Common Questions About Infertility
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
When to Consider Tubal Reversal Vs IVF Success Rates Point to Greater Outcomes with IVF for Women in Their Mid-Thirties and Older
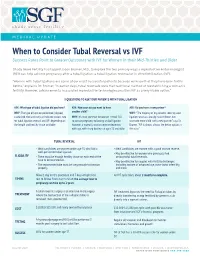
MEDICAL UPDATE When to Consider Tubal Reversal vs IVF Success Rates Point to Greater Outcomes with IVF for Women in their Mid-Thirties and Older Shady Grove Fertility has tapped Jason Bromer, M.D., to explore the two primary ways a reproductive endocrinologist (REI) can help achieve pregnancy after a tubal ligation: a tubal ligation reversal or in vitro fertilization (IVF). "Women with tubal ligations are some of our most successful patients because we know that they have been fertile before," explains Dr. Bromer. "In earlier days, tubal reversals were the traditional method of reestablishing a woman’s fertility. However, advancements in assisted reproductive technologies position IVF as a very viable option." 3 QUESTIONS TO ASK YOUR PATIENTS WITH TUBAL LIGATION ASK: What type of tubal ligation did you have? ASK: How soon do you want to have ASK: Do you have a new partner? WHY: The type of ligation performed (clipped, another child? WHY: "The majority of my patients seeking tubal cauterized, tied and cut) can indicate success rate WHY: It’s most common for women in their 30s ligation reversals already have children, but for tubal ligation reversal and IVF, depending on to pursue pregnancy following a tubal ligation. want one more child with a new partner," says Dr. the length and healthy tissue available. However, a woman’s ovarian reserve decreases Bromer. "IVF is almost always the better option in with age, with sharp declines at ages 35 and older. this case." TUBAL REVERSAL IVF • Ideal candidates are women under age 35 who had a • Ideal candidates are women with a good ovarian reserve. -

Female Fertility Assessment
Assessment Female Fertility Assessment Fertility challenges impact millions of couples in the United States and Medical conditions that impact the function of a woman’s ovaries, fallopian around the globe. Approximately 10% of US women ages 15-44 have tubes, or uterus can contribute to female infertility. Anovulation causes can difficulty getting or staying pregnant.1 Infertility is defined as the inability to include underweight, overweight/obesity, PCOS, endometriosis, diminished get pregnant after one year of trying (or six months in a woman 35 years or ovarian reserve (e.g., due to age), functional hypothalamic amenorrhea older) through unprotected sex.2 In addition to age and coital frequency,3 (FHA), dysfunction of the hypothalamus or pituitary gland, premature hormonal health has a major physiological influence on fertility. ovarian insufficiency, and menopause.2,13 In women, ovulation depends on a regular menstrual cycle, a 28-day Reproductive endocrinologists specialize in infertility and also support symphony of the hypothalamic-pituitary-gonadal (HPG) axis involving women who have experienced recurrent pregnancy loss; however, a specific fluctuations in estrogen and progesterone levels, shown in the multidisciplinary clinical team approach addressing hormonal, lifestyle, Figures in this assessment.4,5 The pituitary gland sends pulses of follicle- social support, and other factors is ideal. While this clinical tool focuses stimulating hormone (FSH) in the follicular phase (days 1-14), triggering on female fertility, it is important to point out that approximately 40% the rise of estrogen, which stimulates the hypothalamic release of of fertility cases involve a male factor (e.g., low sperm count or quality).3 gonadotropin-releasing hormone (GnRH), causing the pituitary secretion Thus, a couple’s approach to fertility assessment is prudent to uncover and of luteinizing hormone (LH).4,5 FSH and LH surges result in egg release from address underlying root causes preventing conception. -

Successful Pregnancies After Removal of Intratubal Microinserts
2. Tonni G, De Felice C, Centini G, Ginanneschi C. Cervical and 5. Levine AB, Alvarez M, Wedgwood J, Berkowitz RL, Holzman oral teratoma in the fetus: a systematic review of etiology, I. Contemporary management of a potentially lethal fetal pathology, diagnosis, treatment and prognosis. Arch Gynecol anomaly: a successful perinatal approach to epignathus. Obstet Obstet 2010;282:355–61. Gynecol 1990;76:962–6. 3. Calda P, Novotna M, Cutka D, Brestak M, Haslik L, Goldova 6. Berrington JE, Stafford FW, Macphail S. Emergency EXIT for B, et al. A case of an epignathus with intracranial extension preterm labour after FETO. Arch Dis Child Fetal Neonatal Ed appearing as a persistently open mouth at 16 weeks and 2010;95:F376–7. subsequently diagnosed at 20 weeks of gestation. J Clin Ultra- 7. Hedrick HL, Flake AW, Crombleholme TM, Howell LJ, sound 2011;39:164–8. Johnson MP, Wilson RD, et al. The ex utero intrapartum 4. Marwan A, Crombleholme TM. The EXIT procedure: principles, therapy procedure for high-risk fetal lung lesions. J Pediatr pitfalls, and progress. Semin Pediatr Surg 2006;15:107–15. Surg 2005;40:1038–44. Successful Pregnancies After and who would like to conceive have two options: in vitro fertilization and sterilization reversal. Successful Removal of Intratubal Microinserts pregnancies resulting from in vitro fertilization after intratubal microinsert sterilization have been described.2 Charles W. Monteith, MD, Based on a literature search of the entire PubMed and Gary S. Berger, MD, MPH database up to August 2011 (using the key words “Essure” and “pregnancy”), these are the first two re- BACKGROUND: Patients with intratubal microinsert ports of successful pregnancy after surgical outpatient sterilization later may request reversal. -

Monash Health Referral Guidelines – Gynaecology
Monash Health Referral Guidelines (Incorporating Statewide Referral Criteria) GYNAECOLOGY EXCLUSIONS Services not offered In Vitro Fertilisation by Monash Health CONDITIONS CONTRACEPTIVE COUNSELLING MENSTRUAL MANAGEMENT Contraception Persistent, heavy menstrual bleeding Pregnancy Choices Bartholin's cysts / vaginal lesions Post-Menopausal bleeding Post-Coital bleeding DYSPLASIA Persistent or unexplained intermenstrual Dysplasia/Abnormal Cervical bleeding Screening Test Fibroids Vulval ulcers Vulval disorders PELVIC FLOOR/UROGYNAECOLOGY Genital warts Pelvic organ prolapse Urinary incontinence Recurrent UTI’s GYNAECOLOGY ENDOSCOPY Ovarian and other adnexal pathology Dyspareunia REPRODUCTIVE MEDICINE Pelvic Inflammatory disease Infertility Persistent pelvic pain Amenorrhea Male infertility Recurrent miscarriages GYNAECOLOGY ONCOLOGY Tubal & vasectomy reversal Cancer of the cervix Endocrine problems (Polycystic Ovarian cancer Ovarian Syndrome) Gynae cancers -suspected and confirmed SEXUAL MEDICINE & THERAPY CLINIC Sexual & relationship counselling MENOPAUSE Turner 's Syndrome Cancer and menopause PAEDIATRIC & ADOLESCENT GYNAE Premature menopause Paediatric and Adolescent Gynaecology General menopause ENDOMETRIOSIS Endometriosis Head of unit: Program Director: Last updated: Professor Beverley Vollenhoven Associate Professor Ryan Hodges 06/02/2020 Monash Health Referral Guidelines (Incorporating Statewide Referral Criteria) GYNAECOLOGY PRIORITY For emergency cases please do any of the following: EMERGENCY - send the patient to the Emergency -

Prevalence Along with Diagnostic Modalities and Treatment of Female Infertility Due to Female Genital Disorders
Virology & Immunology Journal MEDWIN PUBLISHERS ISSN: 2577-4379 Committed to Create Value for Researchers Prevalence Along with Diagnostic Modalities and Treatment of Female Infertility Due to Female Genital Disorders Omer Iqbal1 and Faiza Naeem2* Research Article 1College of Medicine and Pharmacy, Ocean University of China Qingdao, Shandong province, Volume 4 Issue 3 China Received Date: August 16, 2020 2Institute of Pharmacy, Lahore College for Women University, Pakistan Published Date: September 08, 2020 DOI: 10.23880/vij-16000249 *Corresponding author: Faiza Naeem, Institute of Pharmacy, Lahore College for Women University, Lahore, Pakistan, Email: [email protected] Abstract Infertility is a communal pathological ailment now-a-days worldwide and approximately females are mostly suffering from this condition. In previous studies, out of 2.4 million married couples have females in between the ages from 15-44 year; 1.0 million couples were suffering from primary infertility and 1.4 million couples had secondary infertility. The infertility causes are ovulatory factors, dietary factors, psychological factors, abnormal endocrine functions, fallopian tube disorders etc. PCOS, PIDs, endometriosis. The ultrasonography is the most powerful tool for diagnosis. The treatment involves medical, surgical and assisted reproduction. Medical treatment includes clomiphene, metformin, iron & folic acid supplements along with oral- contraceptives. Surgical treatment is operative laparoscopy and assisted reproduction is achieved by IVF, GIFT & IUI etc. It is concluded from the study that the percentage prevalence of female infertility among ages was higher in age group (25-34) years (76%) and it was mostly secondary infertility (54%). The main pathological factor of female infertility in Sialkot city was PCOS, which was 52% of evaluated patients. -

Genetic Counseling and Diagnostic Guidelines for Couples with Infertility And/Or Recurrent Miscarriage
medizinische genetik 2021; 33(1): 3–12 Margot J. Wyrwoll, Sabine Rudnik-Schöneborn, and Frank Tüttelmann* Genetic counseling and diagnostic guidelines for couples with infertility and/or recurrent miscarriage https://doi.org/10.1515/medgen-2021-2051 to both partners prior to undergoing assisted reproduc- Received January 16, 2021; accepted February 11, 2021 tive technology. In couples with recurrent miscarriages, Abstract: Around 10–15 % of all couples are infertile, karyotyping is recommended to detect balanced structural rendering infertility a widespread disease. Male and fe- chromosomal aberrations. male causes contribute equally to infertility, and, de- Keywords: female infertility, male infertility, miscarriages, pending on the defnition, roughly 1 % to 5 % of all genetic counseling, ART couples experience recurrent miscarriages. In German- speaking countries, recommendations for infertile cou- ples and couples with recurrent miscarriages are pub- lished as consensus-based (S2k) Guidelines by the “Ar- Introduction beitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften” (AWMF). This article summarizes the A large proportion of genetic consultation appointments current recommendations with regard to genetic counsel- is attributed to infertile couples and couples with recur- ing and diagnostics. rent miscarriages. Infertility, which is defned by the WHO Prior to genetic counseling, the infertile couple as the inability to achieve a pregnancy after one year of must undergo a gynecological/andrological examination, unprotected intercourse [1], afects 10–15 % of all couples, which includes anamnesis, hormonal profling, physical thus rendering infertility a widespread disease, compara- examination and genital ultrasound. Women should be ex- ble to, e. g., high blood pressure or depression. Histori- amined for the presence of hyperandrogenemia. Men must cally, the female partner has been the focus of diagnos- further undergo a semen analysis. -

A Personal Choice with Dr. Monteith Where Permanent
A Personal Choice With Dr. Monteith Where Permanent THE MAGAZINE Is Not Forever FOR HEALTHCARE PROFESSIONALS A Personal Choice with Dr. Monteith Specializing in Male and Female Sterilization Reversal and No-Needle No-Scalpel Vasectomy Women and men travel across the United Many within the medical community re- The new practice name is a reflection of States and around the world to A Personal call the practice when it was Chapel Hill the broader vision, says Dr. Monteith. “Our Choice of Raleigh, a unique practice dedi- Tubal Reversal Center, founded by Gary S. new name may not be understandable to cated to outpatient, minimally invasive Berger, M.D. Dr. Monteith joined Dr. Berger the general public but for those who seek sterilization and sterilization reversal ser- there in 2008, and together they provided our services the immense meaning of our vices in a state-of-the-art facility. a unique form of tubal ligation reversal name is readily apparent,” he says. that allows faster patient recovery, avoids The surgical specialty practice exclusively prolonged hospitalization and decreases A Personal Choice is conveniently located offers tubal ligation reversal, and vasec- patient recovery time. near North Hills Mall and Midtown Raleigh, tomy and vasectomy reversal. Tubal rever- so patients can stay in one of the nearby sal and vasectomy reversal have proven to After Dr. Berger retired in 2013, Dr. Monte- luxury hotels and walk to many restaurants be more effective and are more affordable ith expanded on his health care vision by and entertainment venues. The area also than alternative treatments, and vasectomy giving male patients greater reproductive provides closer access to Raleigh Durham is safer than tubal ligation. -

Post Sterilization Tuboplasty: Boon Or Bain !
Indian Journal of Obstetrics and Gynecology Case Report 107 Volume 5 Number 1, January - March 2017 DOI: http://dx.doi.org/10.21088/ijog.2321.1636.5117.19 Post Sterilization Tuboplasty: Boon or Bain ! Mukti S. Harne*, Sumedha Harne**, Urmila Gavali*** Abstract fertilization for the next pregnancy, leading to compulsion on women to undergo tubal reversal. The incidence of a successful India is developing country, yet pregnancy after tubal ligation is 40%. There the development is less in the are many predisposing factors for the success medical sector. Though the of the pregnancy like the tubal length after awareness of tubal ligation is vividly surgery should be >4 cm, absence of present in the rural set up, pressure hydrosalpingnx and previous birth within on females are increasing due to 5 years [1]. preference of male child in the society. Some unfortunate We, at our institution encountered, an circumstances, may it be pressure unfortunate case of a couple, with history of from the family members or secondary infertility and belonging to the unfortunate death of the existing muslim community, who were anxious to children or poor economic status of conceive since 3 years and weren’t the family to afford the In vitro investigated previously. This 24 years, fertilization for the next pregnancy, Shabana Shaikh, P1D1, housewife by leading to compulsion on women to occupation and resident of Ahmednagar, undergo tubal reversal. Hence, this came with her husband in the gynaec opd. case was brought to notice,while Detailed history of the couple was taken . emphasis was laid on the surgical Her menstrual history was regular, management of a case that we monthly interval, soaking 1-2 pads per day, managed. -

Diagnostic Testing for Female Infertility
Fact Sheet From ReproductiveFacts.org The Patient Education Website of the American Society for Reproductive Medicine Diagnostic Testing for Female Infertility An evaluation of a woman for infertility is appropriate for women over age 35 years; 2) have a family history of early menopause; 3) who have not become pregnant after having 12 months of regular, have a single ovary; 4) have a history of previous ovarian surgery, unprotected intercourse. Being evaluated earlier is appropriate chemotherapy, or pelvic radiation therapy; 5) have unexplained after six months for women who are older than age 35 or who have infertility; or 6) have shown poor response to gonadotropin ovarian one of the following in their medical history or physical examination: stimulation. • History of irregular menstrual cycles (over 35 days apart or no periods at all) Other Blood Tests: Thyroid-stimulating hormone (TSH) and • Known or suspected problems with the uterus (womb), tubes, prolactin levels are useful to identify thyroid disorders and or other problems in the abdominal cavity (like endometriosis hyperprolactinemia, which may cause problems with fertility, or adhesions) menstrual irregularities, and repeated miscarriages. In women • Known or suspected male infertility problems who are thought to have an increase in hirsutism (including hair on the face and/or down the middle of the chest or abdomen), Any evaluation for infertility should be done in a focused and cost- blood tests for dehydroepiandrosterone sulfate (DHEAS), 17-α effective way to find all relevant factors, and should include the hydroxyprogesterone, and total testosterone should be considered. male as well as female partners. The least invasive methods A blood progesterone level drawn in the second half of the menstrual that can detect the most common causes of infertility should be cycle can help document whether ovulation has occurred. -

Infertility in the Military
Updated May 26, 2021 Infertility in the Military In recent years, Congress has become increasingly 8,744 were diagnosed with infertility from 2013 to 2018. interested in the provision of infertility services and During this same time period, the annual incidence rate of expanded reproductive care for servicemembers. Federal infertility diagnoses decreased by 25.3% (from 85.1 per regulation (32 C.F.R. §199.4(g)) generally prohibits the 10,000 to 63.6 per 10,000 [see Figure 1]); while the Department of Defense (DOD) from paying for certain average annual prevalence of diagnosed female infertility infertility services for most servicemembers and other decreased by 18% (from 173.6 per 10,000 to 142.3 per beneficiaries eligible for the TRICARE program. Some 10,000 [see Figure 2]). Members of Congress argue that TRICARE coverage of Figure 1. Annual incidence rates of female infertility infertility services is an essential benefit to recruit and retain an all-volunteer force, while others express concern diagnoses, active component servicewomen of childbearing potential, 2013-2018 that expanded coverage would make the benefit too costly. This In Focus describes the prevalence of infertility among servicemembers, available treatment options, and considerations when addressing expanded TRICARE coverage of infertility services for servicemembers. Background The U.S. Centers for Disease Control and Prevention (CDC), defines infertility as “not being able to conceive after one year of regular, unprotected sexual intercourse.” Some health care providers, military and civilian, choose to evaluate and treat females over age 35 after 6 months of unprotected intercourse. Any condition affecting the ovaries, fallopian tubes and/or uterus can result in infertility among females. -

Endometriosis-Related Infertility: Ovarian Endometrioma Per Se Is Not Associated with Presentation for Infertility
Human Reproduction, Vol.31, No.8 pp. 1765–1775, 2016 Advanced Access publication on April 29, 2016 doi:10.1093/humrep/dew093 ORIGINAL ARTICLE Infertility Endometriosis-related infertility: ovarian endometrioma per se is not associated with presentation for infertility P. Santulli1,2,3, M.C. Lamau1, L. Marcellin1,3,V.Gayet1, P. Marzouk1, B. Borghese1,2, Marie-Christine Lafay Pillet1, and C. Chapron1,2,* 1Service de Chirurgie Gyne´cologie Obste´trique II et Me´decine de la Reproduction, Universite´ Paris Descartes, Sorbonne Paris Cite´, Faculte´ de Me´decine, Assistance Publique – Hoˆpitaux de Paris (AP-HP), Hoˆpital Universitaire Paris Centre (HUPC), Centre Hospitalier Universitaire (CHU) Cochin, Paris, France 2Equipe Ge´nomique, Epige´ne´tique et Physiopathologie de la Reproduction, De´partement De´veloppement, Reproduction, Cancer, Inserm U1016, Universite´ Paris Descartes, Sorbonne Paris Cite´, Faculte´ de Me´decine, AP-HP, HUPC, CHU Cochin, Paris,France 3Equipe Stress Oxydant, Prolife´ration Cellulaire et Inflammation, De´partement De´veloppement, Reproduction, Cancer, Inserm U1016, Universite´ Paris Descartes, Sorbonne Paris Cite´, Faculte´ de Me´decine, AP-HP, HUPC, CHU Cochin, Paris, France *Correspondence address. Service de Chirurgie Gyne´cologie Obste´trique II et Me´decine de la Reproduction, Baˆtiment Port Royal, CHU Cochin, 53 avenue de l’Observatoire, 75679 Paris 14, France. Tel: +33-1-58-41-36-69; Fax: +33-1-58-41-36-68; E-mail: [email protected] Submitted on November 2, 2015; resubmitted on February 24, 2016; accepted on March 23, 2016 study question: Is there an association between the endometriosis phenotype and presentation with infertility? summaryanswer: In a population of operated patients with histologically proven endometriosis, ovarian endometrioma (OMA) per se is not associated with an increased risk of presentation with infertility, while previous surgery for endometriosis was identified as a risk factor for infertility. -

Tubal Ligation Reversal (English)
Tubal Ligation Reversal What is tubal ligation reversal? Tubal ligation reversal is an operation that may be done in some cases after you have had tubal sterilization. Tubal sterilization, also called tubal ligation or having your tubes tied, is a permanent way to prevent pregnancy by surgically closing a woman's fallopian tubes. It is considered to be a permanent type of birth control. Normally, the fallopian tubes carry the eggs from the ovaries to the uterus. Tubal ligation closes the tubes by cutting, tying, clipping, or burning the tubes, or by plugging the opening of the tubes. It prevents pregnancy because it stops sperm from reaching and fertilizing eggs after you have sex. It also prevents eggs from reaching the inside of the uterus (womb). Tubal ligation reversal is an operation to try to reconnect or unblock the fallopian tubes so that you may be able to get pregnant again, naturally. Tubal ligation reversal is difficult, expensive, and often not successful. Health insurance may not cover the cost. Talk to your healthcare provider to see if this procedure is right for you. When is this procedure used? If you decide that you want to become pregnant again after sterilization, having surgery to reverse tubal ligation is one way that might make this possible. It does not always work, but it may be less expensive than other procedures. If it is successful, you will not likely need any other treatments to have more children. Another way to try to get pregnant after sterilization is assisted reproduction technology (ART). When ART is done, eggs are removed from your body and fertilized with the father’s sperm in a lab.