Puff Adder Bite in Ireland
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Snake Charming and the Exploitation of Snakes in Morocco
Snake charming and the exploitation of snakes in Morocco J UAN M. PLEGUEZUELOS,MÓNICA F ERICHE,JOSÉ C. BRITO and S OUMÍA F AHD Abstract Traditional activities that potentially threaten bio- also for clothing, tools, medicine and pets, as well as in diversity represent a challenge to conservationists as they try magic and religious activities (review in Alves & Rosa, to reconcile the cultural dimensions of such activities. ). Vertebrates, particularly reptiles, have frequently Quantifying the impact of traditional activities on biodiver- been used for traditional medicine. Alves et al. () iden- sity is always helpful for decision making in conservation. In tified reptile species ( families, genera) currently the case of snake charming in Morocco, the practice was in- used in traditional folk medicine, % of which are included troduced there years ago by the religious order the on the IUCN Red List (IUCN, ) and/or the CITES Aissawas, and is now an attraction in the country’s growing Appendices (CITES, ). Among the reptile species tourism industry. As a consequence wild snake populations being used for medicine, % are snakes. may be threatened by overexploitation. The focal species for Snakes have always both fascinated and repelled people, snake charming, the Egyptian cobra Naja haje, is undergo- and the reported use of snakes in magic and religious activ- ing both range and population declines. We estimated the ities is global (Alves et al., ). The sacred role of snakes level of exploitation of snakes based on field surveys and may be related to a traditional association with health and questionnaires administered to Aissawas during – eternity in some cultures (Angeletti et al., ) and many , and compared our results with those of a study con- species are under pressure from exploitation as a result ducted years previously. -

An in Vivo Examination of the Differences Between Rapid
www.nature.com/scientificreports OPEN An in vivo examination of the diferences between rapid cardiovascular collapse and prolonged hypotension induced by snake venom Rahini Kakumanu1, Barbara K. Kemp-Harper1, Anjana Silva 1,2, Sanjaya Kuruppu3, Geofrey K. Isbister 1,4 & Wayne C. Hodgson1* We investigated the cardiovascular efects of venoms from seven medically important species of snakes: Australian Eastern Brown snake (Pseudonaja textilis), Sri Lankan Russell’s viper (Daboia russelii), Javanese Russell’s viper (D. siamensis), Gaboon viper (Bitis gabonica), Uracoan rattlesnake (Crotalus vegrandis), Carpet viper (Echis ocellatus) and Puf adder (Bitis arietans), and identifed two distinct patterns of efects: i.e. rapid cardiovascular collapse and prolonged hypotension. P. textilis (5 µg/kg, i.v.) and E. ocellatus (50 µg/kg, i.v.) venoms induced rapid (i.e. within 2 min) cardiovascular collapse in anaesthetised rats. P. textilis (20 mg/kg, i.m.) caused collapse within 10 min. D. russelii (100 µg/kg, i.v.) and D. siamensis (100 µg/kg, i.v.) venoms caused ‘prolonged hypotension’, characterised by a persistent decrease in blood pressure with recovery. D. russelii venom (50 mg/kg and 100 mg/kg, i.m.) also caused prolonged hypotension. A priming dose of P. textilis venom (2 µg/kg, i.v.) prevented collapse by E. ocellatus venom (50 µg/kg, i.v.), but had no signifcant efect on subsequent addition of D. russelii venom (1 mg/kg, i.v). Two priming doses (1 µg/kg, i.v.) of E. ocellatus venom prevented collapse by E. ocellatus venom (50 µg/kg, i.v.). B. gabonica, C. vegrandis and B. -

Snakes of Durban
SNakes of durban Brown House Snake Herald Snake Non - venomous Boaedon capensis Crotaphopeltis hotamboeia Often found near human habitation where they Also referred to as the Red-lipped herald. hunt rodents, lizards and small birds. This nocturnal (active at night) snake feeds They are active at night and often collected mainlyly on frogs and is one of the more common for the pet trade. snakes found around human dwellings. SPOTTED BUSH Snake Eastern Natal Green Snake Southern Brown Egg eater Philothamnus semivariegatus Philothamnus natalensis natalensis Dasypeltis inornata Probably the most commonly found snake in This green snake is often confused with the This snake has heavily keeled body scales and urban areas. They are very good climbers, Green mamba. This diurnal species, (active during is nocturnal (active at night) . Although harmless, often seen hunting geckos and lizards the day) actively hunts frogs and geckos. they put up an impressive aggression display, in the rafters of homes. Max length 1.1 metres. with striking and open mouth gaping. Can reach This diurnal species (active during the day) over 1 metre in length and when they are that big is often confused with the Green mamba. they can eat chicken eggs. Habitat includes Max length 1.1 metres. grasslands, coastal forests and it frequents suburban gardens where they are known to enter aviaries in search of eggs. night adder Causus rhombeatus A common snake often found near ponds and dams because they feed exclusively on amphibians. They have a cytotoxic venom and bite symptoms will include pain and swelling. Max length 1 metre. -

RJHS 6(2).Cdr
Management of snakebite victims Ayinbuomwan et al. Management of snakebite victims using low dose antisnake venom in a tertiary hospital in Southern Nigeria: A 5-year Retrospective study *Ayinbuomwan A.S.1,2, Opadeyi A.O.1,2, and Isah A.O.1,2 Abstract Objective: Antisnake venom (ASV) is a specific antidote for the management of snake bite envenomations. This study profiled the treatment and outcome of adult snake bite victims managed using low dose antisnake venom. Methods: This was a 5-year retrospective study that involved all adult patients who presented in University of Benin Teaching Hospital, Benin City, Nigeria, with a history of snake bite. Information obtained were demographic characteristics, clinical features, and administered treatment per established. All patients with a diagnosis of snake bite envenomation were administered ASV. Results: Sixty patients were seen during the study period, 35(58.3%) males, 25(41.7%) females with a mean age was 34.7±13.3. The mean time from bite to presentation was 14.67±14.05 hours with range of 1- 48 hours. Twenty patients (33.3%) had snake bite envenomations, of these eleven (57.9%) were managed and discharged after administration of 30 to 40 mls of polyvalent ASV. The mean dose of PASV used was 3.9 ± 2.0 vials. The most encountered clinical indication for ASV administration was progressive painful swelling. No death was recorded throughout this period studied. Conclusion: Adoption of the low dose regimen in the management of snake bite envenomations may be as effective as the traditional high dose regimen. -

Snake and Lizards of Minnesota
SNAKES AND LIZARDS OF MINNESOTA TABLE OF CONTENTS Acknowledgments . 4 Introduction . 6 Key to Minnesota’s Snakes . 24 Common Gartersnake . 26 Common Watersnake . 28 DeKay’s Brownsnake . 30 Eastern Hog‑nosed Snake . 32 Gophersnake . 34 Lined Snake . 36 Massasauga . 38 Milksnake . 40 North American Racer . 42 Plains Gartersnake . 44 Plains Hog‑nosed Snake . 46 Red‑bellied Snake . 48 Ring‑necked Snake . 50 Smooth Greensnake . 52 Timber Rattlesnake . 54 Western Foxsnake . 56 Western Ratsnake . 58 Key to Minnesota’s Lizards . 61 Common Five‑lined Skink . .. 62 Prairie Skink . 64 Six‑lined Racerunner . 66 Glossary . 68 Appendix . 70 Help Minnesota’s Wildlife! . 71 Cover photos: Timber rattlesnakes photograph by Barb Perry . Common five‑lined skink photograph by Carol Hall . Left: Park naturalist holding gophersnake . Photograph by Deborah Rose . ACKNOWLEDGMENTS Text Rebecca Christoffel, PhD, Contractor Jaime Edwards, Department of Natural Resources (DNR) Nongame Wildlife Specialist Barb Perry, DNR Nongame Wildlife Technician Snakes and Lizards Design of Minnesota Creative Services Unit, DNR Operation Services Division Editing Carol Hall, DNR Minnesota Biological Survey (MBS), Herpetologist Liz Harper, DNR Ecological and Water Resources (EWR), Assistant Central Regional Manager Erica Hoagland, DNR EWR, Nongame Wildlife Specialist Tim Koppelman, DNR Fish and Wildlife, Assistant Area Wildlife Manager Jeff LeClere, DNR, MBS, Animal Survey Specialist John Moriarity, Senior Manager of Wildlife, Three Rivers Park District Pam Perry, DNR, EWR, Nongame Wildlife Lake Specialist (Retired) This booklet was funded through a State Wildlife Grant and the Nongame Wildlife Program, DNR Ecological and Water Resources Division . Thank you for your contributions! See inside back cover . ECOLOGICAL AND WATER RESOURCES INTRODUCTION is understandable in Minnesota, spend most of the active season . -

Puff Adder Very Dangerous
PUFF ADDER VERY DANGEROUS Adders are abundant and occur in, or close to, most major cities in southern Africa. They account for many of the snakebites serious enough to require medical attention – the majority, in many regions, the work of the Puff Adder. Most adders are short and stubby, with large erectile fangs in the front of the mouth. When not in use, the fangs are folded back within their sheaths against the roof of the mouth. They have keeled scales, those on the head and on the body similar in size. Night adders (Causus spp.) are generally less stubby and their heads are not as triangular as those of other adders. They have smooth scales, their head scales larger than their body scales. Night adders have shorter fangs than other adders and the longest venom glands (relative to body size) of all snakes. Adder venoms are predominantly cytotoxic or cell-destroying, i.e. they are responsible for the destruction of blood vessels and tissue. Symptoms are localized and bites are often extremely painful, followed by severe swelling as a result of internal bleeding and, in some cases, blistering and death of tissue. This, coupled with secondary infection, may even make amputation necessary. Bites from small adder species, although painful and unpleasant, are usually not as serious. Length: Adults average 90 cm in South Africa, but may reach 1,4 m. In Kenya specimens of over 1,8 m have been recorded, making this Africa’s largest adder. Scale count: The dorsal scales are keeled with 29–41 rows at midbody, 123–147 ventral scales and 14– 38 paired subcaudals. -

THE PUFF ADDER (BITIS ARIETANS) J.L. CLOUDSLEY-THOMPSON Department of Biology (Medawar Building), University College, University
British Herpetological Society Bulletin, No. 26, 1988. THE PUFF ADDER (BITIS ARIETANS) J.L. CLOUDSLEY-THOMPSON Department of Biology (Medawar Building), University College, University of London, Gower Street, London WCIE 6BT The Puff Adder (Bitis arietans) is one of the largest of the African vipers and probably the species most frequently seen by travellers in that continent. It receives its English name from the habit of inflating its body and hissing loudly when disturbed. The sound is produced both when the breath is inhaled as well as during exhalation. This behaviour is characteristic of all true vipers, but is particularly evident in the case of the Puff Adder. Unlike the Gaboon Viper (Bitis gabonica), which is a forest snake, the Puff Adder inhabits subdeserts and savannas, and is also to be found in mountainous regions. Except in rain forests, Puff Adders are widespread southward to the Cape from Morocco in the west and the Sudan in the east. They occur as near to Khartoum as Jebel Aulia. This is their northernmost limit in Sudan, but they range also into western and southern Arabia. Puff Adders may exceed 1.4m in length, and have a girth of 25cm. Although they do not attain the weight of a full-grown Gaboon Viper they are, nevertheless, formidable snakes. There may be considerable variation in the coloration of Puff Adders. In some specimens, the chevrons are sooty black and the crescents cream coloured while, in others, the chevrons are dark brown or grey and the crescents dull buff. The blotched pattern of dark chevrons separated by yellow crescents (Plate 1) is cryptic. -

Wildlife Population, Structure and Reproduction Based on Hunters' Returns to a Bush Meat Market in Abeokuta, Ogun State, Niger
541 Advances in Forestry Science Original Article Wildlife population, structure and reproduction based on hunters’ returns to a bush meat market in Abeokuta, Ogun state, Nigeria Muideen Alade Yisau¹*Israel Oluyinka Oloyede Osunsina¹*Samuel Akinyele Onadeko¹ ¹ Department of Forestry and Wildlife Management, College of Environmental Resources Management, Federal University of Agriculture, Abeokuta, Ogun State, Nigeria. *Author for correspondence: [email protected] Received: November 2018 / Accepted: March 2019 / Published: March 2019 Abstract common scenario in Africa (Onadeko et al. 2001). In many Assessment of the population structure and reproductive countries in Africa; West Africa (Brashares et al. 2014, status based on hunters’ returns to bush meat market were Waite, 2007), Central Africa (Fa &Yuste, 2001, Rist et al. carried out in Ogun state, Nigeria. Information on animal 2008), East Africa (Kiringe et al. 2017;Lwanga 2006; species was collected before they are dissected or processed; Olupot et al. 2009; Loibooki et al. 2002; Thirgood et al. names of species, age class, sex, weight and sources. After 2007) wildlife remain the chief traditional source of protein. dissection, its reproductive status viz number of foetus and The bush meat trade is perceived as a major threat to stages of development were observed. The data collected wild animal population in the tropics. There is little covered a period of three months. The result from the study information in the literature about the organization of the showed that nine hundred and eighty-nine animals were trade, thus hindering the development of effective returned by hunters to the market within the period. The conservation policy (Guy et al. -
African Adders: Partial Characterization of Snake Venoms from Three Bitis Species of Medical Importance and Their Neutralization by Experimental Equine Antivenoms
RESEARCH ARTICLE African Adders: Partial Characterization of Snake Venoms from Three Bitis Species of Medical Importance and Their Neutralization by Experimental Equine Antivenoms Danielle Paixão-Cavalcante, Alexandre K. Kuniyoshi, Fernanda C. V. Portaro, Wilmar Dias da Silva, Denise V. Tambourgi* Immunochemistry Laboratory, Butantan Institute, São Paulo, Brazil * [email protected] Abstract Background An alarming number of fatal accidents involving snakes are annually reported in Africa and most of the victims suffer from permanent local tissue damage and chronic disabilities. En- OPEN ACCESS venomation by snakes belonging to the genus Bitis, Viperidae family, are common in Sub- Citation: Paixão-Cavalcante D, Kuniyoshi AK, Saharan Africa. The accidents are severe and the victims often have a poor prognosis due Portaro FCV, da Silva WD, Tambourgi DV (2015) to the lack of effective specific therapies. In this study we have biochemically characterized African Adders: Partial Characterization of Snake venoms from three different species of Bitis, i.e., Bitis arietans, Bitis gabonica rhinoceros Venoms from Three Bitis Species of Medical and Bitis nasicornis, involved in the majority of the human accidents in Africa, and analyzed Importance and Their Neutralization by Experimental Equine Antivenoms. PLoS Negl Trop Dis 9(2): the in vitro neutralizing ability of two experimental antivenoms. e0003419. doi:10.1371/journal.pntd.0003419 Editor: Jean-Philippe Chippaux, Institut de Methodology/Principal Findings Recherche pour le Développement, BENIN The data indicate that all venoms presented phospholipase, hyaluronidase and fibrinogen- Received: March 6, 2014 olytic activities and cleaved efficiently the FRET substrate Abz-RPPGFSPFRQ-EDDnp and – Accepted: November 15, 2014 angiotensin I, generating angiotensin 1 7. -

THE BREEDING in CAPTIVITY of the PUFF ADDER, BITIS ARIETANS ( MERREM, 1820) . By: Roberto Rosi, Via A. Nardi 3, 19100 La Spezia
-THE BREEDING -IN CAPTIVITY ----OF THE PUFF ADDER, BITIS ARIETANS ( MERREM, 1820) . By: Roberto Rosi, Via A. Nardi 3, 19100 La Spezia, Italy. Contents: Introduction - The terrarium - Lighting - Heating - Humidity - Food - Courtship - Copulation and birth - Acknowledge- ments - References. INTRODUCTION Bitis arietans is, of the large adders, the most common species of the African continent. The genus includes numerous other species (Pezzano, 1986), including small species as Bitis peringueyi. The Puff adder varies in colour of dark brown to grey with crescent-shaped, yellow marking on the back. In size the Puff adder is second to Bitis gabonica which often reaches a length of 150 cm and more. It is an animal that is found in a variety of habitats with a preference for savanna with scat tered shrubs and clumps of trees. It is also found on forest fringes, where it is sometimes found to gether with Bitis gabonica. The Puff adder is pro vided with large venom glands which help to make it one of the most-feared venomous snakes of Afri ca. This snake is perfectly coloured to become practically invisible in its surroundings. The food of the Puff adder consists mainly of small mammals and birds. The Puff adder is ovo viviparous, producing 30-50 young. THE TERRARIUM For my three specimens I use a terrarium measuring 123 Foto 1. Bitis arietans, in copula. Foto: Giancarlo Macch,avelli. 200 x 100 x 75 cm (lxdxh), which can be divided in two halves by a movable zinc partition. The frame is made of wood and eternite. The roof is made of white, non-transparant plexi-glass. -
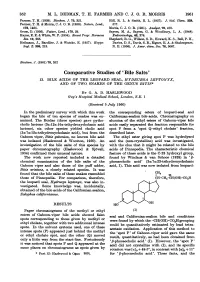
Comparative Studies of 'Bile Salts' 13
352 M. L. DEDMAN, T. H. FARMER AND C. J. 0. R. MORRIS 1961 Farmer, T. H. (1959). Biochem. J. 73, 321. Hill, R. L. & Smith, E. L. (1957). J. biol. (Chem. 228, Farmer, T. H. & Morris, C. J. 0. R. (1956). Nature, Lond., 577. 178, 1465. Morris, C. J. 0. R. (1951). Analy8t, 76, 470. Gross, D. (1956). Nature, Lond., 178, 29. Sayers, M. A., Sayers, G. & Woodbury, L. A. (1948). Hayes, E. E. & White, W. F. (1954). Recent Progr. Hormone Endocrinology, 42, 378. Res. 10, 265. Shepherd, R. G., Wilson, S. D., Howard, K. S., Bell, P. H., Heilmann, J., Barollier, J. & Watzke, E. (1957). Hoppe- Davies, D. S., Davis, S. B., Eigner, E. A. & Shakespeare, Seyl. Z. 30, 219. N. E. (1956). J. Amer. chem. Soc. 78, 5067. Biochem. J. (1961) 78, 352 Comparative Studies of 'Bile Salts' 13. BILE ACIDS OF THE LEOPARD SEAL, HYDRURGA LEPTONYX, AND OF TWO SNAKES OF THE GENUS BITIS* BY G. A. D. HASLEWOOD Guy'8 Ho8pital Medical School, London, S.E. 1 (Received 5 July 1960) In the preliminary survey with which this work the corresponding esters of leopard-seal and began the bile of ten species of snakes was ex- Californian-sealion bile acids. Chromatography on amined. The Boidae (three species) gave pytho- alumina of the ethyl esters of Gaboon-viper bile cholic lactone (3cc: 12a: 16ac-trihydroxycholanic acid acids easily separated the fraction responsible for lactone), six other species yielded cholic acid spot P from a 'spot Q-ethyl cholate' fraction, (3x:7a:12x-trihydroxycholanic acid), but from the described later. -

Snakes, People, and Spirits, Volume One
Snakes, People, and Spirits, Volume One Snakes, People, and Spirits, Volume One: Traditional Eastern Africa in its Broader Context By Robert Hazel Snakes, People, and Spirits, Volume One: Traditional Eastern Africa in its Broader Context By Robert Hazel This book first published 2019 Cambridge Scholars Publishing Lady Stephenson Library, Newcastle upon Tyne, NE6 2PA, UK British Library Cataloguing in Publication Data A catalogue record for this book is available from the British Library Copyright © 2019 by Robert Hazel All rights for this book reserved. No part of this book may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior permission of the copyright owner. ISBN (10): 1-5275-3767-6 ISBN (13): 978-1-5275-3767-5 To Professor Jean-Claude Muller, recently deceased, whose commitment to African studies and comparative anthropology was outstanding. His on- going support and encouragement enabled the author to undertake and carry out this wide-ranging research programme. TABLE OF CONTENTS Acknowledgements ................................................................................... xii List of Illustrations ................................................................................... xiv Introduction ............................................................................................... xv Part I: Prolegomena Chapter 1.1 .................................................................................................