether of hydroquinone/monobenzone) are considered cosmetic. The following treatments for the condition vitiligo are considered not medically necessary as there is a lack of evidence regarding the safety and effectiveness have not been established o Home phototherapy o Melanocyte transplantation/cultured and non-cultured cellular melanocyte keratinocyte transfer for the treatment of vitiligo o Vitamin D analogs (e.g., calcitriol and paricalcitol) o Tumor necrosis factor-alpha agents (e.g., adalimumab, etanercept, and infliximab) o Alpha-melanocyte stimulating hormone (e.g., afamelanotide) o Chimeric monoclonal antibody to CD20 (e.g., rituximab) o Autologous mini-punching grafting, blister roof grafting (suction epidermal blister grafting) and split thickness skin grafting AC-AEVITI082014 Page 1 of 5 Copyright 2016 No part of this document may be reproduced without permission ActiveHealth Management Medical Management Guidelines References: 1. Grimes PE. Diseases of hypopigmentation. In: Principles and Practice of Dermatology. -

Mortar & Pestle
Nebraska January/February 2020 | Volume 83, Number 1 MORTAR & PESTLE Official Publication of theNebraska Pharmacists Association Pam Miller 2020 NPA President Member Spotlight - Sabrina Beck | Pg 6 For NPA Members Vitiligo & Treatment Options | Pg 8 Rx and The Law | Pg 17 Baqsimi - New Delivery for Glucagon | Pg 18 Financial Forum | Pg 26 Trelegy - New Triple Therapy | Pg 28 Nebraska MORTAR & PESTLE CPE Programs npharm.org/npacpeprograms Fraud, Waste, and Abuse USP Chapter <800> Handling Hazardous Drugs in 1.0 hour Knowledge-based CPE Activity Healthcare Setting: Considerations for STERILE Products $10 NPA Member | $20 NonMember and Compounding 1.0 hour Knowledge-based CPE Activity How to Engage Your Senators: You Can Make $25 NPA Member | $50 NonMember a Difference 1.0 hour Knowledge-based CPE Activity USP Chapter <800> Handling Hazardous Drugs in $0 NPA Member | $25 NonMember Healthcare Setting: Considerations for Non-Sterile Products and Compounding Nicotine Cessation Counseling: A Guide for Pharmacists 1.0 hour Knowledge-based CPE Activity 2.0 hours Knowledge-based CPE Activity $25 NPA Member | $50 NonMember $25 NPA Member | $50 NonMember Risky Business: Assessment of Risk on Hazardous Drugs 1.0 hour Knowledge-based CPE Activity $25 NPA Member | $50 NonMember NPA Staff Joni Cover, JD Marcia Mueting, PharmD Diane Webb Sarah Hunter Chief Executive Officer VP, Professional Affairs Finance & Marketing Project Coordinator Pharmacy Technician Second class postage paid at Lincoln, Board of Directors Publisher Nebraska, and at additional mailing offices. Tyler Garrelts The Nebraska Mortar & Pestle (M&P) (ISSN President, Pam Miller Postmaster: send address changes to 0028-1891) is owned and published by Immediate Past President, Nebraska Mortar & Pestle, 6221 S 58th St, the Nebraska Pharmacists Association to Suite A, Lincoln, NE 68516-3687 or email Ally Dering-Anderson Students provide continuing pharmacy education, [email protected]. -

FDA Listing of Established Pharmacologic Class Text Phrases January 2021
FDA Listing of Established Pharmacologic Class Text Phrases January 2021 FDA EPC Text Phrase PLR regulations require that the following statement is included in the Highlights Indications and Usage heading if a drug is a member of an EPC [see 21 CFR 201.57(a)(6)]: “(Drug) is a (FDA EPC Text Phrase) indicated for Active Moiety Name [indication(s)].” For each listed active moiety, the associated FDA EPC text phrase is included in this document. For more information about how FDA determines the EPC Text Phrase, see the 2009 "Determining EPC for Use in the Highlights" guidance and 2013 "Determining EPC for Use in the Highlights" MAPP 7400.13. -

Important Note:All Human Products Must Be Of
* Important Note:All human products must be of human recombinant origin wherever these are available in the market *For oral solution it is preferable:Syrup then Suspension and then Elixir MOH CODE ITEM NAME Qty 1 CARDIOVASCULAR SYSTEM 1A Positive inotropic drugs 1Aa Digtalis glycoside 02-01-00001 digoxin tab 62.5 mcg 800,000 02-01-00002 digitoxin tab 100 mcg 800,000 02-01-00003 digoxin tab 125 mcg 800,000 02-01-00004 digoxin tab 250 mcg 30,415,200 02-01-00005 digoxin PG elixir 50mcg /ml 800,000 02-01-00006 digoxin inj 250 mcg/ml, (2ml amp) 800,000 1Ab PHOSPHODIESTERASE INHIBITORS 02-01-00007 Enoximone inj 5mg/ml (20ml amp) 800,000 1B DIURETICS 02-01-00008 amiloride Hcl 5mg + hydrochlorthiazide 50mg tab 50,000,000 02-01-00009 bumetanide tab 1 mg 1,094,000 02-01-00010 chlorthalidone tab 50mg 3,264,000 02-01-00011 ethacrynic acid as sod.salt inj powder for 800,000 reconstitution 50mg vial 02-01-00012 frusemide inj 20mg/2ml amp 5,780,400 02-01-00013 frusemide I.V. infusion inj 10mg/ml, (25ml amp) 800,000 02-01-00014 frusemide tab 40mg 25,000,000 02-01-00015 frusemide scored tab 500mg 800,000 02-01-00016 frusemide oral solution pead liquid 1mg/1ml 800,000 02-01-00017 frusemide oral solution 4mg/ml 800,000 02-01-00018 frusemide oral solution 8mg/ml 800,000 02-01-00019 hydrochlorothiazide tab 25mg 1,084,000 02-01-00020 hydrochlorothiazide tab 50mg 1,396,000 02-01-00021 indapamide tab 2.5mg 800,000 02-01-00022 Indapamide s/r coated tab 1.5mg 800,000 02-01-00023 spironolactone tab 25mg 5,568,400 02-01-00024 spironolactone tab 100mg 5,147,200 -
2018 Formulary Drug List
2018 Formulary Drug List For Small Groups and Large Groups GlobalHealth, Inc. 701 NE 10th Street, Suite 300 Oklahoma City, OK 73104-5403 MGDF18 Lists Updated 11/2017 www.GlobalHealth.com/commercial HELPFUL NUMBERS Plan Issuer: Medication Prior Authorizations: GlobalHealth, Inc. [email protected] PO Box 2393 918.878.7361 Oklahoma City, OK 73101-2393 Mail Claims to: GlobalHealth Customer Care, Language Magellan Rx Management, LLC Assistance, and Disease Management: PO Box 85042 [email protected] Richmond, VA 23261-5042 405.280.2964 (local) 1.877.280.2964 (toll-free) Mail Order Pharmacy: 711 (TTY) Magellan Rx Management, LLC Monday – Friday, 9 a.m. – 5 p.m. Central 1.800.424.1789 (toll-free) www.GlobalHealth.com/commercial 711 (TTY) P.O. Box 620968 Behavioral Health and Substance Use: Orlando, FL 32862 [email protected] 405.280.2964 (local) 24/7 Nurse Help Line: 1.877.280.2964 (toll-free) Information Line 711 (TTY) 1.877.280.2993 (toll-free) Monday – Friday, 9 a.m. – 5 p.m. Central www.GlobalHealth.com/commercial GlobalHealth Compliance Officer: 1.877.280.5852 (toll-free) Pharmacy Benefits Manager: 405.280.5852 Magellan Rx Management, LLC [email protected] Customer Service 1.800.424.1789 (toll-free) GlobalHealth Privacy Officer: 711 (TTY) 405.280.5524 [email protected] i IMPORTANT INFORMATION This formulary applies to Members who enrolled through an employer in any of the following Plans: Platinum Plan 1 without Dental Gold Plan 1 with Dental Gold Plan 1 without Dental Standard Plan Member Materials Your comprehensive Member handbook has three booklets. -

Ibm Micromedex® Carenotes Titles by Category
IBM MICROMEDEX® CARENOTES TITLES BY CATEGORY DECEMBER 2019 © Copyright IBM Corporation 2019 All company and product names mentioned are used for identification purposes only and may be trademarks of their respective owners. Table of Contents IBM Micromedex® CareNotes Titles by Category Allergy and Immunology ..................................................................................................................2 Ambulatory.......................................................................................................................................3 Bioterrorism ...................................................................................................................................18 Cardiology......................................................................................................................................18 Critical Care ...................................................................................................................................20 Dental Health .................................................................................................................................22 Dermatology ..................................................................................................................................23 Dietetics .........................................................................................................................................24 Endocrinology & Metabolic Disease ..............................................................................................26 -

Clinuvel Price Target: AUD 31.70 Reuters: CUV.AX Bloomberg: CUV:AU the Light Protection Enabler
30 January 2018 Rating: Buy Risk: High Price: AUD 8.65 Clinuvel Price target: AUD 31.70 Reuters: CUV.AX Bloomberg: CUV:AU The light protection enabler We’re initiating coverage of Australian Clinuvel with a WKN/ISIN: A0JEGY/AU000000CUV3 buy rating and a price target of AUD 31.70 per share, Indices: All Ordinaries Index (XAO) since we believe investors are not fully factoring in Transparency level: n/a potential opportunities to Clinuvel’s long-term growth in Weighted average number of share: 47.7 mn the global skin protection market. The orphan disease Market cap: AUD 412.9 mn drug company is dramatically expanding top-line growth Daily trading volume: ~40,000 shares in the near-term as we expect the company to expand its Next AGM: n/a global footprint in EPP. Apart from these significant growth opportunities, that even a rare disease like EPP AUD mn (31/12) 2016 2017 2018e 2019e offers, we expect even more in the years to come, since Revenues 6.4 17.0 46.3 133.4 (1) Clinuvel is expected to launch its vitiligo product in EBITDA -3.1 7.2 22.7 72.0 2021e, representing a substantial larger market than the EBIT -3.2 7.1 22.5 71.6 rare disease EPP, (2) the launch of a topical product EBT -3.2 7.1 22.8 72.0 should make room for the mass market of non- EAT -3.2 7.1 22.8 72.0 prescription skin care solutions, and (3) Clinuvel could also offer a treatment for various Central Nervous % of revenues. -

Pharmaceutical Cream Compositions Comprising Oxymetazoline to Treat Rosacea
(19) TZZ¥___ __T (11) EP 3 181 121 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 21.06.2017 Bulletin 2017/25 A61K 9/10 (2006.01) A61K 31/4174 (2006.01) A61K 47/10 (2017.01) A61K 47/14 (2017.01) (2006.01) (21) Application number: 16196317.8 A61K 9/00 (22) Date of filing: 01.12.2011 (84) Designated Contracting States: • POWALA, Christopher AL AT BE BG CH CY CZ DE DK EE ES FI FR GB Radnor GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO Pennsylvania 19087 (US) PL PT RO RS SE SI SK SM TR • RIOS, Luis Pembroke Pines (30) Priority: 03.12.2010 US 419693 P Florida 33029 (US) 03.12.2010 US 419697 P (74) Representative: Hoffmann Eitle (62) Document number(s) of the earlier application(s) in Patent- und Rechtsanwälte PartmbB accordance with Art. 76 EPC: Arabellastraße 30 11794911.5 / 2 645 993 81925 München (DE) (71) Applicant: ALLERGAN, INC. Remarks: Irvine, CA 92612 (US) •This application was filed on 28-10-2016 as a divisional application to the application mentioned (72) Inventors: under INID code 62. • SHANLER, Stuart D. •Claims filed after the date of receipt of the divisional Pomona application (Rule 68(4) EPC). New York 10970 (US) (54) PHARMACEUTICAL CREAM COMPOSITIONS COMPRISING OXYMETAZOLINE TO TREAT ROSACEA (57) Embodiments relating to cream formulations as baceous glands, such as acne, perioral dermatitis, and well as oxymetazoline creams and methods for treating pseudofolliculitis barbae; disorders of sweat glands, such rosacea and symptoms associated with rosacea, includ- as miliaria, including, but not limited -
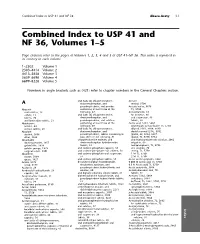
Combined Index to USP 41 and NF 36, Volumes 1–5
Combined Index to USP 41 and NF 36 Abaca-Acety I-1 Combined Index to USP 41 and NF 36, Volumes 1–5 Page citations refer to the pages of Volumes 1, 2, 3, 4 and 5 of USP 41±NF 36. This index is repeated in its entirety in each volume. 1–2302 Volume 1 2303–4414 Volume 2 4415–5658 Volume 3 5659–6698 Volume 4 6699–8228 Volume 5 Numbers in angle brackets such as 〈421〉 refer to chapter numbers in the General Chapters section. and (salts of) chlorpheniramine, Acetate A dextromethorphan, and methyl, 5706 pseudoephedrine, oral powder Acetate buffer, 5676 Abacavir containing at least three of the TS, 5750 oral solution, 19 following, 47 Acetazolamide, 65 sulfate, 23 and (salts of) chlorpheniramine, for injection, 66 tablets, 20 dextromethorphan, and oral suspension, 68 and lamivudine tablets, 21 pseudoephedrine, oral solution tablets, 68 Abiraterone containing at least three of the Acetic acid, 5181, 5664 acetate, 24 following, 49 ammonium acetate buffer TS, 5750 acetate tablets, 26 and (salts of) chlorpheniramine, diluted, 5181, 5664, 5690 Absolute dextromethorphan, and double-normal (2 N), 5762 alcohol, 5666 pseudoephedrine, tablets containing at glacial, 69, 5664, 5697 ether, 5664 least three of the following, 51 glacial, TS, 5750, 5754 Absorbable chlorpheniramine maleate, and and hydrocortisone otic solution, 2062 dusting powder, 1457 dextromethorphan hydrobromide irrigation, 69 gelatin film, 1929 tablets, 53 metaphosphoric, TS, 5756 gelatin sponge, 1929 and codeine phosphate capsules, 55 otic solution, 70 surgical suture, 3901 and codeine phosphate