Lower-Extremity Peripheral Nerve Blockade: Essentials of Our Current Understanding
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(12) United States Patent (10) Patent No.: US 7,074,961 B2 Wang Et Al
US007074961B2 (12) United States Patent (10) Patent No.: US 7,074,961 B2 Wang et al. (45) Date of Patent: Jul. 11, 2006 (54) ANTIDEPRESSANTS AND THEIR 6.211,171 B1 4/2001 Sawynok et al. ANALOGUES AS LONG-ACTING LOCAL 6,545,057 B1 4/2003 Wang et al. ANESTHETCS AND ANALGESCS 2001/0036943 A1 11/2001 Coe et al. (75) Inventors: Ging Kuo Wang, Westwood, MA (US); FOREIGN PATENT DOCUMENTS Peter Gerner, Weston, MA (US); Donald K. Verrecchia, Winchester, MA CH 534124 A 2, 1973 (US) WO WO95/17903 A1 7, 1995 WO WO95/1818.6 A1 7, 1995 (73) Assignee: The Brigham and Women's Hospital, WO WO 99.59.598 A1 11, 1999 Inc., Boston, MA (US) WO WO O2/060870 A2 8, 2002 (*) Notice: Subject to any disclaimer, the term of this OTHER PUBLICATIONS patent is extended or adjusted under 35 U.S.C. 154(b) by 451 days. Luo et al., Xenobiotica, vol. 25, No. 3, pp. 291-301, 1995.* (21) Appl. No.: 10/117,708 Ehlert et al., The Interaction of Amitriptyline, Doxepin, Imipramine and Their N-Methyl Quaternary Ammonium (22) Filed: Apr. 4, 2002 Derivatives with Subtypes of Muscarinic Receptors in Brain (65) Prior Publication Data and Heart, The Journal of Pharmacology and Experimental Therapeutics, Apr. 1990, vol. 253, No. 1, pp. 13–19. US 2003/00968.05 A1 May 22, 2003 Gerner, P., et al., Anesthesiology (2002) 96:1435–42. Related U.S. Application Dat e pplication Uata Khan, M.A., et al., Anesthesiology (2002) 96:109–16. (63) stripps'965,138, filed on Sep. -

Bilateral Anomalous Muscle in the Popliteal Fossa & Its Clinical
International Journal of Anatomy and Research, Int J Anat Res 2014, Vol 2(4):614-16. ISSN 2321- 4287 Case Report DOI: 10.16965/ijar.2014.501 BILATERAL ANOMALOUS MUSCLE IN THE POPLITEAL FOSSA & ITS CLINICAL SIGNIFICANCE Sowmya S *, Meenakshi Parthasarathi, Sharmada KL, Sujana M. Department of anatomy, Bangalore Medical College & Research Institute, Bangalore, India. ABSTRACT Muscle variation may occur due to genetic or developmental causes. Some variations may compromise the vascular, muscular or nervous system in the region. Bilateral muscle variation in popliteal fossa is very rare. In present study an instance of bilateral muscle variation in popliteal fossa, arising from different muscles like gastrocnemius and from biceps femoris is recorded. There is no report of such variations. These observations are rare of its kind because of bilateral asymmetrical presence and difference in the origins in different legs. This is the first report as for the literatures available. Clinical and functional importance of such variation is discussed with the morphological aspects of this anomalous muscle. KEY WORDS: Popliteal fossa, Gastrocnemius, Biceps femoris, Popliteal Artery Entrapment Syndrome. Address for Correspondence: Dr.Sowmya S, Assistant Professor, Department of Anatomy, Bangalore Medical College & Research Institute, Bangalore-560002, India. Mobile: +919482476545. E-Mail: [email protected] Access this Article online Quick Response code Web site: International Journal of Anatomy and Research ISSN 2321-4287 www.ijmhr.org/ijar.htm Received: 08 Sep 2014 Peer Review: 08 Sep 2014 Published (O):31 Oct 2014 DOI: 10.16965/ijar.2014.501 Accepted: 22 Sep 2014 Published (P):31 Dec 2014 INTRODUCTION Insertion of muscle slips from biceps femoris into gastrocnemius and into tendocalcaneus have The popliteal fossa is a rhomboidal region been reported [3]. -

Clinical Presentations of Lumbar Disc Degeneration and Lumbosacral Nerve Lesions
Hindawi International Journal of Rheumatology Volume 2020, Article ID 2919625, 13 pages https://doi.org/10.1155/2020/2919625 Review Article Clinical Presentations of Lumbar Disc Degeneration and Lumbosacral Nerve Lesions Worku Abie Liyew Biomedical Science Department, School of Medicine, Debre Markos University, Debre Markos, Ethiopia Correspondence should be addressed to Worku Abie Liyew; [email protected] Received 25 April 2020; Revised 26 June 2020; Accepted 13 July 2020; Published 29 August 2020 Academic Editor: Bruce M. Rothschild Copyright © 2020 Worku Abie Liyew. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Lumbar disc degeneration is defined as the wear and tear of lumbar intervertebral disc, and it is mainly occurring at L3-L4 and L4-S1 vertebrae. Lumbar disc degeneration may lead to disc bulging, osteophytes, loss of disc space, and compression and irritation of the adjacent nerve root. Clinical presentations associated with lumbar disc degeneration and lumbosacral nerve lesion are discogenic pain, radical pain, muscular weakness, and cutaneous. Discogenic pain is usually felt in the lumbar region, or sometimes, it may feel in the buttocks, down to the upper thighs, and it is typically presented with sudden forced flexion and/or rotational moment. Radical pain, muscular weakness, and sensory defects associated with lumbosacral nerve lesions are distributed on -

Piriformis Syndrome Is Overdiagnosed 11 Robert A
American Association of Neuromuscular & Electrodiagnostic Medicine AANEM CROSSFIRE: CONTROVERSIES IN NEUROMUSCULAR AND ELECTRODIAGNOSTIC MEDICINE Loren M. Fishman, MD, B.Phil Robert A.Werner, MD, MS Scott J. Primack, DO Willam S. Pease, MD Ernest W. Johnson, MD Lawrence R. Robinson, MD 2005 AANEM COURSE F AANEM 52ND Annual Scientific Meeting Monterey, California CROSSFIRE: Controversies in Neuromuscular and Electrodiagnostic Medicine Loren M. Fishman, MD, B.Phil Robert A.Werner, MD, MS Scott J. Primack, DO Willam S. Pease, MD Ernest W. Johnson, MD Lawrence R. Robinson, MD 2005 COURSE F AANEM 52nd Annual Scientific Meeting Monterey, California AANEM Copyright © September 2005 American Association of Neuromuscular & Electrodiagnostic Medicine 421 First Avenue SW, Suite 300 East Rochester, MN 55902 PRINTED BY JOHNSON PRINTING COMPANY, INC. ii CROSSFIRE: Controversies in Neuromuscular and Electrodiagnostic Medicine Faculty Loren M. Fishman, MD, B.Phil Scott J. Primack, DO Assistant Clinical Professor Co-director Department of Physical Medicine and Rehabilitation Colorado Rehabilitation and Occupational Medicine Columbia College of Physicians and Surgeons Denver, Colorado New York City, New York Dr. Primack completed his residency at the Rehabilitation Institute of Dr. Fishman is a specialist in low back pain and sciatica, electrodiagnosis, Chicago in 1992. He then spent 6 months with Dr. Larry Mack at the functional assessment, and cognitive rehabilitation. Over the last 20 years, University of Washington. Dr. Mack, in conjunction with the Shoulder he has lectured frequently and contributed over 55 publications. His most and Elbow Service at the University of Washington, performed some of the recent work, Relief is in the Stretch: End Back Pain Through Yoga, and the original research utilizing musculoskeletal ultrasound in order to diagnose earlier book, Back Talk, both written with Carol Ardman, were published shoulder pathology. -
Bone Grafts and Implants in Spine Surgery
CHAPTER 39 BONE GRAFTS AND IMPLANTS IN SPINE SURGERY Ken Hsu James F. Zucherman Arthur H. White Recent advances in both fusion tech of scaffolds, bridges, spacers, fillers of J • niques and instrumentation have defects, and replacements of bone lost. markedly facilitated the treatment of Immobilization of multiple motion seg spinaldisorders. Yet asignificantnumber ments is frequently necessary in the spine; of patients exist who continue to have great demands arc made on bone grafts. pseudarthroses. Despite the surgical ad In the lumbosacral spine, body weight vances the essentials ofa successful spinal and muscular forcesimpart loads equal to fusion still appear to be the effective ap three or four times body weight. It is plication of sound bone grafting princi not surprising that the highest rate of ples. These principles, along with the bone graft failure is seen in the lumbo techniques, problems, and complications sacral spine. Hence, the following is a associated with bone grafting, arc re discussion of technical problems, bio- viewed in this chapter. mechanical and physiologic character The loss ofbone in the spine often pre istics of bone grafts, and implants. sents serious difficulties not seen in other areas. The most favorable replacement THE AUTOGRAFT would still be a bone graft that fills the Autograft, or bone graft transplanted defect and becomes incorporated into the from one site to another in the same indi spine. However, the availability of ap vidual, is considered to be the most bio propriate bone to replace the loss is a logically suitable. Its advantages include: significant problem. Alternatives to bone 1. -

The Square Flap Technique for Burn Contractures: Clinical Experience and Analysis of Length Gain
Annals of Burns and Fire Disasters - vol. XXXI - n. 4 - December 2018 THE SQUARE FLAP TECHNIQUE FOR BURN CONTRACTURES: CLINICAL EXPERIENCE AND ANALYSIS OF LENGTH GAIN DOUBLE LAMBEAU RHOMBOÏDE POUR BRIDE SÉQUELLAIRE DE BRÛ- LURE: EXPÉRIENCE PRATIQUE ET ANALYSE DE LA LONGUEUR GAGNÉE Hifny M.A. Department of Plastic Surgery, Faculty of Medicine, Qena University Hospital, South Valley University, Egypt SUMMARY. Post-burn contractures, affecting the joints especially, are demanding problems. Many surgical techniques have been designated for burn contracture release. The aim of this study is to investigate the efficiency of the square flap technique to release a post-burn scar contracture, and assess the post-operative length gain that can be achieved by simple mathematical calculation. In this study, sixteen patients with linear contracture bands were treated with the square flap tech- nique. The anatomical distribution of the contractures was: axilla, cubital fossa, flank, perineum and popliteal fossa. Scar maturity ranged from 4 months - 9 years. Square flap width and contracture band length before and immediately after surgery were recorded by simple mathematical calculation. Flap complication was assessed. Patient satisfaction was also assessed during the follow-up period. All square flaps were effective in lengthening the contracture bands. The length of the contracture that was released ranged from 2 to 6 cm. The gain in length provided with this technique ranged from 212 to 350%, average 247%, and adequate contracture release was achieved in all cases postoperatively. All square flaps healed uneventfully except for one (6%), which demonstrated limited epidermolysis that healed by secondary intention. The fol- low-up interval ranged from 6 months to 1.5 years. -

Sensory Conduction in Medial and Lateral Plantar Nerves
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.51.2.188 on 1 February 1988. Downloaded from Journal ofNeurology, Neurosurgery, and Psychiatry 1988;51:188-191 Sensory conduction in medial and lateral plantar nerves S N PONSFORD From the Department of Clinical Neurophysiology, Walsgrave Hospital, Coventry, UK SUMMARY A simple and reliable method of recording medial and lateral plantar nerve sensory action potentials is described. Potentials are recorded with surface electrodes at the ankle using surface electrodes stimulating orthodromically at the sole. The normal values obtained are higher in amplitude than those obtained by the method described by Guiloff and Sherratt and are detectable in older subjects aged over 80 years. The procedure is valuable in the diagnosis of early peripheral neuropathy, mononeuritig multiplex; tarsal tunnel syndrome and in differentiation between pre and post ganglionic L5 SI lesions. The value of medial plantar sensory action potential EL53051 applied to the sole just lateral to the first meta-guest. Protected by copyright. (SAP) recording in the diagnosis of peripheral neuro- tarsal, the anode level with metatarsophalangeal joint, the pathy and investigation of root or individual nerve cathode thus overlying the first common digital nerve sub- lesions involving the leg or foot was clearly estab- serving contiguous surfaces ofthe great and second toes. For the lateral plantar, the stimulator was placed between the lished by Guiloff and Sherratt.1 However, their fourth and fifth metatarsals, the anode-again level with the method of stimulating at the big toe and recording at metatarsophalangeal joint, overlying the fourth common the ankle gives potentials of relatively small ampli- digital nerve supplying contiguous surfaces of the fourth and tude (mean amplitude 2-3 pv, range 0-8- 1). -

Femoral and Sciatic Nerve Blocks for Total Knee Replacement in an Obese Patient with a Previous History of Failed Endotracheal Intubation −A Case Report−
Anesth Pain Med 2011; 6: 270~274 ■Case Report■ Femoral and sciatic nerve blocks for total knee replacement in an obese patient with a previous history of failed endotracheal intubation −A case report− Department of Anesthesiology and Pain Medicine, School of Medicine, Catholic University of Daegu, Daegu, Korea Jong Hae Kim, Woon Seok Roh, Jin Yong Jung, Seok Young Song, Jung Eun Kim, and Baek Jin Kim Peripheral nerve block has frequently been used as an alternative are situations in which spinal or epidural anesthesia cannot be to epidural analgesia for postoperative pain control in patients conducted, such as coagulation disturbances, sepsis, local undergoing total knee replacement. However, there are few reports infection, immune deficiency, severe spinal deformity, severe demonstrating that the combination of femoral and sciatic nerve blocks (FSNBs) can provide adequate analgesia and muscle decompensated hypovolemia and shock. Moreover, factors relaxation during total knee replacement. We experienced a case associated with technically difficult neuraxial blocks influence of successful FSNBs for a total knee replacement in a 66 year-old the anesthesiologist’s decision to perform the procedure [1]. In female patient who had a previous cancelled surgery due to a failed tracheal intubation followed by a difficult mask ventilation for 50 these cases, peripheral nerve block can provide a good solution minutes, 3 days before these blocks. FSNBs were performed with for operations on a lower extremity. The combination of 50 ml of 1.5% mepivacaine because she had conditions precluding femoral and sciatic nerve blocks (FSNBs) has frequently been neuraxial blocks including a long distance from the skin to the used for postoperative pain control after total knee replacement epidural space related to a high body mass index and nonpalpable lumbar spinous processes. -

Femoral Nerve Block Versus Spinal Anesthesia for Lower Limb
Alexandria Journal of Anaesthesia and Intensive Care 44 Femoral Nerve Block versus Spinal Anesthesia for Lower Limb Peripheral Vascular Surgery By Ahmed Mansour, MD Assistant Professor of Anesthesia, Faculty of Medicine, Alexandria University. Abstract Perioperative cardiac complications occur in 4% to 6% of patients undergoing infrainguinal revascularization under general, spinal, or epidural anesthesia. The risk may be even greater in patients whose cardiac disease cannot be fully evaluated or treated before urgent limb salvage operations. Prompted by these considerations, we investigated the feasibility and results of using femoral nerve block with infiltration of the genito4femoral nerve branches in these high-risk patients. Methods: Forty peripheral vascular reconstruction of lower limbs were performed under either spinal anesthesia (20 patients) or femoral nerve block with infiltration of genito-femoral nerve branches supplemented with local infiltration at the site of dissection as needed (20 patients). All patients had arterial lines. Arterial blood pressure and electrocardiographic monitoring was continued during surgery, in PACU and in the intensive care units. Results: Operations included femoral-femoral, femoral-popliteal bypass grafting and thrombectomy. The intra-operative events showed that the mean time needed to perform the block and dose of analgesics and sedatives needed during surgery was greater in group I (FNB,) compared to group II [P=0.01*, P0.029* , P0.039*], however, the time needed to start surgery was shorter in group I than in group II [P=0. 039]. There were no block failures in either group, but local infiltration in the area of the dissection with 2 ml (range 1-5 ml) of 1% lidocaine was required in 4 (20%) patients in FNB group vs none in the spinal group. -

Compiled for Lower Limb
Updated: December, 9th, 2020 MSI ANATOMY LAB: STRUCTURE LIST Lower Extremity Lower Extremity Osteology Hip bone Tibia • Greater sciatic notch • Medial condyle • Lesser sciatic notch • Lateral condyle • Obturator foramen • Tibial plateau • Acetabulum o Medial tibial plateau o Lunate surface o Lateral tibial plateau o Acetabular notch o Intercondylar eminence • Ischiopubic ramus o Anterior intercondylar area o Posterior intercondylar area Pubic bone (pubis) • Pectineal line • Tibial tuberosity • Pubic tubercle • Medial malleolus • Body • Superior pubic ramus Patella • Inferior pubic ramus Fibula Ischium • Head • Body • Neck • Ramus • Lateral malleolus • Ischial tuberosity • Ischial spine Foot • Calcaneus Ilium o Calcaneal tuberosity • Iliac fossa o Sustentaculum tali (talar shelf) • Anterior superior iliac spine • Anterior inferior iliac spine • Talus o Head • Posterior superior iliac spine o Neck • Posterior inferior iliac spine • Arcuate line • Navicular • Iliac crest • Cuboid • Body • Cuneiforms: medial, intermediate, and lateral Femur • Metatarsals 1-5 • Greater trochanter • Phalanges 1-5 • Lesser trochanter o Proximal • Head o Middle • Neck o Distal • Linea aspera • L • Lateral condyle • L • Intercondylar fossa (notch) • L • Medial condyle • L • Lateral epicondyle • L • Medial epicondyle • L • Adductor tubercle • L • L • L • L • 1 Updated: December, 9th, 2020 Lab 3: Anterior and Medial Thigh Anterior Thigh Medial thigh General Structures Muscles • Fascia lata • Adductor longus m. • Anterior compartment • Adductor brevis m. • Medial compartment • Adductor magnus m. • Great saphenous vein o Adductor hiatus • Femoral sheath o Compartments and contents • Pectineus m. o Femoral canal and ring • Gracilis m. Muscles & Associated Tendons Nerves • Tensor fasciae lata • Obturator nerve • Iliotibial tract (band) • Femoral triangle: Boundaries Vessels o Inguinal ligament • Obturator artery o Sartorius m. • Femoral artery o Adductor longus m. -
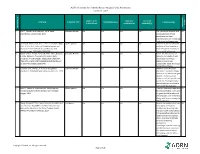
AORN Guideline for Patients Receiving Local-Only Anesthesia Evidence Table
AORN Guideline for Patients Receiving Local-Only Anesthesia Evidence Table SAMPLE SIZE/ CONTROL/ OUTCOME CITATION EVIDENCE TYPE INTERVENTION(S) CONCLUSION(S) POPULATION COMPARISON MEASURE(S) SCORE CONSENSUS REFERENCE # REFERENCE 1 Lirk P., Picardi S. and Hollmann, M. W. Local Literature Review n/a n/a n/a n/a The mechanism of action and VA anaesthetics: 10 essentials. 2014 access pathways of local anesthetics and their pharmokinetics are increasingly understood and appreciated. 2 Calatayud, Jesús, M.D.,D.D.S., Ph.D., González, Õngel, Expert Opinion n/a n/a n/a n/a A review of the discovery and VA M.D., D.D.S., Ph.D. History of the development and evolution of local anesthesia evolution of local anesthesia since the coca leaf. from the Spanish discovery of Anesthesiology. 2003;98(6):1503-1508. the coca leaf in America. 3 Gordh T, M.D., Gordh, Torsten E.,M.D., Ph.D., Lindqvist Literature Review n/a n/a n/a n/a Before the introduction of VA K, M.Sc. Lidocaine: The origin of a modern local lidocaine, the choice of local anesthetic. Anesthesiology. 2010;113(6):1433-1437. anesthetics was limited. https://doi.org/10.1097/ALN.0b013e3181fcef48. doi: Lidocaine's onset was 10.1097/ALN.0b013e3181fcef48. substantially faster and longer lasting than procaine. 4 Volcheck G.W., Mertes, P. M. Local and general Literature Review n/a n/a n/a n/a Whether to test the local VA anesthetics immediate hypersensitivity reactions. 2014 anesthetic causing the allergic reaction or an alternative agent depends on the expected future need of the specific local anesthetic. -

Study of Anatomical Pattern of Lumbar Plexus in Human (Cadaveric Study)
54 Az. J. Pharm Sci. Vol. 54, September, 2016. STUDY OF ANATOMICAL PATTERN OF LUMBAR PLEXUS IN HUMAN (CADAVERIC STUDY) BY Prof. Gamal S Desouki, prof. Maged S Alansary,dr Ahmed K Elbana and Mohammad H Mandor FROM Professor Anatomy and Embryology Faculty of Medicine - Al-Azhar University professor of anesthesia Faculty of Medicine - Al-Azhar University Anatomy and Embryology Faculty of Medicine - Al-Azhar University Department of Anatomy and Embryology Faculty of Medicine of Al-Azhar University, Cairo Abstract The lumbar plexus is situated within the substance of the posterior part of psoas major muscle. It is formed by the ventral rami of the frist three nerves and greater part of the fourth lumbar nerve with or without a contribution from the ventral ramus of last thoracic nerve. The pattern of formation of lumbar plexus is altered if the plexus is prefixed (if the third lumbar is the lowest nerve which enters the lumbar plexus) or postfixed (if there is contribution from the 5th lumbar nerve). The branches of the lumbar plexus may be injured during lumbar plexus block and certain surgical procedures, particularly in the lower abdominal region (appendectomy, inguinal hernia repair, iliac crest bone graft harvesting and gynecologic procedures through transverse incisions). Thus, a better knowledge of the regional anatomy and its variations is essential for preventing the lesions of the branches of the lumbar plexus. Key Words: Anatomical variations, Lumbar plexus. Introduction The lumbar plexus formed by the ventral rami of the upper three nerves and most of the fourth lumbar nerve with or without a contribution from the ventral ramous of last thoracic nerve.