Positional Asphyxia Pdf 98.64 KB
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hypothermia Brochure
Visit these websites for more water safety and hypothermia prevention in- formation. What is East Pierce Fire & Rescue Hypothermia? www.eastpiercefire.org Hypothermia means “low temperature”. Washington State Drowning When your body is exposed to cold tem- Prevention Coalition Hypothermia www.drowning-prevention.org perature, it tries to protect itself by keeping a normal body temperature of 98.6°F. It Children’s Hospital & tries to reduce heat loss by shivering and Regional Medical Center In Our Lakes moving blood from your arms and legs to www.seattlechildrens.org the core of your body—head, chest and and Rivers abdomen. Hypothermia Prevention, Recognition and Treatment www.hypothermia.org Stages of Hypothermia Boat Washington Mild Hypothermia www.boatwashington.org (Core body temperature of 98.6°— 93.2°F) Symptoms: Shivering; altered judg- ment; numbness; clumsiness; loss of Boat U.S. Foundation dexterity; pain from cold; and fast www.boatus.com breathing. Boat Safe Moderate Hypothermia www.boatsafe.com (Core body temperature of 93.2°—86°F) Symptoms: Semiconscious to uncon- scious; shivering reduced or absent; lips are blue; slurred speech; rigid n in muscles; appears drunk; slow Eve breathing; and feeling of warmth can occur. mer! Headquarters Station Sum Severe Hypothermia 18421 Old Buckley Hwy (Core body temperature below 86°F) Bonney Lake, WA 98391 Symptoms: Coma; heart stops; and clinical death. Phone: 253-863-1800 Fax: 253-863-1848 Email: [email protected] Know the water. Know your limits. Wear a life vest. By choosing to swim in colder water you Waters in Western Common Misconceptions Washington reduce your survival time. -

No Limits Freediving
1 No Limits Freediving "The challenges to the respiratory function of the breath-hold diver' are formidable. One has to marvel at the ability of the human body to cope with stresses that far exceed what normal terrestrial life requires." Claes Lundgren, Director, Center for Research and Education in Special Environments A woman in a deeply relaxed state floats in the water next to a diving buoy. She is clad in a figure-hugging wetsuit, a dive computer strapped to her right wrist, and another to her calf. She wears strange form-hugging silicone goggles that distort her eyes, giving her a strange bug-eyed appearance. A couple of meters away, five support divers tread water near a diving platform, watching her perform an elaborate breathing ritual while she hangs onto a metal tube fitted with two crossbars. A few meters below the buoy, we see that the metal tube is in fact a weighted sled attached to a cable descending into the dark-blue water. Her eyes are still closed as she begins performing a series of final inhalations, breathing faster and faster. Photographers on the media boats snap pictures as she performs her final few deep and long hyperventilations, eliminating carbon dioxide from her body. Then, a thumbs-up to her surface crew, a pinch of the nose clip, one final lungful of air, and the woman closes her eyes, wraps her knees around the bottom bar of the sled, releases a brake device, and disappears gracefully beneath the waves. The harsh sounds of the wind and waves suddenly cease and are replaced by the effervescent bubbling of air being released from the regulators of scuba-divers. -

The Hazards of Nitrogen Asphyxiation US Chemical Safety and Hazard Investigation Board
The Hazards of Nitrogen Asphyxiation US Chemical Safety and Hazard Investigation Board Introduction • Nitrogen makes up 78% of the air we breath; because of this it is often assumed that nitrogen is not hazardous. • However, nitrogen is safe to breath only if it is mixed with an appropriate amount of oxygen. • Additional nitrogen (lower oxygen) cannot be detected by the sense of smell. Introduction • Nitrogen is used commercially as an inerting agent to keep material free of contaminants (including oxygen) that may corrode equipment, present a fire hazard, or be toxic. • A lower oxygen concentration (e.g., caused by an increased amount of nitrogen) can have a range of effects on the human body and can be fatal if if falls below 10% Effects of Oxygen Deficiency on the Human Body Atmospheric Oxygen Concentration (%) Possible Results 20.9 Normal 19.0 Some unnoticeable adverse physiological effects 16.0 Increased pulse and breathing rate, impaired thinking and attention, reduced coordination 14.0 Abnormal fatigue upon exertion, emotional upset, faulty coordination, poor judgment 12.5 Very poor judgment and coordination, impaired respiration that may cause permanent heart damage, nausea, and vomiting <10 Inability to move, loss of consciousness, convulsions, death Source: Compressed Gas Association, 2001 Statistics on Incidents CSB reviewed cases of nitrogen asphyxiation that occurred in the US between 1992 and 2002 and determined the following: • 85 incidents of nitrogen asphyxiation resulted in 80 deaths and 50 injuries. • The majority of -

Clinical Management of Severe Acute Respiratory Infections When Novel Coronavirus Is Suspected: What to Do and What Not to Do
INTERIM GUIDANCE DOCUMENT Clinical management of severe acute respiratory infections when novel coronavirus is suspected: What to do and what not to do Introduction 2 Section 1. Early recognition and management 3 Section 2. Management of severe respiratory distress, hypoxemia and ARDS 6 Section 3. Management of septic shock 8 Section 4. Prevention of complications 9 References 10 Acknowledgements 12 Introduction The emergence of novel coronavirus in 2012 (see http://www.who.int/csr/disease/coronavirus_infections/en/index. html for the latest updates) has presented challenges for clinical management. Pneumonia has been the most common clinical presentation; five patients developed Acute Respira- tory Distress Syndrome (ARDS). Renal failure, pericarditis and disseminated intravascular coagulation (DIC) have also occurred. Our knowledge of the clinical features of coronavirus infection is limited and no virus-specific preven- tion or treatment (e.g. vaccine or antiviral drugs) is available. Thus, this interim guidance document aims to help clinicians with supportive management of patients who have acute respiratory failure and septic shock as a consequence of severe infection. Because other complications have been seen (renal failure, pericarditis, DIC, as above) clinicians should monitor for the development of these and other complications of severe infection and treat them according to local management guidelines. As all confirmed cases reported to date have occurred in adults, this document focuses on the care of adolescents and adults. Paediatric considerations will be added later. This document will be updated as more information becomes available and after the revised Surviving Sepsis Campaign Guidelines are published later this year (1). This document is for clinicians taking care of critically ill patients with severe acute respiratory infec- tion (SARI). -

How to Help Someone Having a Panic Attack
How to Help Someone Having a Panic Attack 1. Understand what a panic attack is. A panic attack is a sudden attack of extreme anxiety. It can occur without warning and for no obvious reason. The symptoms are listed under the tips sections of this article. In extreme cases, the symptoms may be accompanied by an acute fear of dying. Although they are quite distressing, panic attacks are not usually life-threatening and can last from 5 - 20 minutes. It is important to note that the signs and symptoms of a panic attack can be similar to those of a heart attack. 2. If this is the first time the person has had something like this, seek emergency medical attention. When in doubt, it is always best to seek immediate medical attention. If the person has diabetes, asthma or other medical problems, seek medical help. 3. Find out the cause of the attack. Talk to the person and determine if he or she is having a panic attack and not another kind of medical emergency (such as a heart or asthma attack) which would require immediate medical attention. Check that the cause of poor breathing is not asthma, as asthma is an entirely different condition and requires different treatments. WARNINGS • Panic attacks, especially to someone who has never had one before, often seem like heart attacks. But heart attacks can be deadly, and if there's any question as to which one it is, it's best to call emergency services. • It should be noted that many asthma sufferers have panic attacks. -
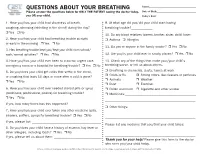
QUESTIONS ABOUT YOUR BREATHING Name:______Please Answer the Questions Below for ONLY the PATIENT Seeing the Doctor Today, Date of Birth:______You OR Your Child
QUESTIONS ABOUT YOUR BREATHING Name:_____________________________________ Please answer the questions below for ONLY THE PATIENT seeing the doctor today, Date of Birth:_______________________________ you OR your child. Today’s Date:_______________________________ 1. Have you/has your child had shortness of breath, 9. At what age did you/did your child start having coughing, wheezing (whistling in the chest) during the day? breathing trouble?_____________ r Yes r No 10. Do any blood relatives (parent, brother, sister, child) have: 2. Have you/has your child had breathing trouble at night r Asthma r Allergies or early in the morning r Yes r No 11. Do you or anyone in the family smoke? r Yes r No 3. Has breathing trouble kept you/kept your child from school/ work/normal activities? r Yes r No 12. Are you/is your child ever in smoky places? r Yes r No 4. Have you/has your child ever been to a doctor, urgent care, 13. Check any of the things that make your/your child’s emergency room or a hospital for breathing trouble? r Yes r No breathing worse, or tell us about others. 5. Do you/does your child get colds that settle in the chest, r Breathing in chemicals, dusts, fumes at work r Colds or flu r Strong odors, like cleaners or perfumes or coughing that lasts 10 days or more after a cold is gone? r Animals r Weather r Yes r No r Dust r Exercise 6. Have you/has your child ever needed steroid pills or syrup r Pollen and mold r Cigarette and other smoke (prednisone, prednisolone, prelone) for breathing trouble? r Medicines:___________________________________________ r Yes r No _______________________________________________________ If yes, how many times has this happened? ___________________ r Other things: 7. -

Diver Medical | Participant Questionnaire Directions
Diver Medical | Participant Questionnaire Recreational scuba diving and freediving requires good physical and mental health. There are a few medical conditions which can be hazardous while diving, listed below. Those who have, or are predisposed to, any of these conditions, should be evaluated by a physician. This Diver Medical Participant Questionnaire provides a basis to determine if you should seek out that evaluation. If you have any concerns about your diving fitness not represented on this form, consult with your physician before diving. If you are feeling ill, avoid diving. If you think you may have a contagious disease, protect yourself and others by not participating in dive training and/or dive activities. References to “diving” on this form encompass both recreational scuba diving and freediving. This form is principally designed as an initial medical screen for new divers, but is also appropriate for divers taking continuing education. For your safety, and that of others who may dive with you, answer all questions honestly. Directions Complete this questionnaire as a prerequisite to a recreational scuba diving or freediving course. Note to women: If you are pregnant, or attempting to become pregnant, do not dive. Yes I have had problems with my lungs/breathing, heart, blood, or have been diagnosed with COVID-19. No 1 Go to Box A Yes I am over 45 years of age. No 2 Go to Box B I struggle to perform moderate exercise (for example, walk 1.6 kilometer/one mile in 14 minutes 3 or swim 200 meters/yards without resting), OR I have been unable to participate in a normal Yes No physical activity due to fitness or health reasons within the past 12 months. -

Carbon Dioxide Exposure Effects – Fact Sheet
CARBON DIOXIDE EXPOSURE EFFECTS – FACT SHEET Studies by NIOSH in 1976 dispelled the myth that carbon dioxide is an asphyxiant gas and only causes adverse health effects when it displaces oxygen. Symptoms of overexposure by inhalation include dizziness, headache, nausea, rapid breathing, shortness of breath, deeper breathing, increased heart rate (tachycardia), eye and extremity twitching, cardiac arrhythmia, memory disturbances, lack of concentration, visual and hearing disturbances (including photophobia, blurred vision, transient blindness, hearing loss and ringing in the ears), sweating, restlessness, vomiting, shaking, confusion, flushed skin, panic, parathesis (a sensation of numbness in the extremities), disorientation, convulsions, unconsciousness, coma, and death. CO2 Duration Physiological Impact/Health Effect Concentration 1,000 ppm Less than Impairs judgment, decision-making ability, and thinking skills on a 2½ hrs. short-term basis, even for healthy individuals. 2,500 ppm Less than Many individuals are rendered cognitively marginal or 2½ hrs. dysfunctional. 5,000 ppm with Headache, lethargy, mental slowness, emotional irritation, and 20.9% Oxygen sleep disruption. 6% 1-2 mins. Hearing and visual disturbances 7% (70,000 ppm) 5 mins. death with 20.9% Oxygen 10% to 15% Dizziness, drowsiness, severe muscle twitching, unconsciousness and death within a few minutes. Within 1 Loss of controlled and purposeful activity, unconsciousness, coma, 17% to 30% min. convulsions, and death 30% carbon 30 secs. Unconsciousness, with some subjects having seizures that were dioxide, with 70% characterized as decerebrate (no cerebral functioning). oxygen Even though oxygen is necessary to carry out cell functions, it is not the lack of oxygen that stimulates breathing. Breathing is stimulated by an excess of CO2. -

Beneath Tropic Seas; a Record of Diving Among the Coral Reefs of Haiti
^'%^^ C Ij > iUiJs'fr) R/V ChTiiit-UBRARY BOOKS BY WILLIAM BEEBE TWO BIRD-LOVERS IN MEXICO Houghton, Mifflin Co.—ig05 THE BIRD Henry Holt and Co.—igo6 THE LOG OP THE SUN Henry Holt and Co.—igo6 OUR SEARCH FOR A WILDERNESS Henry Holt and Co.—ig/o TROPICAL WILD LIFE New York Zoological Society—igr^ JUNGLE PEACE Henry Holt and Co. —igiS EDGE OF THE JUNGLE Henry Holt and Co.—ig2l A MONOGRAPH OF THE PHEASANTS H. F. Witherby and Co.—igi8-ig22 GALAPAGOS: WORLD'S END G. P. Putnam's Sons—ig24 JUNGLE DAYS G. P. Putnam's Sons—ig2S THE ARCTURUS ADVENTURE G. P. Putnam's Sons—ig26 pheasants: their lives and homes Doubleday, Page ^ Co. —1926 pheasant JUNGLES G. P. Putnam's Sons—Jg2y BENEATH TROPIC BEAS G. P. Putnam's Sons—1928 ^1 No-Man's-Land Five Fathoms Down Painted by Zarh Pritchard many feet beneath the water on a coral reef in the Lagoon of Maraa, Tahiti ^' BENEATH TROPIC SEAS C" ^ A RECORD OF DIVING AMONG THE CORAL REEFS OF HAITI BY WILLIAM BEEBE, ScD. ^Director of the 'Department of 'tropical 'Research of the V^ew york 'Zoological Society TH SIXTY ILLUSTRATIONS G. P. PUTNAM'S SONS NEW YORK — LONDON 1928 R/V Cjri>*«W BENEATH TROPIC SEAS ex- Copyright, 1928 by William Beebe First printing, September, 1928 Second printing, September, 1928 ^^ Made in the United States of America To ELSWYTH THANE I PREFACE The Tenth Expedition of the Department of Tropical Research of the New York Zoological Society was made possible by generous contribu- tions from members of the Society. -

Salem Area Mass Transit District BOARD of DIRECTORS VIRTUAL MEETING Thursday, February 25, 2021 at 6:30 PM
Salem Area Mass Transit District BOARD OF DIRECTORS VIRTUAL MEETING Thursday, February 25, 2021 at 6:30 PM PURSUANT TO GOVERNOR BROWN’S EXECUTIVE ORDER TO KEEP THE COMMUNITY SAFE DURING THE CONTINUING COVID-19 PANDEMIC EVENT, THIS MEETING WILL BE ONLINE ONLY. GO TO: Join ZoomGov Meeting https://cherriots-org.zoomgov.com/j/1608361530?pwd=MHNSRGZ3a1FiTE5XSHlGdzYvRWpuUT09 Zoom ID: 160 836 1530 | Passcode: 864458 Comcast Cable . Channel 21 Cherriots Facebook Live. https://www.facebook.com/cherriots/ YouTube through CC:Media. https://www.capitalcommunitymedia.org/all AGENDA A. CALL TO ORDER (President Ian Davidson) 1. Note of Attendance for a Quorum 2. Pledge of Allegiance 3. “Safety Moment” B. ANNOUNCEMENTS & CHANGES TO AGENDA This is the time for Board members to declare a (potential) conflict of interest prior to taking action on the agenda items below. C. PRESENTATION D. PUBLIC COMMENT E. CONSENT CALENDAR Items on the Consent Calendar are considered routine business and are adopted as a group by a single motion unless a Board member requests to withdraw an item. Action on items pulled for discussion will be deferred until after adoption of the Consent Calendar. 1. Approval of Minutes a. January 28, 2021 Board of Directors Meeting ……………………………………………….. 3 b. January 28, 2021 Work Session …………………………………………………………………….. 11 c. January 28, 2021 Executive Session (Potential Litigation) …………………………………. 13 F. ITEMS DEFERRED FROM THE CONSENT CALENDAR Salem Area Mass Transit District Board of Directors Meeting Agenda February 25, 2021 Page 2 G. ACTION ITEMS 1. Resolution No. 2021-01 Amend Retirement Plan for Non-Represented Employees 15 2. Resolution No. 2021-02 Approval of New Retirement Plan …………………………………. -
Breathing Air Quality, Sampling and Testing
Breathing Air Quality, Sampling and Testing Environmental Health Laboratory Department of Environmental and Occupational Health Sciences School of Public Health University of Washington Funding and support from The State of Washington Department of Labor & Industries Safety & Health Investment Projects Medical Aid and Accident Fund Breathing Air Quality, Sampling, and Testing Environmental Health Laboratory Department of Environmental and Occupational Health Sciences School of Public Health University of Washington Funding and support from The State of Washington Department of Labor & Industries Safety & Health Investment Projects Medical Aid and Accident Funds 1 University of Washington Environmental Health Laboratory Table of Contents Overview ...............................................................................1 Background ...........................................................................2 Regulated Components of Breathing Air ...............................7 Performance of Breathing Air Testing Kits ............................9 Laboratory Accreditation .....................................................18 Guidance Summary .............................................................19 Glossary ..............................................................................20 References ...........................................................................22 List of Tables Table 1. Breathing Air Quality Specifications ........................2 Table 2. Description of Kits Tested ........................................9 -

Safety Induction and Guidelines for Snorkel, Freedive and Finswimming
Geelong Freedivers Inc. Safety Induction and guidelines for Snorkel, Freedive and Finswimming Training Pool Requirements Booking training sessions ● Ensure your AUF insurance and GFD membership is up to date. ● Try and book at least 1 day prior as this allows time to get additional lanes booked if required. Signing attendance log ● Upon entering please sign the attendance book. ● If you’re the first person to arrive ask for the Geelong Freedivers attendance sheet. ● We need to do this for billing and safety. Start/End Times: ● We officially have access to the lane(s) at 18:45 ● Unofficially we can use the diving pool from 18:00 onwards. ● The session ends ~ 19:45 allowing time to get changed. General approach: ● Warmup up 18:00-18:45. ● Main session 18:45-19:45 Theory Quick Note ● The majority of this safety induction is going to concentrate on potential issues that could arise and prevention of possible incidents. ● We don’t want this to detract from the positive benefits to pool training of which there are many. ● There is a significant amount of information regarding physics, physiology, and general theory that it outside of the safety induction scope. It’s strongly recommended that you undertake a more indepth course for detailed instruction on these areas. ● In this session the goal is to provide basic coverage and to ensure each participant is introduced to the the GFD safety protocols and able to train safely. ● Feel free to ask questions during the safety induction and whenever you’re training from this point forwards. The Buddy System ● Never Dive Alone.