Topical Corticosteroids: Applications in Dentistry
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Betamethasone Valerate Foam: a Look at the Clinical Data
Review: Clinical Trial Outcomes Betamethasone valerate foam: a look at the clinical data Clin. Invest. (2014) 4(3), 259–267 Topical corticosteroids and especially betamethasone valerate (BMV) have Avner Shemer1, Nicole Sakka1 & been used topically to relieve many inflammatory skin conditions such as Dov Tamarkin*2 psoriasis and atopic dermatitis. The vehicle used to deliver topical drugs 1Department of Dermatology, the Chaim Sheba Medical Center, Affiliated with the can influence the performance of these topical applications. BMV has Tel-Aviv University, Sackler School of Medicine, traditionally been available in creams, ointments, lotions and sprays. In Tel Hashomer, Israel the early 2000s, a topical hydroethanolic BMV foam became commercially 2Foamix Ltd., 2 Holzman Street, Weizmann available. Subsequently, alcohol-free emulsion- and petrolatum-based Science Park, Rehovot 76704, Israel foam formulations were also developed. This manuscript reviews the *Author for correspondence: Tel.: +972 52 457 5677 properties of BMV foams and clinical studies that have been conducted Fax: +972 8 853 1102 to assess their efficacy and safety as treatments for scalp and non-scalp [email protected] psoriasis, as well as other dermatological inflammatory conditions. Keywords: betamethasone valerate • foam • psoriasis • topical corticosteroids Topical corticosteroids have been ranked in four groups consisting of seven classes ranging from ultra-high potency preparations (class 1) to low-potency prepara- tions (class 7). Betamethasone valerate (BMV) is a mid-potency corticosteroid (class 3–5, depending on the dosage form), used topically to relieve inflammatory skin conditions. It is used as a treatment for psoriasis, atopic dermatitis and other corticosteroid-responsive dermatoses. The vehicle used to deliver topical drugs can influence the performance of these drugs. -

Albany-Molecular-Research-Regulatory
PRODUCT CATALOGUE API COMMERCIAL US EU Japan US EU Japan API Name Site CEP India API Name Site CEP India DMF DMF DMF DMF DMF DMF A Abiraterone Malta • Benztropine Mesylate Cedarburg • Adenosine Rozzano - Quinto de' Stampi • • * Betaine Citrate Anhydrous Bon Encontre • Betametasone-17,21- Alcaftadine Spain Spain • • Dipropionate Sterile • Alclometasone-17, 21- Spain Betamethasone Acetate Spain Dipropionate • • Altrenogest Spain • • Betamethasone Base Spain Amphetamine Aspartate Rensselaer Betamethasone Benzoate Spain * Monohydrate Milled • Betamethasone Valerate Amphetamine Sulfate Rensselaer Spain * • Acetate Betamethasone-17,21- Argatroban Rozzano - Quinto de' Stampi Spain • • Dipropionate • • • Atenolol India • • Betamethasone-17-Valerate Spain • • Betamethasone-21- Atracurium Besylate Rozzano - Quinto de' Stampi Spain • Phosphate Disodium Salt • • Bromfenac Monosodium Atropine Sulfate Cedarburg Lodi * • Salt Sesquihydrate • • Azanidazole Lodi Bromocriptine Mesylate Rozzano - Quinto de' Stampi • • • • • Azelastine HCl Rozzano - Quinto de' Stampi • • Budesonide Spain • • Aztreonam Rozzano - Valle Ambrosia • • Budesonide Sterile Spain • • B Bamifylline HCl Bon Encontre • Butorphanol Tartrate Cedarburg • Beclomethasone-17, 21- Spain Capecitabine Lodi Dipropionate • C • 2 *Please contact our Accounts Managers in case you are interested in this API. 3 PRODUCT CATALOGUE API COMMERCIAL US EU Japan US EU Japan API Name Site CEP India API Name Site CEP India DMF DMF DMF DMF DMF DMF Dexamethasone-17,21- Carbimazole Bon Encontre Spain • Dipropionate -

(12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 De Juan Et Al
US 200601 10428A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 de Juan et al. (43) Pub. Date: May 25, 2006 (54) METHODS AND DEVICES FOR THE Publication Classification TREATMENT OF OCULAR CONDITIONS (51) Int. Cl. (76) Inventors: Eugene de Juan, LaCanada, CA (US); A6F 2/00 (2006.01) Signe E. Varner, Los Angeles, CA (52) U.S. Cl. .............................................................. 424/427 (US); Laurie R. Lawin, New Brighton, MN (US) (57) ABSTRACT Correspondence Address: Featured is a method for instilling one or more bioactive SCOTT PRIBNOW agents into ocular tissue within an eye of a patient for the Kagan Binder, PLLC treatment of an ocular condition, the method comprising Suite 200 concurrently using at least two of the following bioactive 221 Main Street North agent delivery methods (A)-(C): Stillwater, MN 55082 (US) (A) implanting a Sustained release delivery device com (21) Appl. No.: 11/175,850 prising one or more bioactive agents in a posterior region of the eye so that it delivers the one or more (22) Filed: Jul. 5, 2005 bioactive agents into the vitreous humor of the eye; (B) instilling (e.g., injecting or implanting) one or more Related U.S. Application Data bioactive agents Subretinally; and (60) Provisional application No. 60/585,236, filed on Jul. (C) instilling (e.g., injecting or delivering by ocular ion 2, 2004. Provisional application No. 60/669,701, filed tophoresis) one or more bioactive agents into the Vit on Apr. 8, 2005. reous humor of the eye. Patent Application Publication May 25, 2006 Sheet 1 of 22 US 2006/0110428A1 R 2 2 C.6 Fig. -

Improved Penetrating Topical Pharmaceutical Compositions Containing Corticosteroids
Europaisches Patentamt ® European Patent Office © Publication number: 0 129 283 Office europeen des brevets A2 © EUROPEAN PATENT APPLICATION © Application number: 84200821.1 ©Int CI.3: A 61 K 31/57 A 61 K 47/00, A 61 K 9/06 © Date of filing: 12.06.84 © Priority: 21.06.83 US 506274 © Applicant: THE PROCTER & GAMBLE COMPANY 01.02.84 US 576065 301 East Sixth Street Cincinnati Ohio 45201 (US) © Date of publication of application: © Inventor: Cooper, Eugene Rex 27.12.84 Bulletin 84/52 2425 Ambassador Drive Cincinnati, OH 45231 (US) © Designated Contracting States: BE CH DE FR GB IT Li NL SE © Inventor: Loomans, Maurice Edward 5231 Jessup Road Cincinnati, OH 45239IUS) © Inventor: Fawzi, Mahdi Bakir 11 Timberline Drive Flanders New Jersey 07836(US) © Representative: Suslic, Lydia et al, Procter & Gamble European Technical Center Temselaan 100 B-1820 Strombeek-Bever(BE) © Improved penetrating topical pharmaceutical compositions containing corticosteroids. Topical pharmaceutical compositions containing a cor- ticosteroid component and a penetration-enhancing vehicle are disclosed. The vehicle comprises a binary combination of a C3-C4 diol and a "cell-envelope disordering compound". The vehicle provides marked transepidermal and percutaneous delivery of corticosteroids. A method of treating certain rheumatic and inflammatory conditions, systemically or loc- ally, is also disclosed. TECHNICAL FIELD The present invention relates to topical compositions effective in delivering high levels of certain pharmaceutically-active cor- ticosteroid agents through the integument. Because of the ease of access, dynamics of application, large surface area, vast exposure to the circulatory and lymphatic networks, and non-invasive nature of the treatment, the delivery of pharmaceutically-active agents through the skin has long been a promising concept. -

AMRI India Pvt
WE’VE GOT API DEVELOPMENT AND MANUFACTURING DOWN TO AN EXACT SCIENCE API Commercial Product Catalogue PRODUCT CATALOGUE API Commercial US EU Japan US EU Japan API Name Site CEP India China API Name Site CEP India China DMF DMF DMF DMF DMF DMF Rozzano Quinto de Adenosine Betaine Citrate Anhydrous Bon Encontre, France A Stampi, Italy • Betametasone-17,21- Alcaftadine Valladolid, Spain Valladolid, Spain • Dipropionate Sterile • Alclometasone-17,21- Valladolid, Spain Betamethasone Acetate Valladolid, Spain Dipropionate • • • Altrenogest Valladolid, Spain • • Betamethasone Base Valladolid, Spain Aminobisamide HCl Rensselaer, US Betamethasone Benzoate Valladolid, Spain Amphetamine Aspartate Betamethasone Valerate Rensselaer, US Valladolid, Spain Monohydrate Milled • Acetate Betamethasone-17,21- Amphetamine Sulfate Rensselaer, US Valladolid, Spain • Dipropionate • • • • Rozzano Quinto de Argatroban Betamethasone-17-Valerate Valladolid, Spain Stampi, Italy • • • • Betamethasone-21- Atenolol Aurangabad, India Valladolid, Spain • • • Phosphate Disodium Salt • • Rozzano Quinto de Bromfenac Monosodium Atracurium Besylate Lodi, Italy Stampi, Italy • Salt Sesquihydrate • • Rozzano Quinto de Atropine Sulfate Grafton, US Bromocriptine Mesylate • Stampi, Italy • • • Rozzano Quinto de Azelastine HCl Budesonide Valladolid, Spain Stampi, Italy • • • • • Rozzano Valleambrosia, Aztreonam (not sterile) Budesonide Sterile Valladolid, Spain Italy • • • • B Bamifylline HCl Bon Encontre, France • C Capecitabine Lodi, Italy • • Beclomethasone-17,21- Valladolid, Spain -

(12) Patent Application Publication (10) Pub. No.: US 2011/0159073 A1 De Juan Et Al
US 20110159073A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2011/0159073 A1 de Juan et al. (43) Pub. Date: Jun. 30, 2011 (54) METHODS AND DEVICES FOR THE Publication Classification TREATMENT OF OCULAR CONDITIONS (51) Int. Cl. (76) Inventors: Eugene de Juan, LaCanada, CA A6F 2/00 (2006.01) (US); Signe E. Varner, Los (52) U.S. Cl. ........................................................ 424/427 Angeles, CA (US); Laurie R. Lawin, New Brighton, MN (US) (57) ABSTRACT Featured is a method for instilling one or more bioactive (21) Appl. No.: 12/981,038 agents into ocular tissue within an eye of a patient for the treatment of an ocular condition, the method comprising con (22) Filed: Dec. 29, 2010 currently using at least two of the following bioactive agent delivery methods (A)-(C): (A) implanting a Sustained release Related U.S. Application Data delivery device comprising one or more bioactive agents in a (63) Continuation of application No. 1 1/175,850, filed on posterior region of the eye so that it delivers the one or more Jul. 5, 2005, now abandoned. bioactive agents into the vitreous humor of the eye; (B) instill ing (e.g., injecting or implanting) one or more bioactive (60) Provisional application No. 60/585,236, filed on Jul. 2, agents Subretinally; and (C) instilling (e.g., injecting or deliv 2004, provisional application No. 60/669,701, filed on ering by ocular iontophoresis) one or more bioactive agents Apr. 8, 2005. into the vitreous humor of the eye. Patent Application Publication Jun. 30, 2011 Sheet 1 of 22 US 2011/O159073 A1 Patent Application Publication Jun. -
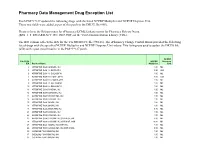
Pharmacy Data Management Drug Exception List
Pharmacy Data Management Drug Exception List Patch PSS*1*127 updated the following drugs with the listed NCPDP Multiplier and NCPDP Dispense Unit. These two fields were added as part of this patch to the DRUG file (#50). Please refer to the Release notes for ePharmacy/ECME Enhancements for Pharmacy Release Notes (BPS_1_5_EPHARMACY_RN_0907.PDF) on the VistA Documentation Library (VDL). The IEN column reflects the IEN for the VA PRODUCT file (#50.68). The ePharmacy Change Control Board provided the following list of drugs with the specified NCPDP Multiplier and NCPDP Dispense Unit values. This listing was used to update the DRUG file (#50) with a post install routine in the PSS*1*127 patch. NCPDP File 50.68 NCPDP Dispense IEN Product Name Multiplier Unit 2 ATROPINE SO4 0.4MG/ML INJ 1.00 ML 3 ATROPINE SO4 1% OINT,OPH 3.50 GM 6 ATROPINE SO4 1% SOLN,OPH 1.00 ML 7 ATROPINE SO4 0.5% OINT,OPH 3.50 GM 8 ATROPINE SO4 0.5% SOLN,OPH 1.00 ML 9 ATROPINE SO4 3% SOLN,OPH 1.00 ML 10 ATROPINE SO4 2% SOLN,OPH 1.00 ML 11 ATROPINE SO4 0.1MG/ML INJ 1.00 ML 12 ATROPINE SO4 0.05MG/ML INJ 1.00 ML 13 ATROPINE SO4 0.4MG/0.5ML INJ 1.00 ML 14 ATROPINE SO4 0.5MG/ML INJ 1.00 ML 15 ATROPINE SO4 1MG/ML INJ 1.00 ML 16 ATROPINE SO4 2MG/ML INJ 1.00 ML 18 ATROPINE SO4 2MG/0.7ML INJ 0.70 ML 21 ATROPINE SO4 0.3MG/ML INJ 1.00 ML 22 ATROPINE SO4 0.8MG/ML INJ 1.00 ML 23 ATROPINE SO4 0.1MG/ML INJ,SYRINGE,5ML 5.00 ML 24 ATROPINE SO4 0.1MG/ML INJ,SYRINGE,10ML 10.00 ML 25 ATROPINE SO4 1MG/ML INJ,AMP,1ML 1.00 ML 26 ATROPINE SO4 0.2MG/0.5ML INJ,AMP,0.5ML 0.50 ML 30 CODEINE PO4 30MG/ML -

1 Topical Corticosteroids in Children
Pediatric Pharmacotherapy A Monthly Review for Health Care Professionals of the Children's Medical Center Volume 2, Number 1, January 1996 Topical Corticosteroid Preparations • Overview • Comparing Potencies o very high potency o high potency o moderate potency o low potency • Selecting a Vehicle • Evaluating Toxicity • Combination Products • Instructions for Parents • References Pharmacology Literature Reviews • Placental Drug Transfer • Antiepileptic Pharmacokinetics • Gentamicin in Children with Cancer Formularly Update Nearly fifty years ago the first topical corticosteroid preparation, hydrocortisone, was introduced in the United States, making a dramatic impact on the management of pediatric dermatologic conditions. Since that time, a wide spectrum of products has been developed in an effort to maximize anti -inflammatory properties while minimizing mineralocorticoid activity and adverse effects. Topical corticosteroid preparations have become a cornerstone in the treatment of children with a variety of skin conditions, including atopic dermatitis, psoriasis, eczema, seborrheic dermatitis, contact dermatitis, and some types of burns. They are useful adjunctive therapy in other dermatologic conditions, such as porphyria, lupus, epidermolysis bullosa, and severe cases of diaper dermatitis in infants.1 This brief review will focus on issues related to potency and drug selection, differences in vehicles, toxicities, and the use of combination corticosteroid products.2-5 Comparing Potency The most common method for comparing topical corticosteroid products is relat ive potency. Potency is determined by the degree of tissue penetration of a product (bioavailability) and the resulting vasoconstriction (skin -blanching) that is produced. It may not be relevant to efficacy in treating specific skin conditions. Testing to determine potency is conducted by pharmaceutical manufacturers and reflects a particular name brand product. -

Recent Advances in the Analysis of Steroid Hormones and Related Drugs
ANALYTICAL SCIENCES MAY 2004, VOL. 20 767 2004 © The Japan Society for Analytical Chemistry Reviews Recent Advances in the Analysis of Steroid Hormones and Related Drugs Sándor GÖRÖG Gedeon Richter Ltd., P.O.B. 27, H-1475 Budapest, Hungary The development during the last 15 years and the state-of-the-art in the analysis of bulk steroid hormone drugs and hormone-like structures and pharmaceutical formulations made thereof are summarized. Other steroids (sterols, bile acids, cardiac glycosides, vitamins D) as well as biological-clinical aspects and pharmacokinetic and metabolic studies are excluded from this review. The state-of-the-art is summarized based on comparisons of monographs in the latest editions of the European Pharmacopoeia, United States Pharmacopoeia and the Japanese Pharmacopoeia. This is followed by sections dealing with new developments in the methodology for the fields of spectroscopic and spectrophotometric, chromatographic, electrophoretic and hyphenated techniques as well electroanalytical methods. The review is terminated by two problem-oriented sections: examples on impurity and degradation profiling as well as enantiomeric analysis. (Received January 14, 2004; Accepted February 2, 2004) 1 Introduction 767 4·3 Supercritical fluid chromatography (SFC) 2 Steroid Hormone Drugs in Pharmacopoeias 768 4·4 High-performance liquid chromatography 2·1 Assay of bulk drug materials (HPLC) and HPLC-MS 2·2 Related impurities test of bulk drug materials 5 Electrophoretic and Related Methods 776 2·3 Assay of steroid hormone formulations -

(12) United States Patent (10) Patent No.: US 7,198,800 B1 K0 (45) Date of Patent: Apr
US007 198800B1 (12) United States Patent (10) Patent No.: US 7,198,800 B1 K0 (45) Date of Patent: Apr. 3, 2007 (54) COMPOSITIONS AND METHODS (56) References Cited (75) Inventor: Thomas Sai Ying Ko. 4 Licence Road, U.S. PATENT DOCUMENTS Belgrave South, Victoria, 3160 (AU) 3,987,000 A * 10/1976 Gleichenhagen et al. ... 523/111 Y re. - - - 5,041.287 A * 8/1991 Driggers et al. .............. 424,81 (73) Assignee: Thomas Sai Ying Ko, Beijing (CN) 5,632,727 A * 5/1997 Tipton et al. ................. 602/47 5,708,023 A * 1/1998 Modak et al. .... ... 514,494 (*) Notice: Subject to any disclaimer, the term of this 5,725.491 A * 3/1998 Tipton et al. ................. 602/43 patent is extended or adjusted under 35 6,183,770 B1* 2/2001 Muchin et al. ............. 424/448 U.S.C. 154(b) by 781 days. * cited by examiner (21) Appl. No.: 09/717,088 Primary Examiner Sreeni Padmanabhan Assistant Examiner Gina Yu (22) Filed: Nov. 22, 2000 (74) Attorney, Agent, or Firm—Sughrue Mion, PLLC (30) Foreign Application Priority Data (57) ABSTRACT Nov. 23, 1999 (AU) ..................................... PQ4190 Non-aerosol spray-on skin patch compositions as described (51) Int. Cl. comprising at least one Substantially water insoluble film A6DF 3/00 (2006.01) forming agent, at least one film plasticizer agent, at least one AOIN 55/00 (2006.01) water soluble compound, and at least one organic solvent, (52) U.S. Cl. ...................... 424/443; 424/447; 424/448: the composition forming a flexible, porous and physiologi 424/449; 424/78.35: 525/363; 514/887: 514/494; cally compatible skin patch when sprayed on to skin and 602/43; 602/47 allowed to dry. -

(12) United States Patent (10) Patent No.: US 6,890,544 B2 Mccadden (45) Date of Patent: May 10, 2005
USOO6890544B2 (12) United States Patent (10) Patent No.: US 6,890,544 B2 McCadden (45) Date of Patent: May 10, 2005 (54) GEL COMPOSITION FOR THE TOPICAL David B. Jackson et al. “Bioeduivalence (bioavailability) of TREATMENT OF POSON IVY AND OTHER General Topical Corticosteroids' Journal of the American FORMS OF CONTACT DERMATITIS Academy of Dermatology, vol. 20, No. 5, Pt. 1 (May 1989) pp. 791-796. (76) Inventor: Michael E. McCadden, 121 Cynthia A. Guzzo et al. “Chapter 64, Dermatological Phar Whitebridge Meadows La., St. Louis, macology' Goodman & Gilman's The Pharmacological MO (US) 63141 Basis of Therapeutics, 9th Ed., McGraw-Hill (1996) pp. 1593-1598. (*) Notice: Subject to any disclaimer, the term of this G. S. Shankland et al. “Comparative in-vitro Activity of patent is extended or adjusted under 35 Clortimazole and a Clotrimazole/hydrocortisone Combina U.S.C. 154(b) by 0 days. tion in the Treatment of Experimental Dermatophytosis in Guinea Pigs’ Journal of Antimicrobial Chemotherapy, vol. 25 (1990) pp. 825–830. (21) Appl. No.: 10/292,251 Roger C. Cornell et al. “Correlation of the Vasoconstriction (22) Filed: Nov. 12, 2002 Assay and Clinical Activity in Psoriasis' Arch Dermatol, vol. 121 (Jan. 1985) pp. 63–67. (65) Prior Publication Data Thomas B. Fitzpatricket al. Dermatology In General Medi cine, vol. II, 4th Ed., McGraw-Hill, Inc., (1993) pp. US 2003/0077304 A1 Apr. 24, 2003 2444-2447 and 2847. E.G.V. Evans et al. “Does Naftifine Have Anti-Inflamma Related U.S. Application Data tory Properties? A Double-blind Comparative Study With (63) Continuation of application No. -
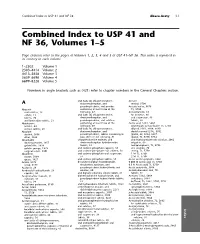
Combined Index to USP 41 and NF 36, Volumes 1–5
Combined Index to USP 41 and NF 36 Abaca-Acety I-1 Combined Index to USP 41 and NF 36, Volumes 1–5 Page citations refer to the pages of Volumes 1, 2, 3, 4 and 5 of USP 41±NF 36. This index is repeated in its entirety in each volume. 1–2302 Volume 1 2303–4414 Volume 2 4415–5658 Volume 3 5659–6698 Volume 4 6699–8228 Volume 5 Numbers in angle brackets such as 〈421〉 refer to chapter numbers in the General Chapters section. and (salts of) chlorpheniramine, Acetate A dextromethorphan, and methyl, 5706 pseudoephedrine, oral powder Acetate buffer, 5676 Abacavir containing at least three of the TS, 5750 oral solution, 19 following, 47 Acetazolamide, 65 sulfate, 23 and (salts of) chlorpheniramine, for injection, 66 tablets, 20 dextromethorphan, and oral suspension, 68 and lamivudine tablets, 21 pseudoephedrine, oral solution tablets, 68 Abiraterone containing at least three of the Acetic acid, 5181, 5664 acetate, 24 following, 49 ammonium acetate buffer TS, 5750 acetate tablets, 26 and (salts of) chlorpheniramine, diluted, 5181, 5664, 5690 Absolute dextromethorphan, and double-normal (2 N), 5762 alcohol, 5666 pseudoephedrine, tablets containing at glacial, 69, 5664, 5697 ether, 5664 least three of the following, 51 glacial, TS, 5750, 5754 Absorbable chlorpheniramine maleate, and and hydrocortisone otic solution, 2062 dusting powder, 1457 dextromethorphan hydrobromide irrigation, 69 gelatin film, 1929 tablets, 53 metaphosphoric, TS, 5756 gelatin sponge, 1929 and codeine phosphate capsules, 55 otic solution, 70 surgical suture, 3901 and codeine phosphate