Prednisolone Also Binds to Transcortin • Other Synthetic GS Only Bind to Albumin
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Penetration of Synthetic Corticosteroids Into Human Aqueous Humour
Eye (1990) 4, 526--530 Penetration of Synthetic Corticosteroids into Human Aqueous Humour C. N. 1. McGHEE,1.3 D. G. WATSON, 3 1. M. MIDGLEY, 3 M. 1. NOBLE, 2 G. N. DUTTON, z A. I. FERNl Glasgow Summary The penetration of prednisolone acetate (1%) and fluorometholone alcohol (0.1%) into human aqueous humour following topical application was determined using the very sensitive and specific technique of Gas Chromatography with Mass Spec trometry (GCMS). Prednisolone acetate afforded peak mean concentrations of 669.9 ng/ml within two hours and levels of 28.6 ng/ml in aqueous humour were detected almost 24 hours post application. The peak aqueous humour level of flu orometholone was S.lng/ml. The results are compared and contrasted with the absorption of dexamethasone alcohol (0.1%), betamethasone sodium phosphate (0.1 %) and prednisolone sodium phosphate (0.5%) into human aqueous humour. Topical corticosteroid preparations have been prednisolone acetate (1.0%) and fluorometh used widely in ophthalmology since the early alone alcohol (0.1 %) (preliminary results) 1960s and over the last 10 years the choice of into the aqueous humour of patients under preparations has become larger and more going elective cataract surgery. varied. Unfortunately, data on the intraocular penetration of these steroids in humans has SUbjects and Methods not paralleled the expansion in the number of Patients who were scheduled to undergo rou available preparations; indeed until recently, tine cataract surgery were recruited to the estimation of intraocular penetration has study and informed consent was obtained in been reliant upon extrapolation of data from all cases (n=88), Patients with corneal disease animal models (see Watson et ai., 1988, for or inflammatory ocular conditions which bibliography). -
[email protected]
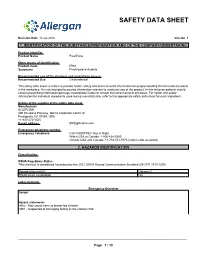
SAFETY DATA SHEET Revision Date 13-Jul-2016 Version 1 1. IDENTIFICATION OF THE SUBSTANCE/PREPARATION AND OF THE COMPANY/UNDERTAKING Product identifier Product Name Pred Forte Other means of identification Product Code FP61 Synonyms Prednisolone Acetate Recommended use of the chemical and restrictions on use Recommended Use Corticosteroid This safety data sheet is written to provide health, safety and environmental information for people handling this formulated product in the workplace. It is not intended to provide information relevant to medicinal use of the product. In this instance patients should consult prescribing information/package insert/product label or consult their pharmacist or physician. For health and safety information for individual ingredients used during manufacturing, refer to the appropriate safety data sheet for each ingredient. Details of the supplier of the safety data sheet Manufacturer ALLERGAN 400 Interpace Parkway, Morris Corporate Center III Parsippany, NJ 07054, USA +1-800-272-5525 E-mail address [email protected] Emergency telephone number Emergency Telephone Call CHEMTREC Day or Night Within USA or Canada: 1-800-424-9300 Outside USA and Canada: +1-703-741-5970 (collect calls accepted) 2. HAZARDS IDENTIFICATION Classification OSHA Regulatory Status This chemical is considered hazardous by the 2012 OSHA Hazard Communication Standard (29 CFR 1910.1200) Reproductive toxicity Category 2 Effects on or via lactation Yes Label elements Emergency Overview Danger Hazard statements H362 - May cause harm to breast-fed -

NINDS Custom Collection II
ACACETIN ACEBUTOLOL HYDROCHLORIDE ACECLIDINE HYDROCHLORIDE ACEMETACIN ACETAMINOPHEN ACETAMINOSALOL ACETANILIDE ACETARSOL ACETAZOLAMIDE ACETOHYDROXAMIC ACID ACETRIAZOIC ACID ACETYL TYROSINE ETHYL ESTER ACETYLCARNITINE ACETYLCHOLINE ACETYLCYSTEINE ACETYLGLUCOSAMINE ACETYLGLUTAMIC ACID ACETYL-L-LEUCINE ACETYLPHENYLALANINE ACETYLSEROTONIN ACETYLTRYPTOPHAN ACEXAMIC ACID ACIVICIN ACLACINOMYCIN A1 ACONITINE ACRIFLAVINIUM HYDROCHLORIDE ACRISORCIN ACTINONIN ACYCLOVIR ADENOSINE PHOSPHATE ADENOSINE ADRENALINE BITARTRATE AESCULIN AJMALINE AKLAVINE HYDROCHLORIDE ALANYL-dl-LEUCINE ALANYL-dl-PHENYLALANINE ALAPROCLATE ALBENDAZOLE ALBUTEROL ALEXIDINE HYDROCHLORIDE ALLANTOIN ALLOPURINOL ALMOTRIPTAN ALOIN ALPRENOLOL ALTRETAMINE ALVERINE CITRATE AMANTADINE HYDROCHLORIDE AMBROXOL HYDROCHLORIDE AMCINONIDE AMIKACIN SULFATE AMILORIDE HYDROCHLORIDE 3-AMINOBENZAMIDE gamma-AMINOBUTYRIC ACID AMINOCAPROIC ACID N- (2-AMINOETHYL)-4-CHLOROBENZAMIDE (RO-16-6491) AMINOGLUTETHIMIDE AMINOHIPPURIC ACID AMINOHYDROXYBUTYRIC ACID AMINOLEVULINIC ACID HYDROCHLORIDE AMINOPHENAZONE 3-AMINOPROPANESULPHONIC ACID AMINOPYRIDINE 9-AMINO-1,2,3,4-TETRAHYDROACRIDINE HYDROCHLORIDE AMINOTHIAZOLE AMIODARONE HYDROCHLORIDE AMIPRILOSE AMITRIPTYLINE HYDROCHLORIDE AMLODIPINE BESYLATE AMODIAQUINE DIHYDROCHLORIDE AMOXEPINE AMOXICILLIN AMPICILLIN SODIUM AMPROLIUM AMRINONE AMYGDALIN ANABASAMINE HYDROCHLORIDE ANABASINE HYDROCHLORIDE ANCITABINE HYDROCHLORIDE ANDROSTERONE SODIUM SULFATE ANIRACETAM ANISINDIONE ANISODAMINE ANISOMYCIN ANTAZOLINE PHOSPHATE ANTHRALIN ANTIMYCIN A (A1 shown) ANTIPYRINE APHYLLIC -

Drug Name Plate Number Well Location % Inhibition, Screen Axitinib 1 1 20 Gefitinib (ZD1839) 1 2 70 Sorafenib Tosylate 1 3 21 Cr
Drug Name Plate Number Well Location % Inhibition, Screen Axitinib 1 1 20 Gefitinib (ZD1839) 1 2 70 Sorafenib Tosylate 1 3 21 Crizotinib (PF-02341066) 1 4 55 Docetaxel 1 5 98 Anastrozole 1 6 25 Cladribine 1 7 23 Methotrexate 1 8 -187 Letrozole 1 9 65 Entecavir Hydrate 1 10 48 Roxadustat (FG-4592) 1 11 19 Imatinib Mesylate (STI571) 1 12 0 Sunitinib Malate 1 13 34 Vismodegib (GDC-0449) 1 14 64 Paclitaxel 1 15 89 Aprepitant 1 16 94 Decitabine 1 17 -79 Bendamustine HCl 1 18 19 Temozolomide 1 19 -111 Nepafenac 1 20 24 Nintedanib (BIBF 1120) 1 21 -43 Lapatinib (GW-572016) Ditosylate 1 22 88 Temsirolimus (CCI-779, NSC 683864) 1 23 96 Belinostat (PXD101) 1 24 46 Capecitabine 1 25 19 Bicalutamide 1 26 83 Dutasteride 1 27 68 Epirubicin HCl 1 28 -59 Tamoxifen 1 29 30 Rufinamide 1 30 96 Afatinib (BIBW2992) 1 31 -54 Lenalidomide (CC-5013) 1 32 19 Vorinostat (SAHA, MK0683) 1 33 38 Rucaparib (AG-014699,PF-01367338) phosphate1 34 14 Lenvatinib (E7080) 1 35 80 Fulvestrant 1 36 76 Melatonin 1 37 15 Etoposide 1 38 -69 Vincristine sulfate 1 39 61 Posaconazole 1 40 97 Bortezomib (PS-341) 1 41 71 Panobinostat (LBH589) 1 42 41 Entinostat (MS-275) 1 43 26 Cabozantinib (XL184, BMS-907351) 1 44 79 Valproic acid sodium salt (Sodium valproate) 1 45 7 Raltitrexed 1 46 39 Bisoprolol fumarate 1 47 -23 Raloxifene HCl 1 48 97 Agomelatine 1 49 35 Prasugrel 1 50 -24 Bosutinib (SKI-606) 1 51 85 Nilotinib (AMN-107) 1 52 99 Enzastaurin (LY317615) 1 53 -12 Everolimus (RAD001) 1 54 94 Regorafenib (BAY 73-4506) 1 55 24 Thalidomide 1 56 40 Tivozanib (AV-951) 1 57 86 Fludarabine -

Pharmacokinetics of Ophthalmic Corticosteroids
British Journal ofOphthalmology 1992; 76: 681-684 681 MINI REVIEW Br J Ophthalmol: first published as 10.1136/bjo.76.11.681 on 1 November 1992. Downloaded from Pharmacokinetics of ophthalmic corticosteroids Corticosteroids have been used by ophthalmologists with an identical vehicle, the aqueous humour concentrations of increasing frequency over the past 30 years, with the these steroids are almost identical.'9 None the less it is concomitant development of a diverse range of drop, essential when considering such empirical data, to recall that ointment, subconjunctival, and oral preparations. Though the systemic anti-inflammatory effect of both betamethasone the clinical benefits and side effects of such corticosteroid and dexamethasone is five to seven times that of predniso- preparations have been well documented, their basic lone.39"' The local anti-inflammatory potency of ocular pharmacokinetics in the human eye have yet to be fully steroids has yet to be fully investigated and whilst early work established. Indeed most of our pharmacokinetic knowledge suggested that prednisolone acetate 1% had the greatest anti- of these drugs has been elucidated by extrapolation of data inflammatory effect in experimental keratitis,'7 later studies obtained from rabbit experiments.1-26 These results can be demonstrated that fluorometholone acetate in a 1% formu- significantly disparate from human data because of the lation was equally efficacious in the same model.26 However, thinner rabbit cornea, lower rabbit blink rate, effect of prednisolone -

Aetna Formulary Exclusions Drug List
Covered and non-covered drugs Drugs not covered – and their covered alternatives 2020 Advanced Control Plan – Aetna Formulary Exclusions Drug List 05.03.525.1B (7/20) Below is a list of medications that will not be covered without a Key prior authorization for medical necessity. If you continue using one of these drugs without prior approval, you may be required UPPERCASE Brand-name medicine to pay the full cost. Ask your doctor to choose one of the generic lowercase italics Generic medicine or brand formulary options listed below. Preferred Options For Excluded Medications1 Excluded drug name(s) Preferred option(s) ABILIFY aripiprazole, clozapine, olanzapine, quetiapine, quetiapine ext-rel, risperidone, ziprasidone, VRAYLAR ABSORICA isotretinoin ACANYA adapalene, benzoyl peroxide, clindamycin gel (except NDC^ 68682046275), clindamycin solution, clindamycin-benzoyl peroxide, erythromycin solution, erythromycin-benzoyl peroxide, tretinoin, EPIDUO, ONEXTON, TAZORAC ACIPHEX, esomeprazole, lansoprazole, omeprazole, pantoprazole, DEXILANT ACIPHEX SPRINKLE ACTICLATE doxycycline hyclate capsule, doxycycline hyclate tablet (except doxycycline hyclate tablet 50 mg [NDC^ 72143021160 only], 75 mg, 150 mg), minocycline, tetracycline ACTOS pioglitazone ACUVAIL bromfenac, diclofenac, ketorolac, PROLENSA acyclovir cream acyclovir (except acyclovir cream), valacyclovir ADCIRCA sildenafil, tadalafil ADZENYS XR-ODT amphetamine-dextroamphetamine mixed salts ext-rel†, dexmethylphenidate ext-rel, dextroamphetamine ext-rel, methylphenidate ext-rel†, MYDAYIS, -

Feline Eosinophilic Keratoconjunctivitis: Nonsteroidal Vs Corticosteroid Topical Treatment
Acta Scientiae Veterinariae, 2021. 49(Suppl 1): 608. CASE REPORT ISSN 1679-9216 Pub. 608 Feline Eosinophilic Keratoconjunctivitis: Nonsteroidal vs Corticosteroid Topical Treatment Gabrielly da Costa Gomes Rodrigues1, Ana Maria Tatoni Pereira Coelho1, João Pedro Brochado Souza2, Joyce Maira de Araújo1, Márcio Virgílio Figueiredo da Silva1, Polyana Mayume Pereira da Silva3 & Gabriel Utida Eguchi1 ABSTRACT Background: Feline eosinophilic keratoconjunctivitis is a proliferative eye lesion of chronic aspect with usually unilateral presentation that may initiate as a superficial vascularization that evolves to a proliferative, granular, irregular lesion of whitish-pink aspect. With its association with an immune-mediated response, nonsteroidal anti-inflammatories do not appear to be efficient, although few studies describe its use. This case report describes a case of a feline eosinophilic kera- toconjunctivitis with its clinical evolution since the use of nonsteroidal topical anti-inflammatory drug in an undiagnosed patient and the transition to a topical corticosteroid and cure after 14 days since diagnosis. Case: An 8-year-old female cat was attended at the Veterinary Hospital of the Dom Bosco Catholic University (UCDB), with main complaint being an eye injury with at least 36 days of evolution and unresponsive to treatment (topical tobra- mycin 0.3% every 12 h / ketorolac trometamol 0.5%/ every 12 h and ophthalmic lubricant/every 4 h). Since the patient had free access to the street, the owners suspected of trauma-induced lesion. At physical examination, it was observed a proliferative lesion at the peri-limbal superotemporal quadrant of the right cornea with approximately 0.4 cm diameter, with color varying of pale to pink, with irregular surface and low vascularity, the adjacent conjunctiva was also affected with similar multiple nodular lesions (0.1 cm). -

Medication Safety Communication – Prednefrin Forte Eye Drops 10Ml
MEDICATION SAFETY COMMUNICATION Information for health professionals in NSW public health organisations Prednefrin Forte eye drops 10mL – 3 March 2021 Prednefrin Forte (prednisolone acetate 1%, phenylephrine 0.12% Details of affected product(s) suspension) 10mL eye drops – ARTG 23235 Reason for communication Supply disruption – manufacturing reasons Shortage commencement date 22 February 2021 Estimated resolution date 1 January 2022 Main therapeutic applications Severe noninfectious eye inflammation such as acute iritis, iridocyclitis, scleritis, episcleritis, uveitis, resistant ocular allergy and post-surgery e.g. post-operative care for cataract and other intraocular surgery. Alternative agents • Equivalent alternatives to the Australian registered prednisolone acetate 1% / phenylephrine 0.12% eye drops (Prednefrin Forte) are unavailable and at this time, there is no provisionally registered product available through Section 19A of the Therapeutic Goods Act. • Existing Prednefrin Forte stock should be reserved for use in patients where alternative agents may be inappropriate e.g. allergy or clinical indication. • In the absence of Prednefrin Forte: • Dexamethasone 0.1% eye drops (Maxidex) are the preferred alternative (as per ACI Ophthalmology Network). Consult with local Ophthalmology teams for situations where other agents may be preferred. • For indications where prednisolone acetate 1% / phenylephrine 0.12% eye drops are essential, sites may wish to consider local aseptic compounding options. • Medsurge Healthcare may be able to supply prednisolone acetate 1% (Pred Forte) eye drops via the Therapeutic Goods Administration’s Special Access Scheme (SAS). The product is registered in New Zealand, with product information and labelling in English. Lead time is 5-7 business days. • LINK Healthcare may also be able to provide prednisolone acetate 1% / phenylephrine hydrochloride 0.12% (Prednefrin Forte) eye drops via the SAS. -

Preferred Drug List
Kansas State Employee ANALGESICS Second Generation cefprozil Health Plan NSAIDs cefuroxime axetil diclofenac sodium delayed-rel Preferred Drug List diflunisal Third Generation etodolac cefdinir 2021 ibuprofen cefixime (SUPRAX) meloxicam nabumetone Erythromycins/Macrolides naproxen sodium tabs azithromycin naproxen tabs clarithromycin oxaprozin clarithromycin ext-rel sulindac erythromycin delayed-rel erythromycin ethylsuccinate NSAIDs, COMBINATIONS erythromycin stearate diclofenac sodium delayed-rel/misoprostol fidaxomicin (DIFICID) Effective 04/01/2021 NSAIDs, TOPICAL Fluoroquinolones diclofenac sodium gel 1% ciprofloxacin For questions or additional information, diclofenac sodium soln levofloxacin access the State of Kansas website at moxifloxacin http://www.kdheks.gov/hcf/sehp or call COX-2 INHIBITORS Penicillins the Kansas State Employees Prescription celecoxib amoxicillin Drug Program at 1-800-294-6324. amoxicillin/clavulanate The Preferred Drug List is subject to change. GOUT amoxicillin/clavulanate ext-rel To locate covered prescriptions online, allopurinol ampicillin access the State of Kansas website at colchicine tabs dicloxacillin http://www.kdheks.gov/hcf/sehp for the probenecid penicillin VK most current drug list. colchicine (MITIGARE) Tetracyclines What is a Preferred Drug List? OPIOID ANALGESICS doxycycline hyclate A Preferred Drug List is a list of safe and buprenorphine transdermal minocycline cost-effective drugs, chosen by a committee codeine/acetaminophen tetracycline of physicians and pharmacists. Drug lists fentanyl -

Preferred Drug List
October 2021 Preferred Drug List The Preferred Drug List, administered by CVS Caremark® on behalf of Siemens, is a guide within select therapeutic categories for clients, plan members and health care providers. Generics should be considered the first line of prescribing. If there is no generic available, there may be more than one brand-name medicine to treat a condition. These preferred brand-name medicines are listed to help identify products that are clinically appropriate and cost-effective. Generics listed in therapeutic categories are for representational purposes only. This is not an all-inclusive list. This list represents brand products in CAPS, branded generics in upper- and lowercase Italics, and generic products in lowercase italics. PLAN MEMBER HEALTH CARE PROVIDER Your benefit plan provides you with a prescription benefit program Your patient is covered under a prescription benefit plan administered administered by CVS Caremark. Ask your doctor to consider by CVS Caremark. As a way to help manage health care costs, prescribing, when medically appropriate, a preferred medicine from authorize generic substitution whenever possible. If you believe a this list. Take this list along when you or a covered family member brand-name product is necessary, consider prescribing a brand name sees a doctor. on this list. Please note: Please note: • Your specific prescription benefit plan design may not cover • Generics should be considered the first line of prescribing. certain products or categories, regardless of their appearance in • This drug list represents a summary of prescription coverage. It is this document. Products recently approved by the U.S. Food and not all-inclusive and does not guarantee coverage. -

Cancer Drugs -Oral Blood Thinners (Anticoagulants) (Antineoplastics)
BLOOD CANCER DRUGS-OTHER (ANTINEOPLASTICS) BLOOD MODIFIERS CANCER DRUGS-OTHER (ANTINEOPLASTICS) anagrelide (P) NEUPOGEN SYLATRON (P) pentoxifylline (M) (P) PROCRIT CANCER DRUGS -ORAL BLOOD THINNERS (ANTICOAGULANTS) (ANTINEOPLASTICS) COUMADIN (M) CANCER DRUGS -ORAL (ANTINEOPLASTICS) enoxaparin (M) anastrozole fondaparinux (P) AFINITOR FRAGMIN (M) bicalutamide PRADAXA (P) (M) BOSULIF warfarin (P) CAPRELSA (M) STROKE PREVENTION exemestane ERIVEDGE (P) (M) GLEEVEC (P) clopidogrel (P) ticlopidine (M) HYCAMTIN INLYTA (P) (M) CANCER DRUGS-OTHER letrozole NEXAVAR (P) (ANTINEOPLASTICS) (P) REVLIMID (P) CANCER DRUGS-OTHER SPRYCEL (ANTINEOPLASTICS) JAKAFI (P) KEY: Preferred Brand-name Drugs (Tier 2) Generic Drugs (Tier 1) P = Prior Authorization Required, Q = Quantity Limit, M = Maintenance Medication CANCER DRUGS -ORAL CENTRAL NERVOUS SYSTEM (ANTINEOPLASTICS) ANTI-PARKINSON DRUGS CANCER DRUGS -ORAL (M) (ANTINEOPLASTICS) pramipexole ropinirole (M) STIVARGA (P) selegiline (M) SUTENT (P) TARCEVA (P) ATTENTION DEFICIT DISORDER (ADD), TASIGNA (P) NARCOLEPSY (P) TEMODAR (M) (P) amphetamine/dextroamphetamine THALOMID (M) (P) dexmethylphenidate TYKERB (M) (P) dextroamphetamine VOTRIENT (M) (P) methamphetamine XALKORI (M) (P) methylphenidate sr XELODA (M) XTANDI (P) methylphenidate ZELBORAF (P) (P) SEIZURE MEDICATIONS (ANTICONVULSANTS) ZOLINZA (P) ZYTIGA carbamazepine extended release (M) carbamazepine (M) CENTRAL NERVOUS SYSTEM clonazepam (M) diazepam (M) ALZHEIMER'S DRUGS divalproex (M) (M) (M) divalproex sodium ARICEPT-23 (M) (M) ethosuximide donepezil -

Uveitis Therapy: the Corticosteroid Options
Drugs https://doi.org/10.1007/s40265-020-01314-y REVIEW ARTICLE Uveitis Therapy: The Corticosteroid Options Lianna M. Valdes1 · Lucia Sobrin1 © Springer Nature Switzerland AG 2020 Abstract Uveitis is characterized by intraocular infammation involving the uveal tract; its etiologies generally fall into two broad categories: autoimmune/infammatory or infectious. Corticosteroids are a powerful and important class of medications ubiquitous in the treatment of uveitis. They may be given systemically or locally, in the form of topical drops, periocular injection, intravitreal suspension, or intravitreal implant. This review describes each of the currently available corticosteroid treatment options for uveitis, including favorable and unfavorable characteristics of each as well as applicable clinical trials. The main advantage of corticosteroids as a whole is their ability to quickly and efectively control infammation early on in the course of uveitis. However, they can have serious side efects, whether localized to the eye (such as cataract and elevated intraocular pressure) or systemic (such as osteonecrosis and adrenal insufciency) and in the majority of cases of uveitis are not an appropriate option for long-term therapy. Key Points Clinical features of uveitis include keratic precipitates, ante- rior chamber cell and fare, anterior and posterior synechiae, Corticosteroids are an important mainstay in the treat- iris nodules, snowballs, snowbanks, vitreous haze and cells, ment of uveitis. choroidal lesions, and choroidal thickening. Uncontrolled uveitis can be complicated by cystoid macular edema, retinal Corticosteroids can be given systemically or locally, in vasculitis, optic nerve head edema, and subretinal fuid. A the form of topical drops, periocular injection, intravit- mainstay of treatment for uveitis and its sequelae is the use real suspension, or intravitreal implant; each option has of corticosteroids.