Vision Therapy and Neuro-Rehabilitation: Optometric Considerations in Third Party Reimbursement
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Management of Microtropia
Br J Ophthalmol: first published as 10.1136/bjo.58.3.281 on 1 March 1974. Downloaded from Brit. J. Ophthal. (I974) 58, 28 I Management of microtropia J. LANG Zirich, Switzerland Microtropia or microstrabismus may be briefly described as a manifest strabismus of less than 50 with harmonious anomalous correspondence. Three forms can be distinguished: primary constant, primary decompensating, and secondary. There are three situations in which the ophthalmologist may be confronted with micro- tropia: (i) Amblyopia without strabismus; (2) Hereditary and familial strabismus; (3) Residual strabismus after surgery. This may be called secondary microtropia, for everyone will admit that in most cases of convergent strabismus perfect parallelism and bifoveal fixation are not achieved even after expert treatment. Microtropia and similar conditions were not mentioned by such well-known early copyright. practitioners as Javal, Worth, Duane, and Bielschowsky. The views of Maddox (i898), that very small angles were extremely rare, and that the natural tendency to fusion was much too strong to allow small angles to exist, appear to be typical. The first to mention small residual angles was Pugh (I936), who wrote: "A patient with monocular squint who has been trained to have equal vision in each eye and full stereoscopic vision with good amplitude of fusion may in 3 months relapse into a slight deviation http://bjo.bmj.com/ in the weaker eye and the vision retrogresses". Similar observations of small residual angles have been made by Swan, Kirschberg, Jampolsky, Gittoes-Davis, Cashell, Lyle, Broadman, and Gortz. There has been much discussion in both the British Orthoptic Journal and the American Orthoptic journal on the cause of this condition and ways of avoiding it. -

The Dominant Eye: Dominant for Parvo- but Not for Magno-Biased Stimuli?
vision Article The Dominant Eye: Dominant for Parvo- But Not for Magno-Biased Stimuli? Brian K. Foutch 1,* and Carl J. Bassi 2 1 Rosenberg School of Optometry, University of the Incarnate Word, San Antonio, TX 78209, USA 2 College of Optometry, University of Missouri-St Louis, St. Louis, MO 63121, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-210-930-8162 Received: 4 September 2019; Accepted: 8 March 2020; Published: 12 March 2020 Abstract: Eye dominance is often defined as a preference for the visual input of one eye to the other. Implicit in this definition is the dominant eye has better visual function. Several studies have investigated the effect of visual direction or defocus on ocular dominance, but there is less evidence connecting ocular dominance and monocular visual thresholds. We used the classic “hole in card” method to determine the dominant eye for 28 adult observers (11 males and 17 females). We then compared contrast thresholds between the dominant and non-dominant eyes using grating stimuli biased to be processed more strongly either by the magnocellular (MC) or parvocellular (PC) pathway. Using non-parametric mean rank tests, the dominant eye was more sensitive overall than the non-dominant eye to both stimuli (z = 2.54, p = 0.01). The dominant eye was also more sensitive − to the PC-biased stimulus (z = 2.22, p = 0.03) but not the MC-biased stimulus (z = 1.16, p = 0.25). We − − discuss the clinical relevance of these results as well as the implications for parallel visual pathways. Keywords: dominant eye; contrast; parvocellular; magnocellular 1. -

Vision Therapy and Post-Concussion Syndrome Management: a Case Report Elizabeth Murray OD, Katie Connolly OD
Vision Therapy and Post-Concussion Syndrome Management: A Case Report Elizabeth Murray OD, Katie Connolly OD Abstract: Current therapy for post-concussion syndrome with visual symptoms are to rest and decrease visual demand. This case looks at vision therapy for first line treatment when decreasing visual demand is not ideal. I. Case History On 5/30/2017, a 37 year old white male presented for persistent visual symptoms following a traumatic brain injury to the occipital lobe with torsion on the brain stem. The injury occurred on 4/3/2017 from a motor vehicle accident, and he had since been cleared from cognitive rest. At the time of the accident, he reported no loss of consciousness but did have post traumatic amnesia. Initially, he reported feeling fine, but his symptoms progressively worsened. He denied blur and diplopia, but was symptomatic for significant cognitive fatigue, gaze instability, visual stimuli triggered headaches, photophobia, and noise sensitivity. He is a pediatric oncologist with significant visual and cognitive demanding duties that exacerbate his symptoms. Ocular and medical history were unremarkable prior to the accident. At the time, he was taking Fioricet and Amitriptyline as directed for headaches and to aid in sleep, respectively. He had been seeing a Chiropractor for vestibular therapy that included some oculomotor therapy and planned to begin cognitive therapy at an outpatient rehabilitation hospital. II. Pertinent findings Entering distance visual acuities were 20/20 OD, OS and OU and near visual acuities were 20/20 OD, 20/25-1 OS, and 20/15-1 OU, without correction. Pupils and extraocular muscles were unremarkable. -

Routine Eye Examination
CET Continuing education Routine eye examination Part 3 – Binocular assessment In the third part of our series on the eye examination, Andrew Franklin and Bill Harvey look at the assessment and interpretation of binocular status. Module C8290, one general CET point, suitable for optometrists and DOs he assessment of binocular previous question. Leading questions function is often one of the should be avoided, especially when weaker areas of a routine, dealing with children. If they are out if observation of candidates of line ask the patient ‘Which one is out in the professional qualifica- of line with the X?’ Ttions examination is any guide. Tests are You should know before you start the done for no clearly logical reason, often test which line is seen by which eye. because they always have been, and in If you cannot remember it from last an order which defeats the object of the time, simply look at the target through testing. Binocular vision seems to be one the visor yourself (Figure 1). Even if of those areas that practitioners shy away you think you can remember, check from, and students often take an instant anyway, as it is possible for the polarisa- dislike to. Many retests and subsequent tion of the visor not to match that of the remakes of spectacles are the result of a Mallett Unit at distance or near or both, practitioner overlooking the effects of a Figure 1 A distance fixation disparity target especially if the visor is a replacement. change of prescription on the binocular If both eyes can see both bars, nobody status of the patient. -

Complete Directory
Complete Directory Name Primary Appointment Tel: (212) 938- xxxx Academic Programs Academic Affairs 5658 Fax Dean's Office Academic Affairs 5714 Pak, Jean Academic Affairs 4313 Vice President/Dean for Academic Academic Affairs 5515 Paulino, Yodania Accounts Payable 5669 Orehek, Frank Administration 5582 Vice President Administration and Administration and Finance 5666 Alumni Association Alumni Affairs 5603 Wall Phone 18th floor Alumni Alumni Commons Caf 5588 Lomparte, Francisco Alumni Relations 5604 Assoc Dean Graduate Program Associate Dean 5540 Alonso, Jose-Manuel Biological and Vision Sciences 5573 Aquilante, Kathy Biological and Vision Sciences 5775 Backus, Benjamin Biological and Vision Sciences 1541 Beaton, Ann Biological and Vision Sciences 5799 Bloomfield, Stewart Biological and Vision Sciences 5532 Ciuffreda, Kenneth Biological and Vision Sciences 5765 Duckman, Robert Biological and Vision Sciences 5857 Dul, Mitchell Biological and Vision Sciences 4164 Gundel, Ralph Biological and Vision Sciences 5868 Kruger, Philip Biological and Vision Sciences 5759 Llerena-Law, Christina Biological and Vision Sciences 4169 McPeek, Robert Biological and Vision Sciences 5762 Picarelli, John Biological and Vision Sciences 5784 Pola, Jordan Biological and Vision Sciences 5758 Rapp, Jerry Biological and Vision Sciences 5786 Reinach, Peter Biological and Vision Sciences 5938 Richdale, Kathryn Biological and Vision Sciences 4165 Rubinson, Kalman Biological and Vision Sciences N/A Sack LAB, Robert Biological and Vision Sciences 5793 Sack, Robert Biological -

Plan Q Full Benefit Description
B E N E F I T D E S C R I P T I O N State Employee Health Plan This booklet describes the health benefits that the Kansas State Employees Health Care Commission provides to Members and their Dependents. These benefits are funded by: The Kansas State Employees Health Care Commission Third Party Administrator (TPA): : Blue Cross Blue Shield of Kansas has been retained to administer claims under this Plan. The TPA provides Administrative Services Only pursuant to this Benefit Description, including claims processing and administration of appeals and grievances. For answers to questions regarding eligibility for benefits, payment of claims, and other information about this Plan contact: Blue Cross Blue Shield of Kansas 1133 SW Topeka Blvd Topeka, KS 66629 By Phone 785-291-4185 or Toll Free at 1-800-332-0307 www.bcbsks.com/state Company is not the insurer under this Program and does not assume any financial risk or obligation with respect to claims. Plan Q Benefit Description 2021 Section I Coverage ................................................................................................. 1 Part 1: General Provisions ................................................................................ 1 Responsibilities of the Third Party Administrator (TPA) ..................................... 1 Case Management/Cost Effective Care ............................................................ 1 How to Contact the TPA .................................................................................... 2 Services from Non Network Providers -
Year in Review Issue
Gregg’s LANDING The exclusiveG newsletter for the residentsLife of Gregg’s Landing January 2021 2020 YEAR IN REVIEW ISSUE YOUR STORIES. YOUR PHOTOS. YOUR COMMUNITY. New Year (finally), New You ! LEAVE IT TO TOPTEC $500 OFF! WE'LL TAKE CARE OF IT. YEAR END SPECIAL $85.00 BRACES Furnace Tune-up INVISALIGN Special *12/1/2020 - 1/31/2021 COMPREHENSIVE TREATMENT ONLY **COUPON MUST BE PRESENT Don't pay until 2021 when you nance a new Lennox* YOUR SPECIALIST FOR: systemfor as little as $132 a month. Early Treatment • Adult Treatment Plus get up to $1,200 in rebates. Ronald S. Jacobson Raymond Y. Tsou No contact service call policy – Techs. D.D.S., M.S. D.M.D., M.S. Diamond Plus Provider wears face masks, gloves & booties IL. Lic. #055-042909 Visit us Online Vernon Hills Office: Chicago Office: 280 W. Townline Rd. 4200 W. Peterson Ave. JTORTHO.COM Suite 220 Suite 116 Vernon Hills, IL 60061 Chicago, IL 60646 Visit our Doctors at our Vernon Hills or Chicago Location 847-816-0633 773-545-5333 2 Gregg's Landing Life • January 2021 January 2021 • Gregg's Landing Life 3 847-780-8200 You can purchase sessions, membership plans and gift cards... please call or Visit our Facebook page or website for promotions. Northshoresalt.com CONDITIONS BENEFITS • Asthma • Clear Pollens, Pollutants, Toxins & Airways • Cough • Reduce Bronchial Inflammation • Sinusitis • Relieve Skin Conditions such as Dermatitis, • COPD Eczema, & Psoriasis • Bronchitis • Improve Lung Function • Stress • Strengthen the Immune System against • Ear Infection Cold, Flu, & Lung Irritants • Allergies • Reduce Triggers that Promote Respiratory Illness • Eczema • Clean Nasal Cavities and Sinuses • Psoriasis • Cystic Fibrosis WE SELL 1282 Old Skokie Rd. -
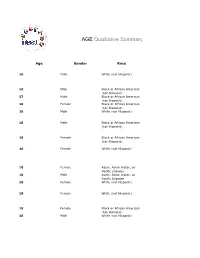
AGE Qualitative Summary
AGE Qualitative Summary Age Gender Race 16 Male White (not Hispanic) 16 Male Black or African American (not Hispanic) 17 Male Black or African American (not Hispanic) 18 Female Black or African American (not Hispanic) 18 Male White (not Hispanic) 18 Malel Blacklk or Africanf American (not Hispanic) 18 Female Black or African American (not Hispanic) 18 Female White (not Hispanic) 18 Female Asian, Asian Indian, or Pacific Islander 18 Male Asian, Asian Indian, or Pacific Islander 18 Female White (not Hispanic) 18 Female White (not Hispanic) 18 Female Black or African American (not Hispanic) 18 Male White (not Hispanic) 19 Male Hispanic (unspecified) 19 Female White (not Hispanic) 19 Female Asian, Asian Indian, or Pacific Islander 19 Male Asian, Asian Indian, or Pacific Islander 19 Male Asian, Asian Indian, or Pacific Islander 19 Female Native American or Alaskan Native 19 Female White (p(not Hispanic)) 19 Male Hispanic (unspecified) 19 Female Hispanic (unspecified) 19 Female White (not Hispanic) 19 Female White (not Hispanic) 19 Male Hispanic/Latino – White 19 Male Hispanic/Latino – White 19 Male Native American or Alaskan Native 19 Female Other 19 Male Hispanic/Latino – White 19 Male Asian, Asian Indian, or Pacific Islander 20 Female White (not Hispanic) 20 Female Other 20 Female Black or African American (not Hispanic) 20 Male Other 20 Male Native American or Alaskan Native 21 Female Don’t want to respond 21 Female White (not Hispanic) 21 Female White (not Hispanic) 21 Male Asian, Asian Indian, or Pacific Islander 21 Female White (not -

Effects of Nd:YAG Laser Capsulotomy in Posterior Capsular Opacification
Original Research Article Effects of Nd:YAG laser capsulotomy in posterior capsular opacification Praveen Kumar G S1, Lavanya P2*, Raviprakash D3 1Assistant Professor, 2Associate Professor, 3Professor & HOD, Department of Ophthalmology, Shridevi institute of Medical Sciences and Research Hospital, Sira Road, NH-4 Bypass Road, Tumkur- 572106, INDIA. Email: [email protected] Abstract Background: Posterior capsular opacification (PCO) is the most common long-term complication of cataract surgery in both phacoemulsification and extracapsular cataract extraction (ECCE). The overall incidence of PCO and the incidence of neodymium-doped yttrium–aluminum–garnet (Nd:YAG) laser posterior capsulotomy has decreased from 50% in the 1980s and early 1990s to less than 10% today. Reported complications of Nd:YAG laser posterior capsulotomy include elevated intraocular pressure, iritis, corneal damage, intraocular lens (IOL) damage, cystoids macular edema, disruption of the anterior hyaloid surface, increased risk of retinal detachment, and IOL movement or dislocation. In some patients, a refraction change is noticed after Nd:YAG laser posterior capsulotomy, but proving this remains difficult. Materials and Methods: Nd; YAG LASER capsulotomy was performed in 200 eyes of 200 patients, some with pseudophakia and some with aphakia at Kurnool medical college, Kurnool. They were followed up between October 2008 and September 2010. Results: Elevation of IOP has been well documented after anterior segment laser procedures. The IOP rise after YAG laser posterior capsulotomy is of short duration starting about 1 hr after laser procedure and lasting for 24 hrs. In this study, in 1case IOP came down to normal level after 3 days and in another case after 7 days. -

The Effect of the Fixation Disparity on Photogrammetric Processes
The Effect of the Fixation Disparity on Photogrammetric Processes SANDOR A. VERES, Asst. Proj., Surveying and Mapping, Purdue University ABSTRACT: This paper reviews the function oj the human eyes in photogram metry, and discusses its limitations. The correction of the observation error is presented by mathematical derivations and practical examples. The paper points out the need for continued development of techniques in view of con stantly increasing requirements. INTRODUCTION study of coincidence is most important from the photogrammetric point of view. For a HOTOGRAMMETRIC instrumentation has undergone a revolutionary development study of this kind an instrument called a P horopter has been used. since the second World War. A precision photogrammetric instrument today is able to The horopter designed by Tschermak con provide measurement to within a precision of sists of thirteen steel channels mounted so as ± 3 microns. By using these precision in to converge to the midpoint of the inter struments the compensation of errors in pupillary base line of the two eyes of an volved in the measurements becomes of pri observer. The central channel lies in a median mary importance. The compensation of errors plane, perpendicular to the eyebase of the is based upon the geometrical knowledge of observer, and the others make angles of 1, 2. the source of errors. The human eye is in 4, 8, 12, and 16 degrees on each side of the volved in every photogrammetric measure central channel. A small vertical steel rod can ment; consequently the geometrical knowl slide smoothly in each channel and the rods edge of the errors due to the limi tation of the are mounted for use at visual distances of 20, human eye is very important. -

G:\All Users\Sally\COVD Journal\COVD 37 #3\Maples
Essay Treating the Trinity of Infantile Vision Development: Infantile Esotropia, Amblyopia, Anisometropia W.C. Maples,OD, FCOVD 1 Michele Bither, OD, FCOVD2 Southern College of Optometry,1 Northeastern State University College of Optometry2 ABSTRACT INTRODUCTION The optometric literature has begun to emphasize One of the most troublesome and long recognized pediatric vision and vision development with the advent groups of conditions facing the ophthalmic practitioner and prominence of the InfantSEE™ program and recently is that of esotropia, amblyopia, and high refractive published research articles on amblyopia, strabismus, error/anisometropia.1-7 The recent institution of the emmetropization and the development of refractive errors. InfantSEE™ program is highlighting the need for early There are three conditions with which clinicians should be vision examinations in order to diagnose and treat familiar. These three conditions include: esotropia, high amblyopia. Conditions that make up this trinity of refractive error/anisometropia and amblyopia. They are infantile vision development anomalies include: serious health and vision threats for the infant. It is fitting amblyopia, anisometropia (predominantly high that this trinity of early visual developmental conditions hyperopia in the amblyopic eye), and early onset, be addressed by optometric physicians specializing in constant strabismus, especially esotropia. The vision development. The treatment of these conditions is techniques we are proposing to treat infantile esotropia improving, but still leaves many children handicapped are also clinically linked to amblyopia and throughout life. The healing arts should always consider anisometropia. alternatives and improvements to what is presently The majority of this paper is devoted to the treatment considered the customary treatment for these conditions. -

Visual Symptoms and Convergence Insufficiency in University Teachers
242ARTIGO ORIGINAL DOI 10.5935/0034-7280.20170050 Sintomas visuais e insuficiência de convergência em docentes universitários Visual symptoms and convergence insufficiency in university teachers Nágila Cristiana Menigite1, Marcelo Taglietti1 RESUMO Objetivo: Investigar a prevalência de desconforto visual e insuficiência de convergência (IC) em docentes universitários. Métodos: Tratar-se de um estudo transversal, com 60 docentes de ambos os sexos, tendo sido utilizado o questionário Convergence Insufficiency Symptom Survey, validado para a população brasileira. Resultados: Dos docentes entrevistados 55,0% eram do sexo feminino. 48,3% responderam dedicar menos que duas horas por dia à leitura, sendo que 40,0% dos entrevistados disseram que fazem pausas de 30 minutos à uma hora durante a leitura e 63,3% afirmaram passar entre 2 a 5 horas por dia em frente ao computador. Em relação à investigação sobre as doenças do sistema visual, 25,0% relataram apresentar miopia, sendo que 55,0% dos indivíduos usam óculos e destes 41,7% o usam com frequência. Quanto à investigação da prevalência de insuficiência de convergência, obteve-se frequência de (1,8) %. Conclusão: Constatou-se que a maioria dos entrevistados se apresentou com desconforto visual e uma pequena porcentagem foram acometidos pela IC. Descritores: Acuidade visual; Transtornos da motilidade ocular; Transtornos da visão; Visão binocular ABSTRACT Objective: To investigate the prevalence of visual discomfort and convergence failure in professors. Methods: A cross-sectional study was done, consisting of 60 teachers of both sexes, of the Centro Universitário FAG, which used the Convergence Insufficiency Symptom Survey, validated for the Brazilian population. Results: Of those surveyed 55.0% are female.