A Case of Abdominal Nephrectomy for Renal
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

What a Difference a Delay Makes! CT Urogram: a Pictorial Essay
Abdominal Radiology (2019) 44:3919–3934 https://doi.org/10.1007/s00261-019-02086-0 SPECIAL SECTION : UROTHELIAL DISEASE What a diference a delay makes! CT urogram: a pictorial essay Abraham Noorbakhsh1 · Lejla Aganovic1,2 · Noushin Vahdat1,2 · Soudabeh Fazeli1 · Romy Chung1 · Fiona Cassidy1,2 Published online: 18 June 2019 © This is a U.S. Government work and not under copyright protection in the US; foreign copyright protection may apply 2019 Abstract Purpose The aim of this pictorial essay is to demonstrate several cases where the diagnosis would have been difcult or impossible without the excretory phase image of CT urography. Methods A brief discussion of CT urography technique and dose reduction is followed by several cases illustrating the utility of CT urography. Results CT urography has become the primary imaging modality for evaluation of hematuria, as well as in the staging and surveillance of urinary tract malignancies. CT urography includes a non-contrast phase and contrast-enhanced nephrographic and excretory (delayed) phases. While the three phases add to the diagnostic ability of CT urography, it also adds potential patient radiation dose. Several techniques including automatic exposure control, iterative reconstruction algorithms, higher noise tolerance, and split-bolus have been successfully used to mitigate dose. The excretory phase is timed such that the excreted contrast opacifes the urinary collecting system and allows for greater detection of flling defects or other abnormali- ties. Sixteen cases illustrating the utility of excretory phase imaging are reviewed. Conclusions Excretory phase imaging of CT urography can be an essential tool for detecting and appropriately characterizing urinary tract malignancies, renal papillary and medullary abnormalities, CT radiolucent stones, congenital abnormalities, certain chronic infammatory conditions, and perinephric collections. -
Laparoscopic Nephrectomy
Laparoscopic Nephrectomy Information for Patients This leaflet explains: What is a Nephrectomy? ............................................................................................. 2 Why do I need a nephrectomy? ................................................................................... 3 What are the risks and side effects of laparoscopic nephrectomy? ............................. 3 Occasional risks ....................................................................................................... 3 Rare risks ................................................................................................................. 3 Very Rare Risks ....................................................................................................... 3 Before the operation .................................................................................................... 4 Day of your operation .................................................................................................. 4 How long will the operation take? ................................................................................ 4 After the operation ....................................................................................................... 4 Going home ................................................................................................................. 5 At home ....................................................................................................................... 5 Contacts ..................................................................................................................... -

Pyelography in Infants
Arch Dis Child: first published as 10.1136/adc.9.50.119 on 1 April 1934. Downloaded from PYELOGRAPHY IN INFANTS BY W. E. UNDERWOOD, F.R.C.S., Chief Assistant to a Surgical Unit, St. Bartholomew's Hospital. Pyelography in infants is an examination which is essential under certain circumstances, and from it valuable facts may often be obtained which would be undiscovered without this specialized form of investigation. Hitherto the examination has been surrounded by difficulties of such a nature that it is often unsuccessful and the child is submitted to discomfort without result. The object of this paper is to bring forward certain notes on cases where pyelography has been indicated. The observations from a series of sixteen cases have led to the development of a method whereby good pyelograms have been obtained with certainty. Instrumental pyelography in infancy is a procedure not to be advised lightheartedly, but there are occasions where the indications are definite and adequate: in these cases the anticipation of possible information to be gained justifies submitting the infants to what constitutes a major examination. In this series are cases of urinary infection resistant to the usual medical treatment, of renal pain, of renal calculi, and cases of congenital malformation http://adc.bmj.com/ of the urinary tract similar to those described by Poynton and Sheldon'. The term pyelography is used here for brevity rather than accuracy, for it embraces a complete investigation of the urinary tract, including ureterography. Methods of pyelography.-The choice lies between intravenous and on September 30, 2021 by guest. -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

Development of the ICD-10 Procedure Coding System (ICD-10-PCS)
Development of the ICD-10 Procedure Coding System (ICD-10-PCS) Richard F. Averill, M.S., Robert L. Mullin, M.D., Barbara A. Steinbeck, RHIT, Norbert I. Goldfield, M.D, Thelma M. Grant, RHIA, Rhonda R. Butler, CCS, CCS-P The International Classification of Diseases 10th Revision Procedure Coding System (ICD-10-PCS) has been developed as a replacement for Volume 3 of the International Classification of Diseases 9th Revision (ICD-9-CM). The development of ICD-10-PCS was funded by the U.S. Centers for Medicare and Medicaid Services (CMS).1 ICD-10- PCS has a multiaxial seven character alphanumeric code structure that provides a unique code for all substantially different procedures, and allows new procedures to be easily incorporated as new codes. ICD10-PCS was under development for over five years. The initial draft was formally tested and evaluated by an independent contractor; the final version was released in the Spring of 1998, with annual updates since the final release. The design, development and testing of ICD-10-PCS are discussed. Introduction Volume 3 of the International Classification of Diseases 9th Revision Clinical Modification (ICD-9-CM) has been used in the U.S. for the reporting of inpatient pro- cedures since 1979. The structure of Volume 3 of ICD-9-CM has not allowed new procedures associated with rapidly changing technology to be effectively incorporated as new codes. As a result, in 1992 the U.S. Centers for Medicare and Medicaid Services (CMS) funded a project to design a replacement for Volume 3 of ICD-9-CM. -
Extraction of Kidney Via Suprapubic Or Inguinal Incision in Total Laparoscopic Donor Nephrectomy
LESS Original Article Laparosc Endosc Surg Sci 2019;26(1):15-18 DOI: 10.14744/less.2019.69772 Extraction of kidney via suprapubic or inguinal incision in total laparoscopic donor nephrectomy 1 1 2 1 Fatih Sümer, Ersin Gündoğan, Neslihan Altunkaya, Mehmet Can Aydın, 1 1 1 1 Sertaç Usta, Sait Murat Doğan, Turgut Pişkin, Cüneyt Kayaalp 1Department of General Surgery, Inönü University Faculty of Medicine, Malatya, Turkey 2Department of Anesthesia, Inonu University Faculty of Medicine, Malatya, Turkey ABSTRACT Introduction: The objective of this study was to investigate the results of the first 48 patients who underwent total laparoscopic transperitoneal donor nephrectomy at a single institution and to present the impact of the kidney extraction site on ischemia time. Materials and Methods: The study included patients who underwent kidney donor surgery between February 2017 and December 2018. Evaluation of the kidney transplantation candidates was performed by the kidney transplantation council. A total of 4 trocars were used for a right-side nephrectomy, and 3 trocars were used for a left-side nephrectomy. The kidneys were extracted through a suprapubic incision in the first 18 cases and through the inguinal region in the last 30 cases. A comparison was made of the demographic charac- teristics and the intraoperative and postoperative results of the 2 groups. Results: Of the study patients, 30 were female and 18 were male, with a mean age of 48.0±9.6 years (range: 30–71 years). All of the patients underwent a total laparoscopic transperitoneal donor nephrectomy. Four patients underwent a right-side nephrectomy and 44 underwent a left-side nephrectomy. -

Complications of Urologic Surgery Acknowledgement
Complications of Urologic Surgery Jay D. Raman, MD, FACS Professor and Chief of Urology Penn State Health Milton S. Hershey Medical Center @urojdr Acknowledgement • J. Kellogg Parsons, MD, MHS, FACS – Professor and Endowed Chair – Moores Comprehensive Cancer Center – UC San Diego Health System © 2018 AMERICAN UROLOGICAL ASSOCIATION. ALL RIGHTS RESERVED. Disclosures • MDxHealth – Study site investigator – urine biomarker trial • Urogen Pharma Ltd – Study site investigator – Olympus trial – Strategic advisor board • American Kidney Stone Management (AKSM) – Stock ownership Resources • AUA Guidelines • AUA Core Curriculum • AUA SASP Questions • AUA Updates • Contemporary or significant publications © 2018 AMERICAN UROLOGICAL ASSOCIATION. ALL RIGHTS RESERVED. Outline (Potpourri of topics) • Nerve injury • Positional • Intra‐operative • Bowel injury • General MIS presentation • Rectal • Air embolism (MIS) Outline (Potpourri of topics) • Venous thromboembolism (VTE) • Rhabdomyolysis • Stone Surgery • Ureteroscopy (URS) • Shock wave lithotripsy (SWL) © 2018 AMERICAN UROLOGICAL ASSOCIATION. ALL RIGHTS RESERVED. Outline (Potpourri of topics) • Nerve injury • Positional • Intra‐operative • Bowel injury • General MIS presentation • Rectal • Air embolism (MIS) Positional Nerve Injury • Presentation – Immediately post‐operatively with deficits in the affected nerve distribution • Paresthesias (numbness/tingling) – sensory • Weakness – motor • Risk factors: – Improper positioning and padding – Obesity – Prolonged operative duration Mills JT et al. -

Supplemental Information
ARTICLE Supplemental Information SUPPLEMENTAL TABLE 3 Codes Used for Building Normal and Hydronephrosis Cohorts: Associated Diagnostic Codes (For Inclusion or Exclusion) Code Description Hydroureteronephrosis 591 Hydronephrosis 753.29 Other obstructive defects of renal pelvis and ureter 593.5 Hydroureter 753.22 Congenital obstruction of UVJ VUR 593.7 VUR 593.70 VUR unspecified or without reflux nephropathy 593.71 VUR with reflux nephropathy, unilateral 593.72 VUR with reflux nephropathy, bilateral 593.73 Other VUR with reflux nephropathy NOS Obstruction 593.3 Stricture or kinking of ureter 599.6 Urinary obstruction, unspecified 599.69 Urinary obstruction NOS UPJO 753.2 Unspecified obstructive defect of renal pelvis and ureter 753.21 Congenital obstruction of the UPJ 753.29 Other obstructive defect of renal pelvis and ureter UVJ obstruction 753.22 Congenital obstruction of the UVJ Ureterocele 753.23 Congenital ureterocele PUV or urethral atresia 753.6 Atresia and stenosis of urethra and bladder neck, includes PUVs NOS, not otherwise specified; UPJ, ureteropelvic junction; UVJ, ureterovesical junction. PEDIATRICS Volume 142, number 1, July 2018 1 SUPPLEMENTAL TABLE 4 Codes Used for Building Normal and Hydronephrosis Cohorts: Urological Surgical Codes for Exclusion in Building Normal Cohort CPT ICD-9 Description Pyeloplasty 50544 — Laparoscopy, surgical; pyeloplasty 50400 55.87 Pyeloplasty 50405 — Complicated pyeloplasty; secondary or congenital 50740 55.86 Ureteropyelostomy, anastomosis of ureter and renal pelvis 50750 — Ureterocalycostomy, -
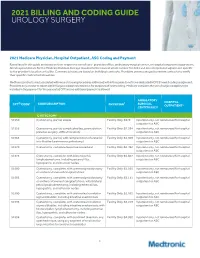
2021 Billing and Coding Guide Urology Surgery
2021 BILLING AND CODING GUIDE UROLOGY SURGERY 2021 Medicare Physician, Hospital Outpatient, ASC Coding and Payment Rates listed in this guide are based on their respective site of care- physician office, ambulatory surgical center, or hospital outpatient department. All rates provided are for the Medicare National Average rounded to the nearest whole number for 2021 and do not represent adjustment specific to the provider's location or facility. Commercial rates are based on individual contracts. Providers are encouraged to review contracts to verify their specific contracted allowables. Medtronic products used associated with wound closure procedures addressed within this guide do not have dedicated HCPCS1 level II coding assignment. Providers may choose to report A4649 Surgical supply; miscellaneous for purposes of cost tracking. Medicare considers the use of surgical supplies to be included in the payment for the associated CPT and no additional payment is allowed. AMBULATORY HOSPITAL ® 2 CODE DESCRIPTION 3 SURGICAL CPT CODE PHYSICIAN OUTPATIENT4 CENTER (ASC)4 CYSTECTOMY 51550 Cystectomy, partial; simple Facility Only: $979 Inpatient only, not reimbursed for hospital outpatient or ASC 51555 Cystectomy, partial; complicated (eg, postradiation, Facility Only: $1,284 Inpatient only, not reimbursed for hospital previous surgery, difficult location) outpatient or ASC 51565 Cystectomy, partial, with reimplantation of ureter(s) Facility Only: $1,309 Inpatient only, not reimbursed for hospital into bladder (ureteroneocystostomy) outpatient -
Having an Open Partial Nephrectomy
Having an open partial nephrectomy UHB is a no smoking Trust Introduction It is essential that you read this booklet carefully. It is important that you understand the operation and its effects on you. If there are any areas that are not clear or there are questions you need answering, the urology nurse specialists are there for you to talk to. Their telephone numbers at the back of this booklet so you can contact them. If you have not had contact with a specialist nurse, then they can be contacted on 0121 371 6926 (answer machine available). They will be able to discuss the operation with you and answer any of your initial questions. The specialist nurses are available to you after you are discharged. If you have any questions or concerns, please feel free to call them. They are there to help you through the whole process. ’Buddy’` system No matter how many leaflets and booklets you will read discussing this operation, sometimes it is helpful to talk to a patient who has undergone this operation. If you feel that you would like to talk to one of our patients, please ask your specialist nurse to put you in contact with someone. All ’Buddies‘ have volunteered their services to help other patients through this process. Early-stage kidney cancer If you have been diagnosed with an early-stage kidney cancer, surgery is usually done with the aim of curing the cancer. Occasionally, additional treatments are given to help reduce the risks of it coming back. 2 | PI20_1333_03 Having an open partial nephrectomy What is a partial nephrectomy? A partial nephrectomy is an operation to treat small kidney cancers (cancer that has not spread outside the kidney). -

Nephrectomy (Removal of the Kidney)
Nephrectomy (Removal of the Kidney) Kidney cancer is a common malignancy with over 30,000 patients afflicted in the United States per year. The incidence of kidney cancer is increasing which is partially due to the increased use of cross-sectional imaging such as CT and MRI. At the UCSF Comprehensive Cancer Center, we provide state-of -the-art care to the entire spectrum of patients with renal cancer, from those with suspicious x-rays without a diagnosis to the care of patients with advanced or recurrent kidney cancer. Surgical removal of the cancer is the most effective form of treatment for patients whose cancer is confined to the kidney. Traditionally this has been through a procedure called radical nephrectomy. Radical nephrectomy is an open surgical procedure performed through an abdominal or flank incision during which the kidney, the fat surrounding the kidney and the adrenal gland or lymph nodes are removed. It's a major surgical procedure requiring a 3-6 day hospitalization depending on a number of factors. For most patients with renal cell carcinoma, this procedure can now be performed laparoscopically, through four small incisions. Laparoscpic radical nephrectomy has the advantage of less pain and quicker return to full activities after surgery. The typical hospitalization is one to two days after surgery. For patients with smaller kidney tumors (under 5 cm.), or bilateral tumors (tumors on both sides), only one kidney or preexisting kidney problems, partial nephrectomy is an equally effective cancer treatment, with the advantage of saving the non-cancerous kidney tissue. For many years, UCSF has been a pioneering institution in the safe performance of partial nephrectomy. -

ICD-10-PCS Reference Manual
ICD-10-PCS Reference Manual 3 Table of Contents Preface ............................................................................................ xi Manual organization ................................................................................................................. xi Chapter 1 - Overview ......................................................................................................... xi Chapter 2 - Procedures in the Medical and Surgical section ............................................. xi Chapter 3 - Procedures in the Medical and Surgical-related sections ............................... xi Chapter 4 - Procedures in the ancillary sections ............................................................... xii Appendix A - ICD-10-PCS definitions ................................................................................ xii Appendix B - ICD-10-PCS device and substance classification ........................................ xii Conventions used ..................................................................................................................... xii Root operation descriptions ............................................................................................... xii Table excerpts ................................................................................................................... xiii Chapter 1: ICD-10-PCS overview ......................................................... 15 What is ICD-10-PCS? .............................................................................................................