2SPD-032 Network Meta-Analysis of Therapeutic Alternatives in Untreated
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cancer Drug Pharmacology Table
CANCER DRUG PHARMACOLOGY TABLE Cytotoxic Chemotherapy Drugs are classified according to the BC Cancer Drug Manual Monographs, unless otherwise specified (see asterisks). Subclassifications are in brackets where applicable. Alkylating Agents have reactive groups (usually alkyl) that attach to Antimetabolites are structural analogues of naturally occurring molecules DNA or RNA, leading to interruption in synthesis of DNA, RNA, or required for DNA and RNA synthesis. When substituted for the natural body proteins. substances, they disrupt DNA and RNA synthesis. bendamustine (nitrogen mustard) azacitidine (pyrimidine analogue) busulfan (alkyl sulfonate) capecitabine (pyrimidine analogue) carboplatin (platinum) cladribine (adenosine analogue) carmustine (nitrosurea) cytarabine (pyrimidine analogue) chlorambucil (nitrogen mustard) fludarabine (purine analogue) cisplatin (platinum) fluorouracil (pyrimidine analogue) cyclophosphamide (nitrogen mustard) gemcitabine (pyrimidine analogue) dacarbazine (triazine) mercaptopurine (purine analogue) estramustine (nitrogen mustard with 17-beta-estradiol) methotrexate (folate analogue) hydroxyurea pralatrexate (folate analogue) ifosfamide (nitrogen mustard) pemetrexed (folate analogue) lomustine (nitrosurea) pentostatin (purine analogue) mechlorethamine (nitrogen mustard) raltitrexed (folate analogue) melphalan (nitrogen mustard) thioguanine (purine analogue) oxaliplatin (platinum) trifluridine-tipiracil (pyrimidine analogue/thymidine phosphorylase procarbazine (triazine) inhibitor) -

I4X-JE-JFCM an Open-Label, Multicenter, Phase 1B/2 Study To
Protocol (e) I4X-JE-JFCM An Open-label, Multicenter, Phase 1b/2 Study to Evaluate Necitumumab in Combination with Gemcitabine and Cisplatin in the First-Line Treatment of Patients with Advanced (Stage IV) Squamous Non-Small Cell Lung Cancer (NSCLC) NCT01763788 Approval Date: 12-Jun-2016 I4X-JE-JFCM(e) Clinical Protocol Page 1 1. Protocol I4X-JE-JFCM(e) An Open-label, Multicenter, Phase 1b/2 Study to Evaluate Necitumumab in Combination with Gemcitabine and Cisplatin in the First-Line Treatment of Patients with Advanced (Stage IV) Squamous Non-Small Cell Lung Cancer (NSCLC) Confidential Information The information contained in this protocol is confidential and is intended for the use of clinical investigators. It is the property of Eli Lilly and Company or its subsidiaries and should not be copied by or distributed to persons not involved in the clinical investigation of Necitumumab (IMC-11F8; LY3012211), unless such persons are bound by a confidentiality agreement with Eli Lilly and Company or its subsidiaries. Note to Regulatory Authorities: This document may contain protected personal data and/or commercially confidential information exempt from public disclosure. Eli Lilly and Company requests consultation regarding release/redaction prior to any public release. In the United States, this document is subject to Freedom of Information Act (FOIA) Exemption 4 and may not be reproduced or otherwise disseminated without the written approval of Eli Lilly and Company or its subsidiaries. Necitumumab (IMC-11F8; LY3012211) Gemcitabine (LY188011) This is a Phase 1b/2 study in the first-line treatment of patients with advanced (Stage IV) Squamous Non-Small Cell Lung Cancer (NSCLC). -
Targeting the Epidermal Growth Factor Receptor in EGFR-Mutated Lung Cancer: Current and Emerging Therapies
cancers Review Targeting the Epidermal Growth Factor Receptor in EGFR-Mutated Lung Cancer: Current and Emerging Therapies Karam Khaddour 1,*, Sushma Jonna 1, Alexander Deneka 2 , Jyoti D. Patel 3, Mohamed E. Abazeed 4, Erica Golemis 2 , Hossein Borghaei 5 and Yanis Boumber 3,6,* 1 Division of Hematology and Oncology, University of Illinois at Chicago, Chicago, IL 60612, USA; [email protected] 2 Fox Chase Cancer Center, Program in Molecular Therapeutics, Philadelphia, PA 19111, USA; [email protected] (A.D.); [email protected] (E.G.) 3 Robert H. Lurie Comprehensive Cancer Center, Division of Hematology/Oncology, Feinberg School of Medicine, Northwestern University, Chicago, IL 60611, USA; [email protected] 4 Robert H. Lurie Comprehensive Cancer Center, Department of Radiation Oncology, Feinberg School of Medicine, Northwestern University, Chicago, IL 60611, USA; [email protected] 5 Fox Chase Cancer Center, Department of Hematology and Oncology, Philadelphia, PA 19111, USA; [email protected] 6 Institute of Fundamental Medicine and Biology, Kazan Federal University, 420008 Kazan, Russia * Correspondence: [email protected] (K.K.); [email protected] (Y.B.) Simple Summary: Epidermal growth factor receptor (EGFR) mutations occur in a significant number Citation: Khaddour, K.; Jonna, S.; of lung cancer patients. Treatment outcomes in this subset of patients has greatly improved over the Deneka, A.; Patel, J.D.; Abazeed, M.E.; last decade after the introduction of EGFR tyrosine kinase inhibitors (TKIs), which demonstrated high Golemis, E.; Borghaei, H.; Boumber, Y. efficacy and improved survival in randomized clinical trials. Although EGFR TKIs became the stan- Targeting the Epidermal Growth dard of care in patients with EGFR-mutated lung cancer, resistance almost inevitably develops. -

Advances in Epidermal Growth Factor Receptor Specific Immunotherapy: Lessons to Be Learned from Armed Antibodies
www.oncotarget.com Oncotarget, 2020, Vol. 11, (No. 38), pp: 3531-3557 Review Advances in epidermal growth factor receptor specific immunotherapy: lessons to be learned from armed antibodies Fleury Augustin Nsole Biteghe1,*, Neelakshi Mungra2,*, Nyangone Ekome Toung Chalomie4, Jean De La Croix Ndong5, Jean Engohang-Ndong6, Guillaume Vignaux7, Eden Padayachee8, Krupa Naran2,* and Stefan Barth2,3,* 1Department of Radiation Oncology and Biomedical Sciences, Cedars-Sinai Medical, Los Angeles, CA, USA 2Medical Biotechnology & Immunotherapy Research Unit, Institute of Infectious Disease and Molecular Medicine, Faculty of Health Sciences, University of Cape Town, Cape Town, South Africa 3South African Research Chair in Cancer Biotechnology, Department of Integrative Biomedical Sciences, Faculty of Health Sciences, University of Cape Town, Cape Town, South Africa 4Sun Yat-Sen University, Zhongshan Medical School, Guangzhou, China 5Department of Orthopedic Surgery, New York University School of Medicine, New York, NY, USA 6Department of Biological Sciences, Kent State University at Tuscarawas, New Philadelphia, OH, USA 7Arctic Slope Regional Corporation Federal, Beltsville, MD, USA 8Department of Physiology, University of Kentucky, Lexington, KY, USA *These authors contributed equally to this work Correspondence to: Stefan Barth, email: [email protected] Keywords: epidermal growth factor receptor (EGFR); recombinant immunotoxins (ITs); targeted human cytolytic fusion proteins (hCFPs); recombinant antibody-drug conjugates (rADCs); recombinant antibody photoimmunoconjugates (rAPCs) Received: May 30, 2020 Accepted: August 11, 2020 Published: September 22, 2020 Copyright: © 2020 Biteghe et al. This is an open access article distributed under the terms of the Creative Commons Attribution License (CC BY 3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. -

Primary and Acquired Resistance to Immunotherapy in Lung Cancer: Unveiling the Mechanisms Underlying of Immune Checkpoint Blockade Therapy
cancers Review Primary and Acquired Resistance to Immunotherapy in Lung Cancer: Unveiling the Mechanisms Underlying of Immune Checkpoint Blockade Therapy Laura Boyero 1 , Amparo Sánchez-Gastaldo 2, Miriam Alonso 2, 1 1,2,3, , 1,2, , José Francisco Noguera-Uclés , Sonia Molina-Pinelo * y and Reyes Bernabé-Caro * y 1 Institute of Biomedicine of Seville (IBiS) (HUVR, CSIC, Universidad de Sevilla), 41013 Seville, Spain; [email protected] (L.B.); [email protected] (J.F.N.-U.) 2 Medical Oncology Department, Hospital Universitario Virgen del Rocio, 41013 Seville, Spain; [email protected] (A.S.-G.); [email protected] (M.A.) 3 Centro de Investigación Biomédica en Red de Cáncer (CIBERONC), 28029 Madrid, Spain * Correspondence: [email protected] (S.M.-P.); [email protected] (R.B.-C.) These authors contributed equally to this work. y Received: 16 November 2020; Accepted: 9 December 2020; Published: 11 December 2020 Simple Summary: Immuno-oncology has redefined the treatment of lung cancer, with the ultimate goal being the reactivation of the anti-tumor immune response. This has led to the development of several therapeutic strategies focused in this direction. However, a high percentage of lung cancer patients do not respond to these therapies or their responses are transient. Here, we summarized the impact of immunotherapy on lung cancer patients in the latest clinical trials conducted on this disease. As well as the mechanisms of primary and acquired resistance to immunotherapy in this disease. Abstract: After several decades without maintained responses or long-term survival of patients with lung cancer, novel therapies have emerged as a hopeful milestone in this research field. -

CDER Breakthrough Therapy Designation Approvals Data As of December 31, 2020 Total of 190 Approvals
CDER Breakthrough Therapy Designation Approvals Data as of December 31, 2020 Total of 190 Approvals Submission Application Type and Proprietary Approval Use Number Number Name Established Name Applicant Date Treatment of patients with previously BLA 125486 ORIGINAL-1 GAZYVA OBINUTUZUMAB GENENTECH INC 01-Nov-2013 untreated chronic lymphocytic leukemia in combination with chlorambucil Treatment of patients with mantle cell NDA 205552 ORIGINAL-1 IMBRUVICA IBRUTINIB PHARMACYCLICS LLC 13-Nov-2013 lymphoma (MCL) Treatment of chronic hepatitis C NDA 204671 ORIGINAL-1 SOVALDI SOFOSBUVIR GILEAD SCIENCES INC 06-Dec-2013 infection Treatment of cystic fibrosis patients age VERTEX PHARMACEUTICALS NDA 203188 SUPPLEMENT-4 KALYDECO IVACAFTOR 21-Feb-2014 6 years and older who have mutations INC in the CFTR gene Treatment of previously untreated NOVARTIS patients with chronic lymphocytic BLA 125326 SUPPLEMENT-60 ARZERRA OFATUMUMAB PHARMACEUTICALS 17-Apr-2014 leukemia (CLL) for whom fludarabine- CORPORATION based therapy is considered inappropriate Treatment of patients with anaplastic NOVARTIS lymphoma kinase (ALK)-positive NDA 205755 ORIGINAL-1 ZYKADIA CERITINIB 29-Apr-2014 PHARMACEUTICALS CORP metastatic non-small cell lung cancer (NSCLC) who have progressed on or are intolerant to crizotinib Treatment of relapsed chronic lymphocytic leukemia (CLL), in combination with rituximab, in patients NDA 206545 ORIGINAL-1 ZYDELIG IDELALISIB GILEAD SCIENCES INC 23-Jul-2014 for whom rituximab alone would be considered appropriate therapy due to other co-morbidities -

The Two Tontti Tudiul Lui Hi Ha Unit
THETWO TONTTI USTUDIUL 20170267753A1 LUI HI HA UNIT ( 19) United States (12 ) Patent Application Publication (10 ) Pub. No. : US 2017 /0267753 A1 Ehrenpreis (43 ) Pub . Date : Sep . 21 , 2017 ( 54 ) COMBINATION THERAPY FOR (52 ) U .S . CI. CO - ADMINISTRATION OF MONOCLONAL CPC .. .. CO7K 16 / 241 ( 2013 .01 ) ; A61K 39 / 3955 ANTIBODIES ( 2013 .01 ) ; A61K 31 /4706 ( 2013 .01 ) ; A61K 31 / 165 ( 2013 .01 ) ; CO7K 2317 /21 (2013 . 01 ) ; (71 ) Applicant: Eli D Ehrenpreis , Skokie , IL (US ) CO7K 2317/ 24 ( 2013. 01 ) ; A61K 2039/ 505 ( 2013 .01 ) (72 ) Inventor : Eli D Ehrenpreis, Skokie , IL (US ) (57 ) ABSTRACT Disclosed are methods for enhancing the efficacy of mono (21 ) Appl. No. : 15 /605 ,212 clonal antibody therapy , which entails co - administering a therapeutic monoclonal antibody , or a functional fragment (22 ) Filed : May 25 , 2017 thereof, and an effective amount of colchicine or hydroxy chloroquine , or a combination thereof, to a patient in need Related U . S . Application Data thereof . Also disclosed are methods of prolonging or increasing the time a monoclonal antibody remains in the (63 ) Continuation - in - part of application No . 14 / 947 , 193 , circulation of a patient, which entails co - administering a filed on Nov. 20 , 2015 . therapeutic monoclonal antibody , or a functional fragment ( 60 ) Provisional application No . 62/ 082, 682 , filed on Nov . of the monoclonal antibody , and an effective amount of 21 , 2014 . colchicine or hydroxychloroquine , or a combination thereof, to a patient in need thereof, wherein the time themonoclonal antibody remains in the circulation ( e . g . , blood serum ) of the Publication Classification patient is increased relative to the same regimen of admin (51 ) Int . -

Necitumumab: a New Therapeutic Option for Squamous Cell Lung Cancer?
Editorial Necitumumab: a new therapeutic option for squamous cell lung cancer? Rathi N. Pillai, Suresh S. Ramalingam Winship Cancer Institute, Emory University, Atlanta, GA, USA Correspondence to: Suresh S. Ramalingam. Professor, Director of Medical Oncology, 1365 Clifton Road NE, Rm C-3090, Atlanta, GA 30322, USA. Email: [email protected]. Submitted Oct 03, 2014. Accepted for publication Oct 08, 2014. doi: 10.3978/j.issn.2218-6751.2014.11.01 View this article at: http://dx.doi.org/10.3978/j.issn.2218-6751.2014.11.01 Squamous cell carcinoma (SqCC) accounts for 25% Society of Clinical Oncology (ASCO) this year. This is the to 30% of all non-small lung carcinoma (NSCLC) largest study to date for patients with SqCC of the lung (3). diagnosed worldwide. Therapeutic advances for squamous A total of 1,093 patients with metastatic SqCC of the lung cell lung carcinoma have remained stagnant. This is in were randomized to treatment with gemcitabine/cisplatin stark comparison to adenocarcinoma of the lung, which combination given with or without necitumumab 800 mg has benefited from the development of therapies such intravenously on days 1 and 8 of a 21-day cycle. Patients as bevacizumab and pemetrexed, as well as targeted could receive up to six cycles of combination therapy therapies for specific molecular subsets with epidermal and then continue on maintenance necitumumab if they growth factor receptor (EGFR) mutations and anaplastic achieved clinical benefit. The primary endpoint was overall lymphoma kinase (ALK) rearrangements. Recent genomic survival (OS), with a pre-planned exploratory endpoint of characterization of SqCC by The Cancer Genome Atlas the use of EGFR protein expression as measured by H-score has identified mutations/amplifications in receptor tyrosine as a predictive biomarker. -

Approval Makes Olaratumab the First First-Line Treatment Option for Soft
Community Translations Edited by Jame Abraham, MD, FACP Approval makes olaratumab the first first-line treatment option for soft tissue sarcoma in more than 40 years hen the US Food and Drug Administration approved olaratumab as a first-line treatment What’s new, what’s important for patients with soft tissue sarcoma (STS) in The approval of olaratumab as a first-line therapy for soft tis- the fall of 2016, it marked the first approval since the che- sue sarcoma was based on data from a phase 2 trial in which W 133 patients received olaratumab+doxorubicin or doxorubicin motherapy drug doxorubicin became standard of care more than 40 years ago.1 Though rare, STS, which comprises a alone. Median PFS was increased by 6.6 months in the study host of different histologic subtypes, has proven difficult group and 4.1 months in controls; improved ORR and OS were to treat. Like pazopanib, which was approved in 2012 for significant with olaratumab. The most common olaratumab-asso- the treatment of STS in the second-line setting, olara- ciated AEs include nausea, fatigue, and neutropenia, with more tumab targets the platelet-derived growth factor receptor grade 3/4 AEs in the olaratumab patients than controls. The alpha (PDGFRα), a tyrosine kinase receptor involved in recommended is dose 15 mg/kg as an IV infusion on days 1 cell signaling pathways that promotes key hallmark abili- and 8 of each 21-day cycle, with doxorubicin for the first 8 ties in both cancer cells and the cells of the tumor microen- cycles. -

Your Pharmacy Benefits Welcome to Your Pharmacy Plan
Your Pharmacy Benefits Welcome to Your Pharmacy Plan OptumRx manages your pharmacy benefits for your health plan sponsor. We look forward to helping you make informed decisions about medicines for you and your family. Please review this information to better understand your pharmacy benefit plan. Using Your Member ID Card You can use your pharmacy benefit ID card at any pharmacy participating in your plan’s pharmacy network. Show your ID card each time you fill a prescription at a network pharmacy. They will enter your card information and automatically file it with OptumRx. Your pharmacy will then collect your share of the payment. Your Pharmacy Network Your plan’s pharmacy network includes more than 67,000 independent and chain retail pharmacies nationwide. To find a network pharmacy near you, use the Locate a Pharmacy tool at www.optumrx.com. Or call Customer Service at 1-877-559-2955. Using Non -Network Pharmacies If you do not show the pharmacy your member ID card, or you fill a prescription at a non-network pharmacy, you must pay 100 percent of the pharmacy’s price for the drug. If the drug is covered by your plan, you can be reimbursed. To be reimbursed for eligible prescriptions, simply fill out and send a Direct Member Reimbursement Form with the pharmacy receipt(s) to OptumRx. Reimbursement amounts are based on contracted pharmacy rates minus your copayment or coinsurance. For a copy of the form, go to www.optumrx.com. Or call the Customer Service number above. The number is also on the back of your ID card. -

Anti-EGFR Antibody 528 Binds to Domain III of EGFR at a Site
www.nature.com/scientificreports OPEN Anti‑EGFR antibody 528 binds to domain III of EGFR at a site shifted from the cetuximab epitope Koki Makabe1, Takeshi Yokoyama2,3, Shiro Uehara2, Tomomi Uchikubo‑Kamo3, Mikako Shirouzu3, Kouki Kimura4, Kouhei Tsumoto5,6, Ryutaro Asano4, Yoshikazu Tanaka2 & Izumi Kumagai4* Antibodies have been widely used for cancer therapy owing to their ability to distinguish cancer cells by recognizing cancer‑specifc antigens. Epidermal growth factor receptor (EGFR) is a promising target for the cancer therapeutics, against which several antibody clones have been developed and brought into therapeutic use. Another antibody clone, 528, is an antagonistic anti‑EGFR antibody, which has been the focus of our antibody engineering studies to develop cancer drugs. In this study, we explored the interaction of 528 with the extracellular region of EGFR (sEGFR) via binding analyses and structural studies. Dot blotting experiments with heat treated sEGFR and surface plasmon resonance binding experiments revealed that 528 recognizes the tertiary structure of sEGFR and exhibits competitive binding to sEGFR with EGF and cetuximab. Single particle analysis of the sEGFR–528 Fab complex via electron microscopy clearly showed the binding of 528 to domain III of sEGFR, the domain to which EGF and cetuximab bind, explaining its antagonistic activity. Comparison between the two‑ dimensional class average and the cetuximab/sEGFR crystal structure revealed that 528 binds to a site that is shifted from, rather than identical to, the cetuximab epitope, and may exclude known drug‑ resistant EGFR mutations. Epidermal growth factor receptor (EGFR) is a member of the closely related family of ErbB transmembrane protein tyrosine kinase receptors. -
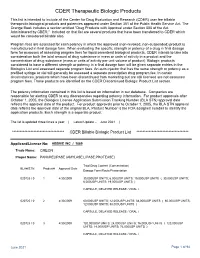
CDER Therapeutic Biologic Products List
CDER Therapeutic Biologic Products This list is intended to include all the Center for Drug Evaluation and Research (CDER) user fee billable therapeutic biological products and potencies approved under Section 351 of the Public Health Service Act. The Orange Book includes a section entitled "Drug Products with Approval under Section 505 of the Act Administered by CBER." Included on that list are several products that have been transferred to CDER which would be considered billable also. Program fees are assessed for each potency in which the approved (non-revoked, non-suspended) product is manufactured in final dosage form. When evaluating the specific strength or potency of a drug in final dosage form for purposes of assessing program fees for liquid parenteral biological products, CDER intends to take into consideration both the total amount of drug substance in mass or units of activity in a product and the concentration of drug substance (mass or units of activity per unit volume of product). Biologic products considered to have a different strength or potency in a final dosage form will be given separate entries in the Biologics List and assessed separate program fees. An auto-injector that has the same strength or potency as a prefilled syringe or vial will generally be assessed a separate prescription drug program fee. In certain circumstances, products which have been discontinued from marketing but are still licensed are not assessed program fees. Those products are identified on the CDER Discontinued Biologic Product List section. The potency information contained in this list is based on information in our database.