Thrombocytopenia in Virus Infections
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Picture of the Month
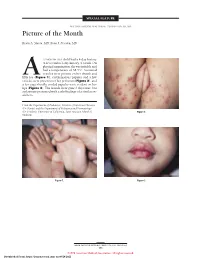
SPECIAL FEATURE SECTION EDITOR: WALTER W. TUNNESSEN, JR, MD Picture of the Month Kevin A. Slavin, MD; Ilona J. Frieden, MD 15-MONTH-OLD child had a 4-day history of fever and a 1-day history of a rash. On physical examination she was irritable and had a temperature of 38.3°C. Scattered vesicles were present on her thumb and Afifth toe (Figure 1), erythematous papules and a few vesicles were present over her perineum (Figure 2), and a few superficially eroded papules were evident on her lips (Figure 3). The lesions were gone 3 days later, but a playmate presented with early findings of a similar ex- anthem. From the Department of Pediatrics, Division of Infectious Diseases (Dr Slavin) and the Department of Pediatrics and Dermatology (Dr Frieden), University of California, San Francisco School of Figure 2. Medicine. Figure 1. Figure 3. ARCH PEDIATR ADOLESC MED/ VOL 152, MAY 1998 505 ©1998 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 09/28/2021 Denouement and Discussion Hand-Foot-and-Mouth Disease Figure 1. Vesicles are present on the thumb and fifth toe. foot-and-mouth disease).1,2,5-9 The lesions on the but- tocks are of the same size and typical of the early forms Figure 2. Multiple erythematous papules and a few scattered vesicles are of the exanthem, but they are not frequently vesicular present over the perineum. in nature. Lesions involving the perineum seem to be more Figure 3. Superficially eroded papules are present on the lips. common in children who wear diapers, suggesting that friction or minor trauma may play a role in the develop- ment of lesions. -

BLOOD INFECTIONS INTRODUCTION TYPES Of
BLOOD INFECTIONS Please supplement and learn theory on the basis of the lecture, Mim’s book and supplementary materials before class!!! INTRODUCTION PRINCIPLE: UNDER NATURAL CONDITIONS BLOOD IS STERILE IMPORTANT TERMS: Nosocomial infection ……………………………………………………………………………………………………………….. Bacteremia ………………………………………………………………………………………………………………………………. Viremia …………………………………………………………………………………………………………………………………….. Fungemia ………………………………………………………………………………………………………………………………….. Sepsis …………………………………………………………………………………………………………………………………………. SIRS …………………………………………………………………………………………………………………………………………….. MODS …………………………………………………………………………………………………………………………………………. ARDS …………………………………………………………………………………………………………………………………………… DIC ………………………………………………………………………………………………………………………………………………. CRBI …………………………………………………………………………………………………………………………………………….. BSI ………………………………………………………………………………………………………………………………………………. TYPES of BACTEREMIA .------------------------------------ ---------------------------------- ---------------------------------- •Examples: •Examples: •Examples: •-------------------------------------- •------------------------------------- •------------------------------------ -------------------------------------- •-------------------------------------- •-------------------------------------- -------------------------------------- -------------------------------------- -------------------------------------- -------------------------------------- -------------------------------------- -------------------------------------- -------------------------------------- -------------------------------------- -

Practice Advisory for the Prevention, Diagnosis, and Management of Infectious Complications Associated with Neuraxial Techniques
PRACTICE PARAMETER Practice Advisory for the Prevention, Diagnosis, and Management of Infectious Complications Associated with Neuraxial Techniques (ANESTHESIOLOGY 2017; XXX:00-00) An Updated Report by the American Society of Anesthesiologists Task Force on Infectious Complications Associated with Neuraxial Techniques and the American Society of Regional Anesthesia and Pain Medicine* RACTICE advisories are systematically developed Methodology reports that are intended to assist decision-making P Definition of Infectious Complications Associated with in areas of patient care. Advisories provide a synthesis of Neuraxial Techniques scientific literature and analysis of expert opinion, clini- For this Advisory, infectious complications are defined cal feasibility data, open forum commentary, and consen- as serious infections associated with the use of neuraxial sus surveys. Practice advisories developed by the American techniques. Neuraxial techniques include, but are not Society of Anesthesiologists (ASA) are not intended as standards, guidelines, or absolute requirements, and their limited to, epidural, spinal, or combined spinal-epidural use cannot guarantee any specific outcome. They may be administration of anesthetics, analgesics, or steroids; lum- adopted, modified, or rejected according to clinical needs bar puncture/spinal tap; epidural blood patch; epidural and constraints, and they are not intended to replace local lysis of adhesions; intrathecal chemotherapy; epidural or institutional policies. spinal injection of contrast agents -

Cytokine Serum Levels During Post-Transplant Adverse Events in 61 Pediatric Patients After Hematopoietic Stem Cell Transplantati
Döring et al. BMC Cancer (2015) 15:607 DOI 10.1186/s12885-015-1616-z RESEARCH ARTICLE Open Access Cytokine serum levels during post-transplant adverse events in 61 pediatric patients after hematopoietic stem cell transplantation Michaela Döring1*, Karin Melanie Cabanillas Stanchi1, Markus Mezger1, Annika Erbacher1, Judith Feucht1, Matthias Pfeiffer1, Peter Lang1, Rupert Handgretinger1 and Ingo Müller2 Abstract Background: Veno-occlusive disease, Graft-versus-Host disease, invasive or localized bacterial, viral and fungal infections are known as adverse events after hematopoietic stem cell transplantation representing the major cause for morbidity and mortality. Detection and differentiation of these adverse events are based on clinical symptoms and routine measurements of laboratory parameters. Methods: To identify the role of cytokines as a possible complication-marker for adverse events, 61 consecutive pediatric patients with a median age of 7.0 years who underwent hematopoietic stem cell transplantation were enrolled in this single-center retrospective study. Interleukin-1 beta (IL-1β), soluble interleukin-2 receptor (sIL-2R), interleukin-6 (IL-6), interleukin-8 (IL-8), interleukin-10 (IL-10) and tumor necrosis factor-α serum (TNF-α) levels were regularly assessed after transplantation and during transplantation related adverse events. Results: Veno-occlusive disease was accompanied by a significant increase in levels of IL-6, IL-8 and TNF-α.Graft- versus-Host disease was associated with a significant increase of IL-10, sIL-2R, IL-6 and TNF-α, depending on the respective stage or grade. Cytokine IL-6 enabled a significant differentiation between sepsis and fungemia, sepsis and viremia, and sepsis and bacteremia. Moreover, cytokine IL-8 enabled a significant differentiation between sepsis and viremia, sepsis and bacteremia, and bacteremia and viremia whereas IL-10 made a distinction between sepsis and viremia possible. -

Hand, Foot, and Mouth Disease (Coxsackievirus) Fact Sheet
Hand, Foot, and Mouth Disease (Coxsackievirus) Fact Sheet Hand, foot, and mouth disease is caused by one of several types of viruses Hand, foot, and mouth disease is usually characterized by tiny blisters on the inside of the mouth and the palms of the hands, fingers, soles of the feet. It is commonly caused by coxsackievirus A16 (an enterovirus), and less often by other types of viruses. Anyone can get hand, foot, and mouth disease Young children are primarily affected, but it may be seen in adults. Most cases occur in the summer and early fall. Outbreaks may occur among groups of children especially in child care centers or nursery schools. Symptoms usually appear 3 to 5 days after exposure. Hand, foot, and mouth disease is usually spread through person-to-person contact People can spread the disease when they are shedding the virus in their feces. It is also spread by the respiratory tract from mouth or respiratory secretions (such as from saliva on hands or toys). The virus has also been found in the fluid from the skin blisters. The infection is spread most easily during the acute phase/stage of illness when people are feeling ill, but the virus can be spread for several weeks after the onset of infection. The symptoms are much like a common cold with a rash The rash appears as blisters or ulcers in the mouth, on the inner cheeks, gums, sides of the tongue, and as bumps or blisters on the hands, feet, and sometimes other parts of the skin. The skin rash may last for 7 to 10 days. -

HIV-1 Tat Protein Mimicry of Chemokines
Proc. Natl. Acad. Sci. USA Vol. 95, pp. 13153–13158, October 1998 Immunology HIV-1 Tat protein mimicry of chemokines ADRIANA ALBINI*, SILVANO FERRINI*, ROBERTO BENELLI*, SABRINA SFORZINI*, DANIELA GIUNCIUGLIO*, MARIA GRAZIA ALUIGI*, AMANDA E. I. PROUDFOOT†,SAMI ALOUANI†,TIMOTHY N. C. WELLS†, GIULIANO MARIANI‡,RONALD L. RABIN§,JOSHUA M. FARBER§, AND DOUGLAS M. NOONAN*¶ *Centro di Biotecnologie Avanzate, Istituto Nazionale per la Ricerca sul Cancro, Largo Rosanna Benzi, 10, 16132 Genoa, Italy; †Geneva Biomedical Research Institute, Glaxo Wellcome Research and Development, 14 chemin des Aulx, 1228 Plan-les Ouates, Geneva, Switzerland; ‡Dipartimento di Medicina Interna, Medicina Nucleare, University of Genova, Viale Benedetto XV, 6, 16132 Genoa, Italy; and §National Institute of Allergy and Infectious Diseases, National Institutes of Health, Building 10, Room 11N228 MSC 1888, Bethesda, MD 20892 Edited by Anthony S. Fauci, National Institute of Allergy and Infectious Diseases, Bethesda, MD, and approved August 25, 1998 (received for review June 24, 1998) ABSTRACT The HIV-1 Tat protein is a potent chemoat- ceptors for some dual tropic HIV-1 strains (10, 11). A CCR2 tractant for monocytes. We observed that Tat shows conserved polymorphism has been found to correlate with delayed amino acids corresponding to critical sequences of the che- progression to AIDS (12, 13). mokines, a family of molecules known for their potent ability We report here that the HIV-1 Tat protein and the peptide to attract monocytes. Synthetic Tat and a peptide (CysL24–51) encompassing the cysteine-rich and core regions induce per- encompassing the ‘‘chemokine-like’’ region of Tat induced a tussis toxin sensitive Ca21 fluxes in monocytes. -

Malarial Pathocoenosis: Beneficial and Deleterious Interactions Between Malaria and Other Human Diseases Eric Faure
Malarial pathocoenosis: beneficial and deleterious interactions between malaria and other human diseases Eric Faure To cite this version: Eric Faure. Malarial pathocoenosis: beneficial and deleterious interactions between malaria and other human diseases. Frontiers in Physiology, Frontiers, 2014, 5 (441 ), 10.3389/fphys.2014.00441. hal- 01242005 HAL Id: hal-01242005 https://hal-amu.archives-ouvertes.fr/hal-01242005 Submitted on 11 Dec 2015 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. REVIEW ARTICLE published: 21 November 2014 doi: 10.3389/fphys.2014.00441 Malarial pathocoenosis: beneficial and deleterious interactions between malaria and other human diseases Eric Faure* Aix-Marseille Université, Centre National de la Recherche Scientifique, Centrale Marseille, I2M, UMR 7373, Marseille, France Edited by: In nature, organisms are commonly infected by an assemblage of different parasite Anaïs Baudot, Centre National de la species or by genetically distinct parasite strains that interact in complex ways. Linked Recherche Scientifique, France to co-infections, pathocoenosis, a term proposed by M. Grmek in 1969, refers to a Reviewed by: pathological state arising from the interactions of diseases within a population and to Satyaprakash Nayak, Pfizer Inc., USA the temporal and spatial dynamics of all of the diseases. -

A Guide to Clinical Management and Public Health Response for Hand, Foot and Mouth Disease (HFMD)
A Guide to Clinical Management and Public Health Response for Hand, Foot and Mouth Disease (HFMD) WHO Western Pacific Region PUBLICATION ISBN-13 978 92 9061 525 5 A Guide to Clinical Management and Public Health Response for Hand, Foot and Mouth Disease (HFMD) WHO Library Cataloguing in Publication Data A Guide to clinical management and public health response for hand, foot and mouth disease (HFMD) 1. Hand, foot and mouth disease – epidemiology. 2. Hand, foot and mouth disease – prevention and control. [ ii ] 3. Disease outbreaks. 4. Enterovirus A, Human. I. Regional Emerging Disease Intervention Center. ISBN 978 92 9061 525 5 (NLM Classification: WC 500) © World Health Organization 2011 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: [email protected]). For WHO Western Pacific Regional Publications, request for permission to reproduce should be addressed to the Publications Office, World Health Organization, Regional Office for the Western Pacific, P.O. Box 2932, 1000, Manila, Philippines, (fax: +632 521 1036, e-mail: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. -

Cytokine Modulators As Novel Therapies for Airway Disease
Copyright #ERS Journals Ltd 2001 Eur Respir J 2001; 18: Suppl. 34, 67s–77s European Respiratory Journal DOI: 10.1183/09031936.01.00229901 ISSN 0904-1850 Printed in UK – all rights reserved ISBN 1-904097-20-0 Cytokine modulators as novel therapies for airway disease P.J. Barnes Cytokine modulators as novel therapies for airway disease. P.J. Barnes. #ERS Correspondence: P.J. Barnes Journals Ltd 2001. Dept of Thoracic Medicine ABSTRACT: Cytokines play a critical role in orchestrating and perpetuating National Heart & Lung Institute inflammation in asthma and chronic obstructive pulmonary disease (COPD), and Imperial College Dovehouse Street several specific cytokine and chemokine inhibitors are now in development for the future London SW3 6LY therapy of these diseases. UK Anti-interleukin (IL)-5 is very effective at reducing peripheral blood and airway Fax: 0207 3515675 eosinophil numbers, but does not appear to be effective against symptomatic asthma. Inhibition of IL-4 with soluble IL-4 receptors has shown promising early results in Keywords: Chemokine receptor asthma. Inhibitory cytokines, such as IL-10, interferons and IL-12 are less promising, cytokine as systemic delivery causes side-effects. Inhibition of tumour necrosis factor-a may be interleukin-4 useful in severe asthma and for treating severe COPD with systemic features. interleukin-5 interleukin-9 Many chemokines are involved in the inflammatory response of asthma and COPD interleukin-10 and several low-molecular-weight inhibitors of chemokine receptors are in development. CCR3 antagonists (which block eosinophil chemotaxis) and CXCR2 antagonists (which Received: March 26 2001 block neutrophil and monocyte chemotaxis) are in clinical development for the Accepted April 25 2001 treatment of asthma and COPD respectively. -

Development of Megakaryoblastic Leukaemia in Runx1-Evi1 Knock-In Chimaeric Mouse
Letter to the Editor 1458 control. The Mcl-1-specific T-cell clone did not kill this cell line Ms. Bodil K. Jakobsen, Department of Clinical Immunology, (Figure 1c). University Hospital, Copenhagen, for HLA-typing of patient blood The lower rates of relapse in allogeneic transplantation samples. This study was supported by grants from the Danish compared with autologous bone marrow transplantation, the Medical Research Council, The Novo Nordisk Foundation, The striking clinical benefit of donor-lymphocyte infusions as well as Danish Cancer Society, The John and Birthe Meyer Foundation, the finding that human T cells can destroy chemotherapy- and Danish Cancer Research Foundation. resistant cell lines from chronic myeloid leukemia and multiple RB Sørensen1, OJ Nielsen2, P thor Straten1 and MH Andersen1 myeloma, have prompted development of immunotherapeutic 1 strategies against hematological cancers.3 Among these ap- Tumor Immunology Group, Institute of Cancer Biology, Danish Cancer Society, Copenhagen, Denmark and proaches, active specific immunization or vaccination is 2Department of Hematology, State University Hospital, emerging as a valuable tool to boost the adaptive immune Copenhagen, Denmark. system against malignant cells. In this regard, the identification E-mail: [email protected] of leukemia-associated antigens is crucial. However, very few antigens are characterized in a conceptual framework in which the biology, microenvironment, and conventional disease management have been taken into consideration. Myeloid cell References factor-1 (Mcl-1) is a death-inhibiting member of the Bcl-2 family that is expressed in early monocyte differentiation. Elevated 1 Andersen MH, Becker JC, thor Straten P. The anti-apoptotic member levels of Mcl-1 have been reported for a number of solid and of the Bcl-2 family Mcl-1 is a CTL target in cancer patients. -

CCR3, CCR5, Interleukin 4, and Interferon-Γ Expression on Synovial
CCR3, CCR5, Interleukin 4, and Interferon-γ Expression on Synovial and Peripheral T Cells and Monocytes in Patients with Rheumatoid Arthritis RIIKKA NISSINEN, MARJATTA LEIRISALO-REPO, MINNA TIITTANEN, HEIKKI JULKUNEN, HANNA HIRVONEN, TIMO PALOSUO, and OUTI VAARALA ABSTRACT. Objective. To characterize cytokine and chemokine receptor profiles of T cells and monocytes in inflamed synovium and peripheral blood (PB) in patients with rheumatoid arthritis (RA) and other arthritides. Methods. We studied PB and synovial fluid (SF) samples taken from 20 patients with RA and 9 patients with other arthritides. PB cells from 8 healthy adults were used as controls. CCR3, CCR5, and intracellular interferon-γ (IFN-γ) and interleukin 4 (IL-4) expression in CD8+ and CD8– T cell populations and in CD14+ cells were determined with flow cytometry. Results. Expression of CCR5 and CCR3 by CD8–, CD8+ T cells and CD14+ monocytes was increased in SF compared to PB cells in patients with RA and other arthritides. The number of CD8+ T cells spontaneously expressing IL-4 and IFN-γ was higher in SF than in PB in RA patients. Spontaneous CCR5 expression was associated with intracellular IFN-γ expression in CD8+ T cells derived from SF in RA. In CD8– T cells the ratio of CCR5+/CCR3+ cells was increased in patients with RA compared to patients with other arthritides. The number of PB CD8– T cells expressing IFN-γ after mitogen stimulation was higher in controls than in patients. In PB monocytes the ratio of CCR5+/CCR3+ cells was increased in patients with RA compared to patients with other arthri- tides and controls. -

Role of Chemokines in Hepatocellular Carcinoma (Review)
ONCOLOGY REPORTS 45: 809-823, 2021 Role of chemokines in hepatocellular carcinoma (Review) DONGDONG XUE1*, YA ZHENG2*, JUNYE WEN1, JINGZHAO HAN1, HONGFANG TUO1, YIFAN LIU1 and YANHUI PENG1 1Department of Hepatobiliary Surgery, Hebei General Hospital, Shijiazhuang, Hebei 050051; 2Medical Center Laboratory, Tongji Hospital Affiliated to Tongji University School of Medicine, Shanghai 200065, P.R. China Received September 5, 2020; Accepted December 4, 2020 DOI: 10.3892/or.2020.7906 Abstract. Hepatocellular carcinoma (HCC) is a prevalent 1. Introduction malignant tumor worldwide, with an unsatisfactory prognosis, although treatments are improving. One of the main challenges Hepatocellular carcinoma (HCC) is the sixth most common for the treatment of HCC is the prevention or management type of cancer worldwide and the third leading cause of of recurrence and metastasis of HCC. It has been found that cancer-associated death (1). Most patients cannot undergo chemokines and their receptors serve a pivotal role in HCC radical surgery due to the presence of intrahepatic or distant progression. In the present review, the literature on the multi- organ metastases, and at present, the primary treatment methods factorial roles of exosomes in HCC from PubMed, Cochrane for HCC include surgery, local ablation therapy and radiation library and Embase were obtained, with a specific focus on intervention (2). These methods allow for effective treatment the functions and mechanisms of chemokines in HCC. To and management of patients with HCC during the early stages, date, >50 chemokines have been found, which can be divided with 5-year survival rates as high as 70% (3). Despite the into four families: CXC, CX3C, CC and XC, according to the continuous development of traditional treatment methods, the different positions of the conserved N-terminal cysteine resi- issue of recurrence and metastasis of HCC, causing adverse dues.