Patient Profile Based Management Approach for Optimal Treatment of Angina: a Consensus from India Cases
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Accused Persons Arrested in Thrissur City District from 12.06.2016 to 18.06.2016
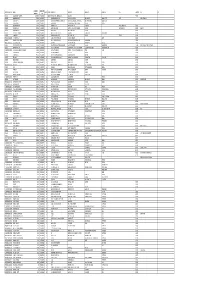
Accused Persons arrested in Thrissur City district from 12.06.2016 to 18.06.2016 Name of Name of the Name of the Place at Date & Arresting Court at Sl. Name of the Age & Cr. No & Sec Police father of Address of Accused which Time of Officer, which No. Accused Sex of Law Station Accused Arrested Arrest Rank & accused Designation produced 1 2 3 4 5 6 7 8 9 10 11 KOLAPPULLY HOUSE, 2078/16 U/S TOWN EAST 12.06.2016 M K AJAYAN, SI BAILED BY 1 RAGESH K R RAJAN 29 MALE MULAYAM P O, DIVANJIMOOLA 15(C) R/W 63 PS (THRISSUR at 00.15 OF POLICE POLICE VALAKKAVU ABKARAI ACT CITY) AMBATT HOUSE, 2079/16 U/S TOWN EAST 12.06.2016 M K AJAYAN, SI BAILED BY 2 VARGHESE A T THOMAS 46 MALE MULAYAM P O , DIVANJIMOOLA 15(C) R/W 63 PS (THRISSUR at 00.22 OF POLICE POLICE VALAKKAVU ABKARAI ACT CITY) MELAYIL HOUSE, 2080/16 U/S TOWN EAST RAMACHAND 12.06.2016 M K AJAYAN, SI BAILED BY 3 RAMAN 47 MALE MULAYAM P O , DIVANJIMOOLA 15(C) R/W 63 PS (THRISSUR RAN at 00.30 OF POLICE POLICE VALAKKAVU ABKARAI ACT CITY) MULLOOKKARAN 2081/16 U/S T OWN EAST 12.06.2016 M.K. AJAYAN, BAILED BY 4 SHIJI RAPPAI 39 MALE HOUSE, MULAYAM DIVANJIMOOLA 15(C) R/W 63 PS (THRISSUR AT 00.29 SI OF POLICE POLICE VALAKKAVU ABKARAI ACT CITY) PALUKKASSERY 2082/16 U/S TOWN EAST CHANDRASEKH 12.06.2016 M K AJAYAN, SI BAILED BY 5 RAJKUMAR 48 MALE HOUSE, MULAYAM P DIVANJIMOOLA 15(C) R/W 63 PS (THRISSUR ARAN at 00.50 OF POLICE POLICE O , VALAKKAVU ABKARAI ACT CITY) THACHATTIL HOUSE,NEAR 2084/16 U/S TOWN EAST V.K. -

Accused Persons Arrested in Thrissur City District from 17.01.2021 to 23.01.2021
Accused Persons arrested in Thrissur City district from 17.01.2021 to 23.01.2021 Name of Name of the Name of the Place at Date & Arresting Court at Sl. Name of the Age & Cr. No & Sec Police father of Address of Accused which Time of Officer, which No. Accused Sex of Law Station Accused Arrested Arrest Rank & accused Designation produced 1 2 3 4 5 6 7 8 9 10 11 MARUTHOOR KARTHIAYA Thrissur HOUSE, NI TEMPLE 23-01-2021 RAMACHA 33, 80/2021 U/s West BYJU K.C. SI BAILED BY 1 RAGHU KARTHIAYANI ROAD at 22:05 NDRAN Male 151 CrPC (Thrissur OF POLICE POLICE TEMPLE, AYYANTHO Hrs City) AYYANTHOLE LE Thrissur ODAYIL 23-01-2021 122/2021 U/s RADHAKRI 36, NR KALYAN East ANUDAS .K, BAILED BY 2 RAKESH (H),KUTTUMUKKU at 23:00 279 IPC & 185 SHNAN Male JEWELLERS (Thrissur SI OF POLICE POLICE , THRISSUR Hrs MV ACT City) Koothumakkal 23-01-2021 71/2021 U/s Peramangal 48, BAILED BY 3 Sreekumar Appu House, Varadiyam at 20:15 118(e) of KP am (Thrissur Sreejith S I Male POLICE Peringottukara Hrs Act City) CHOONDAKARA Thrissur N (H), NEAR 23-01-2021 26, 121/2021 U/s East ANUDAS .K, BAILED BY 4 THOMAS PAULSON THOTTAPPADY, SAPNA at 20:35 Male 279, 283 IPC (Thrissur SI OF POLICE POLICE ANCHERY, THEATRE Hrs City) THRISSUR ERATH (H), Thrissur 23-01-2021 119/2021 U/s 27, VALARKAVU, BTR ITC East ANUDAS .K, BAILED BY 5 SANOOP SUNIL at 19:00 279 IPC & 185 Male NAGAR, JUNCTION (Thrissur SI OF POLICE POLICE Hrs MV ACT KURIACHIRA City) KEEDAM KUNNATH(H)THI 51/2021 U/s PAZHAYA NIZAMUDDI 23-01-2021 GOPALAKR RAMAKRIS 39, RUVADI,PUDUKK PAZHAYAN 279 IPC & NNUR N J, BAILED BY 6 at -

KERALA LAKSHMI MILLS (A Unit of NTC Limited, Government of India Undertaking) PULLAZHI,THRISSUR-680012
KERALA LAKSHMI MILLS (A Unit of NTC Limited, Government of India Undertaking) PULLAZHI,THRISSUR-680012 Ref: KLM/GM/COTTON WASTE/2017-18/ET/JAN- MAR/ Date: 10-01-2018 TENDER FOR COTTON/PC WASTE Sealed Tenders(Without price bid) are invited by the undersigned (Merchants and others) dealing in Cotton Waste, to purchase Cotton Waste produced in our mills 01-.01-.2018 to 31.03.2018 on the following terms and conditions: - ` 1. Every Tender terms and conditions along with EMD should be sent in a Sealed Cover addressed to the General Manager, KERALA LAKSHMI MILLS,PULLAZHI THRISSUR so as to be received by the undersigned not later than 3.00 PM on 25.01.2018 (without price bid) 2. The sealed covers of the tenders should be superscribed on the top as “TENDER FOR PURCHASE OF COTTON WASTE available at KERALA LAKSHMI MILLS, THRISSUR”. 3. The materials mentioned in the Annexure can be inspected at the premises of Kerala Lakshmi Mills on any day (except Sundays and Holidays) between 10.00 AM and 4.00 PM 4. The allotted materials should be accepted by the Tenderers in “AS IS WHERE CONDITION”, which is in pressed Bale/Borah form, (Cotton waste) approximate weight around 50-130kgs. 5. The Tender should remit EMD 2 days before the commencement of the tender and scheduled Tender should be accompanied by Tender Deposit(will not carry any interest) (Earnest Money Deposit) of 30,000/-(Rupees Thirty Thousand only) per tender by means of an “Account payee” Pay order/Demand Draft drawn in favor of KERALA LAKSHMI MILLS, THRISSUR, on any Nationalized/Scheduled Bank payable at Thrissur and payment by any other means will neither be accepted nor recognized. -

Dept. of Computer Science and Applications Academic Year 2015-2016
Dept. of Computer Science and Applications Academic Year 2015-2016 World Environment Day Celebration: As part of world environment day celebration, Department of Computer Science and Application organized a cartoon Competition on 9th June 2015. As we all know, the aim of world environment day, is to spread awareness and to encourage people to take action and to protect the environment , we gave a topic ‘Sustainable Living in Digital Era’ to the participating students to visualize their ideas and express their knowledge .Students from various departments participated in the competition. Their creative cartoons were judeged by Sri.Jayasurya, Retd Professor, School of Drama, Thrissur. The winners wre Prize 1 : Ms. Anupriya C.S. III BCA Prize 2 : Ms. Krishnapriya II DC Chemistry Prize 3 : Ms. Nishan A. Salim III BCA Digital India Week celebrations: As part of Digital India Week celebration, department of Computer Science and Applications had organized a series of activities. On 6th July 2015 ,the department of Computer Science and Applications and Vocational Studies organized an inauguration program of Digital India Week . The event was inaugurated by our Principal Sr.Dr. Jacinitha by launching the video of Digital India followed by a presentation on “What is digital India “ and an introductory session on Sixth Sense technology by our students . We conducted a rally as a part of Digital India Week. Also there was a demonstration of logo of Digital India by our students. On 8th July 2015 the department of Computer Science and Applications conducted an awareness class on the topic “How to be safe on internet “at Jubilee hall, which was a powerpoint presentation by our student. -

Accused Persons Arrested in Thrissur City District from 28.02.2021To06.03.2021
Accused Persons arrested in Thrissur City district from 28.02.2021to06.03.2021 Name of Name of the Name of the Place at Date & Arresting Court at Sl. Name of the Age & Cr. No & Sec Police father of Address of Accused which Time of Officer, which No. Accused Sex of Law Station Accused Arrested Arrest Rank & accused Designation produced 1 2 3 4 5 6 7 8 9 10 11 135/2021 U/s Sec. 4(2)(e)(j) PANICHAKATH r/w 3(b) of VADAKEK 06-03-2021 20, HOUSE PANANTHA Kerala AD P.R RAJEEV, BAILED BY 1 HASSAN IBRAHIM at 00:00 Male VELIYAMCODE , RA Epidemic (Thrissur SI OF POLICE POLICE Hrs MALAPPURAM Diseases City) Ordinance 2020 PANAMUKU 06-03-2021 181/2021 U/s Pavaratty CHANDRA 31, HOUSE MULLASSER BAILED BY 2 ANPPO at 21:20 118(e) of KP (Thrissur SUJITH R.P N Male THANAVEEDHI Y POLICE Hrs Act City) MULLASSERY THEKKEPPURATH U KUNNAMK 06-03-2021 248/2021 U/s MUHAMME VELAYUDH 53, HOUSE,PERUMAN KUNNAMKU ULAM BAILED BY 3 VENU T V at 21:50 279 IPC & 185 D ABDUL AN Male NU DESAM LAM (Thrissur POLICE Hrs MV ACT NAZIR ,KECHERY City) ,KUNNAMKULAM 133/2021 U/s Sec. 4(2)(e)(j) KATTISSERY r/w 3(b) of VADAKEK 06-03-2021 45, HOUSE KADIKAD PANANTHA Kerala AD P.R RAJEEV, BAILED BY 4 VINAYAN VELAYI at 00:00 Male PUNNAYURKULA RA Epidemic (Thrissur SI OF POLICE POLICE Hrs M Diseases City) Ordinance 2020 132/2021 U/s Sec. 4(2)(e)(j) r/w 3(b) of VADAKEK cheruparambil veed, 06-03-2021 SREEDHAR 20, ALTHARA Kerala AD P.R RAJEEV, BAILED BY 5 VISHNU panthavoor at 00:00 AN Male EAST 2 KM Epidemic (Thrissur SI OF POLICE POLICE vadakkekad Hrs Diseases City) Ordinance 2020 PANNENGATH -

Agenda & Notes for the Meeting of the R T a , Thrissur to Be Held on 02-02
1 Agenda & Notes for the Meeting of the R T A , Thrissur to be held on 02-02-2018 at 10.30 A.M (Venue : Conference Hall, District Collectorate, Thrissur) PRESENT : CHAIRMAN :SHRI.DR.A.KOWSIGAN I A S DISTRICT COLLECTOR & CHAIRMAN, R T A, THRISSUR. MEMBER : SHRI YATHISH CHANDRA I. P. S, DISTRICT POLICE CHIEF, THRISSUR RURAL, ( MEMBER, R T A, THRISSUR) MEMBER : SHRI. SHAJI JOSEPH DEPUTY TRANSPORT COMMISSIONER, CENTRAL ZONE-1, THRISSUR. ( MEMBER, R T A, THRISSUR) 2 Item No.1 G-128759/2017 Agenda :. To Consider the application for the grant of fresh regular permit in respect of suitable stage carriage ( 28 seats in all ) to operate on the route Karappadam-Chalakkudy-Thiruthyparambu-Chembankunnu,via Kundukuzhipadam- Koorkamattom-MarancodeStMary’sChurch, Kuttikkadu-Poovathinkal-Paroyaram- Anamala junction-Sadayam College-Vellanchira-Annur-Kottat-Kuttikkadu church- Mechira-Chowka-VGM-Thazhur church-Nayarangadi- as Ordinary service Applicant:Sri. Shaju,Pariyadan House,P O Pattikkad,Thrissur Proposal Timings Karappad Chalakk Thiruthipara Chalakk Karappad Chebanku am udy mbu udy am nnu 6.20 6.58 7.00 7.20 7.40 7.53 8.31 8.32 10.45 10.00/10. 9.40 9.20 07 10.47 11.25 11.30 11.50 12.10 12.48 1.26 2.35 1.57 3.18 4.03 4.53 4.10 5.03 5.46 6.48 6.05 7.46Halt 7.08 Total route length- 54.8KM. Overlapping on the notified route – Nil 3 1) Trip.at,6.20ViaKundukuzhi,Koorkamattom,Kuttikkad,Pariyaram,Anamal a road 2) Trip at,7.00 Via Sadayan College,Vellanchira 3) Trip.at,7.53ViaAnamalaRoad,Pariyaram,Poovathinkal,Kuttikkad, Karunalayam, Kuttichira 4) Trip.at,9.10ViaKundukuzhi,Koorkamattom,Kuttikkad,Pariyaram,Anamal -

List of Hospitals Empanelled by Ssmc for Sst Services In
वर राय चकसा आयु कायालय OFFICE OF THE STATE MEDICAL COMMISSIONER कमचार राय बीमा नगम EMPLOYEES’ STATE INSURANCE CORPORATION , , , 680 020 ESIC पंचदप भवन उर वराज राउंड तृशूर िचंता से मुि PANCHDEEP BHAVAN, NORTH SWARAJ ROUND, THRISSUR, 680 020 Chinta Se Mukti दूरभाष/Phone: 0487-2330424 ; ईमेल / E-Mail: [email protected]; वेबसाइट/Website: esickerala.gov.in [आई एस ओ/ISO 9001 2008 (QS) माणत Certified] LIST OF HOSPITALS EMPANELLED BY SSMC FOR SST SERVICES IN KERALA Name & Address Services District Expiring on Extended upto 1 M/s Century Hospital, Neurosurgery, Urology, Alappuzha 31.03.2016 31.07.2016 Mulakuzha Chengannur, 689 Medical Gastro 509 Enterology, Nephrology 2 M/s Jospeh Kandathil Surgical Oncology, Alappuzha 31.03.2016 31.07.2016 Memorial Cancer Research Radiation Oncology Centre, Green Garden, Cherthala, 688524 3 M/s Malankara Orthodox Cardiology, Gastro Ernakulam 31.03.2016 31.07.2016 Syrian Church Medical College Enterology, Paediatric Hospital, Kolenchery, Kochi - Surgery Nephrology, 682311 Neurology & Neuro Surgery, Urology, Cardio Vascular & Cardio Thoracic Surgery 4 M/s Little Flower Hospital & Cardiology, Urology & Ernakulam 31.03.2016 31.07.2016 Research Centre, Post Box 23, Uro Surgery, Burns & Angamaly, 683 572 Plastic Surgery, Cardiothoracic Surgery, Gastro Entrology, Nephrology, Neurology & Neuro Surgery 5 M/s Lourdes Hospital, Cardiology, Neurology & Ernakulam 31.03.2016 31.07.2016 Ernakulam, Kochi - 682 012 Neuro surgery, Nephrology Urology, Onco Medicine & Onco Surgery, Burns & Plastic Surgery, Special, Cardio thoracic Investigations and Imaging (MRI, CT, Ultra Sound Scan, Mammography) 6 M/s KIMS Hospital, Neuro Surgery, Burns & Ernakulam 31.03.2016 31.07.2016 Pathadipalam, Edapally, Kochi, Plastic Surgery 682033 7 M/s Medall Healthcare Pvt. -
Mgl-Di219-Unpaid Share Holders List As on 31-03-2020
DIVIDEND WARRANT FOLIO-DEMAT ID NAME MICR DDNO ADDRESS 1 ADDRESS 2 ADDRESS 3 ADDRESS 4 CITY PINCODE JH1 JH2 AMOUNT NO 001221 DWARKA NATH ACHARYA 220000.00 192000030 680109 5 JAG BANDHU BORAL LANE CALCUTTA 700007 000642 JNANAPRAKASH P.S. 2200.00 192000034 18 POZHEKKADAVIL HOUSE P.O.KARAYAVATTAM TRICHUR DIST. KERALA STATE 68056 MRS. LATHA M.V. 000691 BHARGAVI V.R. 2200.00 192000035 19 C/O K.C.VISHWAMBARAN,P.B.NO.63 ADV.KAYCEE & KAYCEE AYYANTHOLE TRICHUR DISTRICT KERALA STATE 002679 NARAYANAN P S 2200.00 192000051 35 PANAT HOUSE P O KARAYAVATTOM, VALAPAD THRISSUR KERALA 002976 VIJAYA RAGHAVAN 2200.00 192000056 40 KIZHAKAYIL (H) KEEZHARIYUR P O KOVILANDY KHARRUNNISSA P M 000000 003124 VENUGOPAL M R 2200.00 192000057 41 MOOTHEDATH (H) SAWMILL ROAD KOORVENCHERY THRISSUR GEETHADEVI M V 000000 RISHI M.V. 003292 SURENDARAN K K 2068.00 192000060 44 KOOTTALA (H) PO KOOKKENCHERY THRISSUR 000000 003442 POOKOOYA THANGAL 2068.00 192000063 47 MECHITHODATHIL HOUSE VELLORE PO POOKOTTOR MALAPPURAM 000000 003445 CHINNAN P P 2200.00 192000064 48 PARAVALLAPPIL HOUSE KUNNAMKULAM THRISSUR PETER P C 000000 IN30611420024859 PUSHPA DEVI JAIN 2750.00 192000075 59 A-402, JAWAHAR ENCLAVE JAWAHAR NAGAR JAIPUR 302004 001431 JITENDRA DATTA MISRA 6600.00 192000079 63 BHRATI AJAY TENAMENTS 5 VASTRAL RAOD WADODHAV PO AHMEDABAD 382415 IN30177410163576 Rukaiya Kirit Joshi 2695.00 192000098 82 303 Anand Shradhanand Road Vile Parle East Mumbai 400057 000493 RATHI PRATAP POYYARA 2200.00 192000101 85 10,GREENVILLA,NETAJIPALKARMARG GHATKOPAR(WEST) MUMBAI MAHARASTRA 400084 MR. PRATAP APPUNNY POYYARA 001012 SHARAVATHY C.H. 2200.00 192000102 86 W/O H.L.SITARAMAN, 15/2A,NAV MUNJAL NAGAR,HOUSING CO-OPERATIVE SOCIETY CHEMBUR, MUMBAI 400089 1201090700097429 NANASAHEB BALIRAM SONAWANE 1606.00 192000114 98 2 PALLAWI HSG SOC. -

Kerala State Electricity Board Limited
KERALA STATE ELECTRICITY BOARD LIMITED (Incorporated under the Indian Companies Act, 1956) Office of the Chief Engineer (Human Resources Management) The following transfers and postings of Overseers (Electrical) are ordered Ref:- 1. This office order No.EB.4(b)/Overseer (Ele)/GT/T&P/2014 Dtd., Tvpm., 25.07.2014. 2. This office order No.EB.4(b)/Pro./90/Ovr/2014 Dtd., Tvpm., 18.02.2014. Sl. Name Present Office Office to Which posted Remarks No. Electrical Section, Transmission Circle, 1 Abdul Azeez K Areacode Malappuram Electrical Section, Electrical Circle, 2 Abdul Hameed P C Perla Kozhikode Electrical Section, Transmission Circle, 3 Abdul Khadar A P Tirurangadi Malappuram Electrical Section, Electrical Circle, 4 Abdul Khadar Kunju A Perappanangadi Harippad Transmission Circle, 5 Abdul Rahim A LMS, Edamon Alappuzha Abdul Salam V S 110 kV Substation, Transmission Circle, 6 (U/o. of transfer vide Sl. No.5 of Erattupettah Thodupuzha the order referred 1st above) Electrical Section, Transmission Circle, 7 Ajayakumar P Azhiyoor Kozhikode Electrical Section, Transmission Circle, 8 Ajayakumar P K Tanur Poovanthuruthu Electrical Circle, 9 Alaudheen S TC Section, Walayar Palakkad Electrical Circle, Electrical Section, 10 Amruthanathan K Thiruvananthapuram Pulamanthole (Urban) Electrical Section, Transmission Circle, 11 Anandakumar K S Puthuppally Poovanthuruthu Electrical Section, Transmission Circle, 12 Anandan M Thottilpalam Kalamassery Electrical Circle, Electrical Section, 13 Anilkumar G Thiruvananthapuram Manippuzha (Rural) Electrical Section, -

Industry Profile
INDUSTRY PROFILE Cotton is the most widely produced textile fabric today. It is believed that India was the first country to manufacture cotton. Among the finds at Mohenjodaro are a few scarps of cotton sticking to the side of a silver vase. This at least shows that cotton must have been used in India as far back as the 2nd millennium BC. Historically painted and printed cotton cloths are known to have been sold in Egypt and some parts of Europe long before the time of Alexander. (300BC). Cotton is soft fibre, probably the most important and truly a king fibre. The cotton plant is scientifically known as Gossypisum harbasium and it belongs to the family of Malvaceae. There are nearly 20 different species of cotton plants. All these grow in tropical and subtropical regions, and those growing in tropics are perennials while those in temperate regions annuals. The quality of cotton depends upon the whiteness, the purity, the length, the softness and regularity of the fibre. Because of its white colour and economic importance cotton is known as white gold. The main uses of cotton are for the manufacture of apparels, house hold articles and for industrial uses and their relative share is represented as 40% and 20% respectively. This king fibre is almost vital for the following products as shown by the list of variety of cotton products given in table 1.1. Table 1.1 The variety pf cotton products Automobile – tops Friction-tapes Tapes Bandages Fabrics Terry-cloth Book-Bindings Furniture covers Threads Canvas Hand kerchiefs Tickings Carpets Hosiery Tobaco-cloth Cheese cloth Lace Towelling Cloth-bags Mosquito-curtains Typewriter-ribbons Coverlets Paper Tyres Curtains Safety bags Umbrella-cloth Ducks Sheetings Wall-coverings Filter-cloth Shirts Washing cloth Fish-nets Shoe-laces yarns Millions in the world are directly dependent on this king fibre and the vagaries of this king (Flutuations in prices) wither make or mar millions- making them wither rich or poor and generally causing immense ups and downs. -
District Census Handbook, Trichur, Part X-A, XB, Series-9
CENSUS 1971 SERIES-9 KERALA DISTRICT CENSUS HANDBOOI{ TRICHUR PART X-A TOWN & VILLAGE DIRECTORY PART X-B PRIMARY CENSUS ABSTRACT K. NARAYANAN OF THE J)\DJAN ADMI::-rrSTRATIVE SEkVICE DlRECTOR OF CENSUS OPERATIONS KERALA 1974 7 0' TRICHUR DISTRICT ,0 ,_d I C" KILOM(TPE'So o 10 I~' L.ECENO _._._ DISTRlcr I!oOUNDARY -- -.- TALUK BOUNDARV ---- NATIONAL HIGHWAY ---- OTHEP IMPORTANT ROAD • RAILWAY- BROAD-GAUGE' ~7 RIVER ~ LAKE AND CA~A~ @ DISTRICT IoIEAOQI.IARTERS ® TALI.I" HEAOQUA~TE~S AND TOWill • TOWN @ TALUK NE4DQUARTEA~ EAST OF GREENWICH 76 IS' PREFACE The District Census Hand books were published for the first time in 1951 as part of the Census Publication Programme. Each Handbook contained a general account of the district and its people, census tables and statistics on the area, houses, population, general amenities and distribution of population by livelihood classes for each village and town. The 1961 District Census Handbooks were a distinct improvement on the 1951 volumes. A uniform procedure was adopted for the preparation of the Handbooks. Each Handbook contained three parts as detailed below: Part A. General, dealing with a general introduction about the district, its progress on various fields of general amenities since 1951 and an analysis of population by various demographic charact eristics. Part B. Census data, dealing with the census tables of 1961 pertaining to the district. Part C. Village/Town Directory, dealing with the amenities,Primary Census Abstract down to the level of karasjmuris/desoms in the case of rural areas and blocks and wards in the case of urban areas and number of industrial establishments by type. -
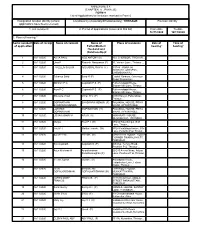
(CHAPTER V , PARA 25) FORM 9 List of Applications for Inclusion
ANNEXURE 5.8 (CHAPTER V , PARA 25) FORM 9 List of Applications for inclusion received in Form 6 Designated location identity (where Constituency (Assembly/£Parliamentary): THRISSUR Revision identity applications have been received) 1. List number@ 2. Period of applications (covered in this list) From date To date 16/11/2020 16/11/2020 3. Place of hearing * Serial number$ Date of receipt Name of claimant Name of Place of residence Date of Time of of application Father/Mother/ hearing* hearing* Husband and (Relationship)# 1 16/11/2020 ASHA PAUL NEO ANTONY (H) 403, CHEROOR, TRICHUR, , 2 16/11/2020 Uma P Ramesh Narayanan (F) 81, Variam Lane , Thrissur , , 3 16/11/2020 FARZEEN SALAM ABDUSSALAM P K (F) 3/1744 JANNATH, AKSHAYA GARDENS, CHEMBUKKAVU, , 4 16/11/2020 Sukanya Balaji Balaji K (F) Capital Gardens, Guruvayur Road, Punkunnam, , 5 16/11/2020 Abhiram P G Gopinath P S (F) Puthenvalappil House, Sitaram Mill Lane, Thrissur, , 6 16/11/2020 Arya P G Gopinath P S (F) Puthenvalappil House, Sitaram Mill Lane, Thrissur, , 7 16/11/2020 Bhuvana Vimal Vimal K V (F) 0/340 Karayil, Patturaikkal, Thrissur, , 8 16/11/2020 GOPINATHAN BHASKARA MENON (F) PALAKKAL HOUSE, PRIYA BHASKARA MENON VIHAR, AYYANTHOLE, , 9 16/11/2020 LAKSHMI GOPINATHAN (H) PALAKKAL HOUSE, PRIYA GOPINATHAN VIHAR, AYYANTHOLE, , 10 16/11/2020 USHAKUMARI M ARUN (H) KOMARATH HOUSE, OLARIKKARA, THRISSUR, , 11 16/11/2020 Mariya Paul P J (H) 49/244 Palanthingal, S M Lane, Trissur, , 12 16/11/2020 Paul P J Mariya Francis . (W) 49/24 Palathingal house, S M Lane, Pullazhy P O, Trissur, , 13 16/11/2020 SUDEEP M PREMA (M) MANAYATH HOUSE, YOUTH CORNER SWARALAYA ST, THRISSUR, , 14 16/11/2020 Biju Gopinath Gopinath S (F) Athullya, Temple Road, Poothole P O, Thrissur , , 15 16/11/2020 Arjun Krishnan A Anantharaman 20/245 Amma Nivas, Adiyat Sivashanmughan (F) Lane, Poothole P O, Thrissur, , 16 16/11/2020 Veena Joyson Joyson .