Nitrous Oxide: Pharmacology, Signs/Symptoms, Patient Selection
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fact Sheet on Methadone
Fact Sheet: Methadone Common Questions about Methadone • What is the typical dose of methadone and how is it taken? • How does someone know methadone is working? • How long does a person take methadone? • Who can prescribe methadone? • Can a person overdose on methadone? What is the typical dose of methadone and how is it taken? • Due to methadone’s slow and steady activation of opioid receptors, a person requires only one methadone dose per day. • Every person is different, and dosing should be individualized, based on a person’s experience of a reduction of withdrawal symptoms and cravings. • Most people start with an initial dose of 30-35 mg. It is then increased by 5mg every 3 days until a person experiences a relief from withdrawal symptoms.1 • Methadone is taken by mouth in a liquid form. • The recommended therapeutic (i.e., effective) dose of methadone is between 60 and 120 mg.1 How does someone know methadone is working? • The person will stop feeling withdrawal symptoms. • The person will also experience fewer cravings to use opioids. The intensity of their cravings will go down, but they may not completely go away.1 o Someone taking methadone may still have cravings to use other substances such as cocaine, benzodiazepines, alcohol, etc. The 3 Dimensions of Cravings: Frequency Duration Severity Number of separate times Once a craving starts, it Cravings range in a person starts to can range in how long it intensity, such as how experience a craving lasts at a high, distracting overwhelming, distracting, during the day. level. This could be and painful they feel. -

Methadone Hydrochloride Tablets, USP) 5 Mg, 10 Mg Rx Only
ROXANE LABORATORIES, INC. Columbus, OH 43216 DOLOPHINE® HYDROCHLORIDE CII (Methadone Hydrochloride Tablets, USP) 5 mg, 10 mg Rx Only Deaths, cardiac and respiratory, have been reported during initiation and conversion of pain patients to methadone treatment from treatment with other opioid agonists. It is critical to understand the pharmacokinetics of methadone when converting patients from other opioids (see DOSAGE AND ADMINISTRATION). Particular vigilance is necessary during treatment initiation, during conversion from one opioid to another, and during dose titration. Respiratory depression is the chief hazard associated with methadone hydrochloride administration. Methadone's peak respiratory depressant effects typically occur later, and persist longer than its peak analgesic effects, particularly in the early dosing period. These characteristics can contribute to cases of iatrogenic overdose, particularly during treatment initiation and dose titration. In addition, cases of QT interval prolongation and serious arrhythmia (torsades de pointes) have been observed during treatment with methadone. Most cases involve patients being treated for pain with large, multiple daily doses of methadone, although cases have been reported in patients receiving doses commonly used for maintenance treatment of opioid addiction. Methadone treatment for analgesic therapy in patients with acute or chronic pain should only be initiated if the potential analgesic or palliative care benefit of treatment with methadone is considered and outweighs the risks. Conditions For Distribution And Use Of Methadone Products For The Treatment Of Opioid Addiction Code of Federal Regulations, Title 42, Sec 8 Methadone products when used for the treatment of opioid addiction in detoxification or maintenance programs, shall be dispensed only by opioid treatment programs (and agencies, practitioners or institutions by formal agreement with the program sponsor) certified by the Substance Abuse and Mental Health Services Administration and approved by the designated state authority. -

Tramadol (Ultram)
TRAMADOL (ULTRAM) Tramadol is FDA approved for the treatment of musculoskeletal pain. Studies have shown it is useful in treating the pain associated with diabetic neuropathy and other pain conditions. Tramadol comes in 50 mg tablets. The maximum dose is two tablets four times per day unless your kidney function is below normal or you are over 75 years old, in which case the maximum dose is two tablets three times per day. The main side effects of Tramadol are drowsiness, sedation, and stomach upset, all of which are minimized by slowly raising the dose. About 5% of patients have stomach upset at any dose of Tramadol and cannot take the medicine. Other risks include seizures (occur in less than 1/100,000 and are more likely if you have seizures) and possibly abuse (relevant if you have abused drugs in the past). Tramadol should be started at a low dose and raise the dose slowly toward the maximum dose. Start with one tablet at bedtime. After 3 - 7 days, increase to one tablet twice daily (morning and bedtime). After an additional 3 - 7 days, increase to one tablet three times per day (morning, noon, and bedtime). After an additional 3 - 7 days, increase to one tablet four times per day (1 tablet with each meal and 1 at bedtime). At that point, the dose may be increased or adjusted depending on how you are doing. To increase further, you will: Add a second tablet at bedtime (one tablet three times per day and two tablets at bedtime). After 3 - 7 days, add a second tablet to another dose (one tablet twice per day and two tablets twice per day). -

Effects of Prophylactic Ketamine and Pethidine to Control Postanesthetic Shivering: a Comparative Study
Biomedical Research and Therapy, 5(12):2898-2903 Original Research Effects of prophylactic ketamine and pethidine to control postanesthetic shivering: A comparative study Masoum Khoshfetrat1, Ali Rosom Jalali2, Gholamreza Komeili3, Aliakbar Keykha4;∗ ABSTRACT Background: Shivering is an undesirable complication following general anesthesia and spinal anesthesia, whose early control can reduce postoperative metabolic and respiratory complications. Therefore, this study aims to compare the effects of prophylactic injection of ketamine and pethi- dine on postoperative shivering.Methods: This double-blind clinical trial was performed on 105 patients with short-term orthopedic and ENT surgery. The patients were randomly divided into three groups; 20 minutes before the end of the surgery, 0.4 mg/kg of pethidine was injected to the first group, 0.5 mg/kg of ketamine was injected to the second group, and normal saline was injected to the third group. After the surgery, the tympanic membrane temperature was measured at 0, 10, 20, and 30 minutes. The shivering was also measured by a four-point grading from zero (no shiv- ering) to four (severe shivering). Data were analyzed by one-way ANOVA, Kruskal Wallis, Chi-square 1Doctor of Medicine (MD), Fellow of and Pearson correlation. Results: The mean age of patients was 35.811.45 years in the ketamine Critical Care Medicine (FCCM), group, 34.811.64 years in the normal saline group, and 33.1110.5 years in the pethidine group. Department of Anesthesiology and The one-way ANOVA showed no significant difference in the mean age between the three groups Critical Care, Khatam-Al-Anbiya (P=0.645). -

Current Awareness in Clinical Toxicology Editors: Damian Ballam Msc and Allister Vale MD
Current Awareness in Clinical Toxicology Editors: Damian Ballam MSc and Allister Vale MD February 2016 CONTENTS General Toxicology 9 Metals 38 Management 21 Pesticides 41 Drugs 23 Chemical Warfare 42 Chemical Incidents & 32 Plants 43 Pollution Chemicals 33 Animals 43 CURRENT AWARENESS PAPERS OF THE MONTH How toxic is ibogaine? Litjens RPW, Brunt TM. Clin Toxicol 2016; online early: doi: 10.3109/15563650.2016.1138226: Context Ibogaine is a psychoactive indole alkaloid found in the African rainforest shrub Tabernanthe Iboga. It is unlicensed but used in the treatment of drug and alcohol addiction. However, reports of ibogaine's toxicity are cause for concern. Objectives To review ibogaine's pharmacokinetics and pharmacodynamics, mechanisms of action and reported toxicity. Methods A search of the literature available on PubMed was done, using the keywords "ibogaine" and "noribogaine". The search criteria were "mechanism of action", "pharmacokinetics", "pharmacodynamics", "neurotransmitters", "toxicology", "toxicity", "cardiac", "neurotoxic", "human data", "animal data", "addiction", "anti-addictive", "withdrawal", "death" and "fatalities". The searches identified 382 unique references, of which 156 involved human data. Further research revealed 14 detailed toxicological case reports. Current Awareness in Clinical Toxicology is produced monthly for the American Academy of Clinical Toxicology by the Birmingham Unit of the UK National Poisons Information Service, with contributions from the Cardiff, Edinburgh, and Newcastle Units. The NPIS is commissioned by Public Health England Current Awareness in Clinical Toxicology Editors: Damian Ballam MSc and Allister Vale MD February 2016 Current Awareness in Clinical Toxicology is produced monthly for the American Academy of Clinical Toxicology by the Birmingham Unit of the UK National Poisons Information Service, with contributions from the Cardiff, Edinburgh, and Newcastle Units. -

Isoflurane Produces Antidepressant Effects and Induces Trkb Signaling in Rodents
bioRxiv preprint doi: https://doi.org/10.1101/084525; this version posted July 11, 2017. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Isoflurane produces antidepressant effects and induces TrkB signaling in rodents Hanna Antilaa, Maria Ryazantsevaa,b, Dina Popovaa, Pia Sipiläa, Ramon Guiradoa, Samuel Kohtalaa,b, Ipek Yalcinc, Jesse Lindholma, Liisa Vesaa, Vinicius Satod, Joshua Cordeirae, Henri Autioa, Mikhail Kislina, Maribel Riose, Sâmia Jocad, Plinio Casarottoa, Leonard Khirouga, Sari Lauria,b, Tomi Tairaa,f, Eero Castréna* and Tomi Rantamäkia,b* aNeuroscience Center, P.O. Box 56, FI-00014 University of Helsinki, Helsinki, Finland. bDivision of Physiology and Neuroscience, Department of Biosciences, Faculty of Biological and Environmental Sciences, P.O. Box 66, FI-00014 University of Helsinki, Helsinki, Finland. cInstitut des Neurosciences Cellulaires et Intégratives, Centre National de la Recherche Scientifique, FR-67084 Strasbourg Cedex, France. dSchool of Pharmaceutical Sciences of Ribeirão Preto 14040-903, Brazil. eTufts University, Boston, MA, USA. fDepartment of Veterinary Biosciences, Faculty of Veterinary Medicine P.O. Box 66, FI-00014 University of Helsinki, Helsinki, Finland. *To whom correspondence should be addressed at: Eero Castrén ([email protected]) or Tomi Rantamäki ([email protected]) A brief burst-suppressing isoflurane anesthesia has been shown to rapidly alleviate symptoms of depression in a subset of patients, but the neurobiological basis of these observations remains obscure. We show that a single isoflurane anesthesia produces antidepressant-like behavioural effects in the learned helplessness paradigm and regulates molecular events implicated in the mechanism of action of rapid-acting antidepressant ketamine: activation of brain-derived neurotrophic factor (BDNF) receptor TrkB, facilitation of mammalian target of rapamycin (mTOR) signaling pathway and inhibition of glycogen synthase kinase 3β (GSK3β). -
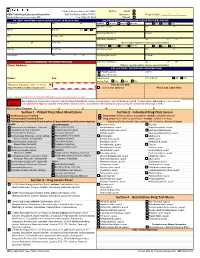
Quantitative Drug Test Menu Section 2
1 Guthrie Square, Sayre, PA 18840 Bill To: Client GMG Toxicology Laboratory Requisition Toll Free Phone (844) 617-4719 Insurance Request Date: _____/______/______ Medical Director: Hani Hojjati, MD Fax (570) 887-4729 Patient PATIENT INFORMATION (PLEASE PRINT IN BLACK INK) INSURANCE BILLING INFORMATION (PLEASE PRINT IN BLACK INK) Pt Last Name First M I PRIMARY Medicare Medicaid Other Ins. Self Spouse Child __ Subscriber Last Name First M Address Birth Date Sex M F Beneficiary/Member # Group # City Pt. SS# or MRN Claims Name and Address City ST ZIP ST ZIP Home Phone (Attach a copy of the patient's insurance card and information) SECONDARY Medicare Medicaid Other Ins. Self Spouse Child Employer Work Phone Subscriber Last Name First M Work Address City ST ZIP Beneficiary/Member # Group # __ CLIENT INFORMATION - REFERRING PHYSICIAN Claims Name and Address City ST ZIP Client Address: (Atttach a copy of the patient's insurance card and information) COLLECTION / REPORTING INFORMATION Copy to: FAX Results to __ CALL Results to Phone: Fax: Date Collected: Time Collected: AM PM Specimen Type: Urine Saliva Other ___________________ Physician Signature (legible - No Stamp) For Lab Use Only (Required for Medicare & Medicaid patient orders) Signed ABN Obtained Place Lab Label Here Contact Laboratory Medical Director (570-887-4719) with questions concerning medical necessity PHYSICIAN When ordering tests, the physician is required to make an independent medical necessity decision with regard to each test thelaboratory will bill. The physician also understands he or she is required NOTICE to (1) submit ICD-10 diagnosis supported in the patient's medical record as documentation of the medical necessity or (2) explain and have the patient sign an ABN. -

Guidelines for Ketamine Use
St Joseph's Mercy Hospice Auckland NZ Guidelines for Ketamine Use Ketamine is a dissociative anaesthetic agent which has analgesic properties in sub- anaesthetic doses 1 Its principal site of action is in the dorsal horn of the spinal cord where it blocks the N-methyl D-aspartate (NMDA) receptor complex. Ketamine is used in palliative care settings primarily for neuropathic pain which is unresponsive or poorly responsive to first-line analgesics (which may include one or more of opioid drug, NSAID, tricyclic antidepressant, or anticonvusant) It has also been used for phantom limb and ischaemic pain and for intractable incident pain or prior to procedures such as dressing changes. Potential side effects Ketamine Routine use of ketamine is limited by its cost and potential side effects which may occur in up to 40% of patients; These may include: Psychotomimetic phenomena – “feeling strange” - dysphoria, vivid dreams, nightmares, hallucinations, altered body image. These effects may be minimised or treated by concurrent use of haloperidol or a benzodiazepine Delirium Hypertension, tachycardia Diplopia, nystagmus Erythema and pain at injection site Contraindications to ketamine use Ketamine has the potential to increase intra-cranial and intra-ocular pressures. It is contraindicated in patients with a history of hypertension, cerebrovascular disease or epilepsy and should be used with caution in patients with raised intra-cranial pressure and/or known cerebral metastases. Dosage regimens for Ketamine use 1. “Burst ketamine” 2 Ketamine is prescribed as a ‘burst’or ‘pulse’ course for a maximum of 5 days. The dose is titrated up, in a stepwise fashion, and once the lowest effective dose is achieved it is continued for 3 days at that dose then stopped. -

Methadone and the Anti-Medication Bias in Addiction Treatment
White, W. & Coon, B. (2003). Methadone and the anti-medication bias in addiction treatment. Counselor 4(5): 58-63. Methadone and the Anti-medication Bias in Addiction Treatment William L. White, MA and Brian F. Coon, MA, CADC An Introductory Note: This article is long overdue. Like many addiction counselors personally and professionally rooted in the therapeutic community and Minnesota model programs of the 1960s and 1970s, I exhibited a rabid animosity toward methadone and protected these beliefs in a shell of blissful ignorance. That began to change in the late 1970s when a new mentor, Dr. Ed Senay, gently suggested that the great passion I expressed on the subject of methadone seemed to be in inverse proportion to my knowledge about methadone. I hope this article will serve as a form of amends for that ignorance and arrogance. (WLW) There is a deeply entrenched anti-medication bias within the field of addiction treatment. This bias is historically rooted in the iatrogenic insults that have resulted from attempts to treat drug addiction with drugs. The most notorious of these professional practices includes: coaching alcoholics to substitute wine and beer for distilled spirits, treating alcoholism and morphine addiction with cocaine and cannabis, switching alcoholics from alcohol to morphine, failing repeatedly to find an alcoholism vaccine, employing aversive agents that linked alcohol or morphine to the experience of suffocation and treating alcoholism with drugs that later emerged as problems in their own right, e.g., barbiturates, amphetamines, tranquilizers, and LSD. A history of harm done in the name of good culturally and professionally imbedded a deep distrust of drugs in the treatment of alcohol and other drug addiction (White, 1998). -

(Methadone Hydrochloride Oral Concentrate USP) and Methadose
NDA 17-116/S-021 Page 3 Methadose™ Oral Concentrate (methadone hydrochloride oral concentrate USP) and Methadose™ Sugar-Free Oral Concentrate (methadone hydrochloride oral concentrate USP) dye-free, sugar-free, unflavored CII Rx only FOR ORAL USE ONLY Deaths have been reported during initiation of methadone treatment for opioid dependence. In some cases, drug interactions with other drugs, both licit and illicit, have been suspected. However, in other cases, deaths appear to have occurred due to the respiratory or cardiac effects of methadone and too-rapid titration without appreciation for the accumulation of methadone over time. It is critical to understand the pharmacokinetics of methadone and to exercise vigilance during treatment initiation and dose titration (see DOSAGE AND ADMINISTRATION). Patients must also be strongly cautioned against self- medicating with CNS depressants during initiation of methadone treatment. Respiratory depression is the chief hazard associated with methadone hydrochloride administration. Methadone's peak respiratory depressant effects typically occur later, and persist longer than its peak analgesic effects, particularly in the early dosing period. These characteristics can contribute to cases of iatrogenic overdose, particularly during treatment initiation and dose titration. Cases of QT interval prolongation and serious arrhythmia (torsades de pointes) have been observed during treatment with methadone. Most cases involve patients being treated for pain with large, multiple daily doses of methadone, NDA -

CAN YOU TAKE TRAMADOL with NEFOPAM Can You Take Tramadol with Nefopam
CAN YOU TAKE TRAMADOL WITH NEFOPAM can you take tramadol with nefopam tramadol 37 5 vs percocet 5 325 ultram tramadol pictures tramadol hcl tabs 50 mg tramadol 200 mg recreational drugs and heart can tramadol and percocet be mixed hbs robaxin tramadol interaction generic tramadol 319 immediate release how long tramadol stay in your urine does tramadol make you sleepy or awake tramadol acetaminophen\/codeine 120 12mg sol b tracert ex tramadol dosage for adults meloxicam/tramadol/amitriptyline/lidocaine/prilocaine apo tramadol high feeling on hydrocodone tramadol apteka internetowa olmed order tramadol/paracetamol from mexico tramadol quizlet flashcards microbiology tramadol has mu opioid agonist activity director jobs tramadol met ritalin sr strengths hur ta tramadol withdrawal in dogs tramadol te gebruiken bij tramadol dosis cachorros bulldog 2015 100mg tramadol 10mg hydrocodone images 100 tramadol termasuk jenis obat apa acyclovir side how to get rid of a tramadol high 200 ml tramadol withdrawal timeline drug interactions between percocet and tramadol comparison tramadol e morfina presentacion de tres can tramadol be taken with paracetamol indication and action tramadol review article template with photos tramadol codeine allergy rash best price tramadol online tramadol 93 58 dosage for ibuprofen tramadol v oxycodone pill colors can tramadol make you drowsy doll b tracert ex tramadol addiction withdrawal tramadol instant release oxycontin pictures can you drink wine with tramadol i can function tramadol hydrochloride sleepy tramadol cva -

Effects of in Vitro Amitriptyline, Fluoxetine, Tranylcypromine and Venlafaxine on Saphenous Vein Grafts
ORIGINAL ARTICLE Braz J Cardiovasc Surg 2019;34(3):290-6 Effects of in vitro Amitriptyline, Fluoxetine, Tranylcypromine and Venlafaxine on Saphenous Vein Grafts Melek Akinci1, MD; Cetin Hakan Karadag2, MD; Serhat Huseyin3, MD; Cagatay Oltulu4, MD; Suat Canbaz3, MD; Ozgur Gunduz2, MD; Ruhan Deniz Topuz2, MD DOI: 10.21470/1678-9741-2018-0338 Abstract Objective: In this study, we aimed to examine the effects of (Log M) was 74.6%, the response at -6.32 (Log M) was 75.5%. amitriptyline, fluoxetine, tranylcypromine and venlafaxine on While the relaxation response at -6.46 (Log M) of fluoxetine was saphenous vein grafts in coronary artery bypass graft surgeries. 68.02%, the response at -6.02 (Log M) was 72.12%. While the Methods: 59 patients (40 males and 19 females; mean age relaxation response of tranylcypromine at -7.53 (Log M) was 65.1 years, distribution: 45-84 years) who had coronary artery 61.13%, the response at -7.23 (Log M) was 65.53%. While the bypass graft surgery between February 2014 and May 2016 were relaxation response of venlafaxine at -6.21 (Log M) was 29.98%, included in the study. After the saphenous vein grafts with intact the response at -5.90 (Log M) was 32.96%. and denuded endothelium were precontracted with 3×10-6M Conclusion: The maximum relaxation at minimum and phenylephrine, amitriptyline, fluoxetine and tranylcypromine maximum therapeutic concentrations was obtained with were cumulatively added to isolated organ baths in the range of amitriptyline, fluoxetine and tranylcypromine, and the minimum 10-11-3x10-5M, while venlafaxine was added in the range of 10-9- relaxation was obtained with venlafaxine.