Endoscopy and Microendoscopy of the Lacrimal Drainage System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ciliary Zonule Sclera (Suspensory Choroid Ligament)
ACTIVITIES Complete Diagrams PNS 18 and 19 Complete PNS 23 Worksheet 3 #1 only Complete PNS 24 Practice Quiz THE SPECIAL SENSES Introduction Vision RECEPTORS Structures designed to respond to stimuli Variable complexity GENERAL PROPERTIES OF RECEPTORS Transducers Receptor potential Generator potential GENERAL PROPERTIES OF RECEPTORS Stimulus causing receptor potentials Generator potential in afferent neuron Nerve impulse SENSATION AND PERCEPTION Stimulatory input Conscious level = perception Awareness = sensation GENERAL PROPERTIES OF RECEPTORS Information conveyed by receptors . Modality . Location . Intensity . Duration ADAPTATION Reduction in rate of impulse transmission when stimulus is prolonged CLASSIFICATION OF RECEPTORS Stimulus Modality . Chemoreceptors . Thermoreceptors . Nociceptors . Mechanoreceptors . Photoreceptors CLASSIFICATION OF RECEPTORS Origin of stimuli . Exteroceptors . Interoceptors . Proprioceptors SPECIAL SENSES Vision Hearing Olfaction Gustation VISION INTRODUCTION 70% of all sensory receptors are in the eye Nearly half of the cerebral cortex is involved in processing visual information Optic nerve is one of body’s largest nerve tracts VISION INTRODUCTION The eye is a photoreceptor organ Refraction Conversion (transduction) of light into AP’s Information is interpreted in cerebral cortex Eyebrow Eyelid Eyelashes Site where conjunctiva merges with cornea Palpebral fissure Lateral commissure Eyelid Medial commissure (a) Surface anatomy of the right eye Figure 15.1a Orbicularis oculi muscle -

Eyelid Conjunctival Tumors
EYELID &CONJUNCTIVAL TUMORS PHOTOGRAPHIC ATLAS Dr. Olivier Galatoire Dr. Christine Levy-Gabriel Dr. Mathieu Zmuda EYELID & CONJUNCTIVAL TUMORS 4 EYELID & CONJUNCTIVAL TUMORS Dear readers, All rights of translation, adaptation, or reproduction by any means are reserved in all countries. The reproduction or representation, in whole or in part and by any means, of any of the pages published in the present book without the prior written consent of the publisher, is prohibited and illegal and would constitute an infringement. Only reproductions strictly reserved for the private use of the copier and not intended for collective use, and short analyses and quotations justified by the illustrative or scientific nature of the work in which they are incorporated, are authorized (Law of March 11, 1957 art. 40 and 41 and Criminal Code art. 425). EYELID & CONJUNCTIVAL TUMORS EYELID & CONJUNCTIVAL TUMORS 5 6 EYELID & CONJUNCTIVAL TUMORS Foreword Dr. Serge Morax I am honored to introduce this Photographic Atlas of palpebral and conjunctival tumors,which is the culmination of the close collaboration between Drs. Olivier Galatoire and Mathieu Zmuda of the A. de Rothschild Ophthalmological Foundation and Dr. Christine Levy-Gabriel of the Curie Institute. The subject is now of unquestionable importance and evidently of great interest to Ophthalmologists, whether they are orbital- palpebral specialists or not. Indeed, errors or delays in the diagnosis of tumor pathologies are relatively common and the consequences can be serious in the case of malignant tumors, especially carcinomas. Swift diagnosis and anatomopathological confirmation will lead to a treatment, discussed in multidisciplinary team meetings, ranging from surgery to radiotherapy. -

Plastic Surgery for Pigmented Hairy Naevus of the Eyelids by Excision and Masquerade Skin Graft
Brit. J. Ophthal. (I969) 53, 343 Br J Ophthalmol: first published as 10.1136/bjo.53.5.343 on 1 May 1969. Downloaded from Plastic surgery for pigmented hairy naevus of the eyelids By excision and masquerade skin graft B. HIRSHOWITZ AND D. MAHLER Department of Plastic Surgery, Rambam Government Hospital, Haifa, Israel The simultaneous excision of a lesion affecting the skin of both upper and lower eyelids carries with it the problem of skin replacement. Both aesthetic and functional require- ments will have to be met in the reconstruction. Ectropion could complicate such a repair, and loss of eyelashes would add to the disfigurement. All these aspects had to be considered in a patient with a darkly pigmented hairy naevus involving both eyelids and the surrounding skin. Case report copyright. A 15-year-old boy had a deeply pigmented hairy naevus of the upper and lower eyelids on the left side. The naevus extended to both inner and outer canthi, the eyebrow, and the temporal and cheek regions (Fig. i). The ciliary borders of both eyelids were also involved. The operation was indicated because of severe psychological disturbances engendered by this disfigurement. http://bjo.bmj.com/ F_I. i Appearance before operation ......... ..... on September 26, 2021 by guest. Protected Operative technique The naevus was almost completely excised, apart from its extension into the eyebrow. Both upper and lower eyelashes were removed together with the naevus. Care was taken not to interfere with the lacrimal punctum. Immobilization of both eyelids was attained by a continuous wire suture running intratarsally. In effect, this adaptation of eyelid margins resulted in almost a complete tarsorrhaphy. -

Anatomy of the Periorbital Region Review Article Anatomia Da Região Periorbital
RevSurgicalV5N3Inglês_RevistaSurgical&CosmeticDermatol 21/01/14 17:54 Página 245 245 Anatomy of the periorbital region Review article Anatomia da região periorbital Authors: Eliandre Costa Palermo1 ABSTRACT A careful study of the anatomy of the orbit is very important for dermatologists, even for those who do not perform major surgical procedures. This is due to the high complexity of the structures involved in the dermatological procedures performed in this region. A 1 Dermatologist Physician, Lato sensu post- detailed knowledge of facial anatomy is what differentiates a qualified professional— graduate diploma in Dermatologic Surgery from the Faculdade de Medician whether in performing minimally invasive procedures (such as botulinum toxin and der- do ABC - Santo André (SP), Brazil mal fillings) or in conducting excisions of skin lesions—thereby avoiding complications and ensuring the best results, both aesthetically and correctively. The present review article focuses on the anatomy of the orbit and palpebral region and on the important structures related to the execution of dermatological procedures. Keywords: eyelids; anatomy; skin. RESU MO Um estudo cuidadoso da anatomia da órbita é muito importante para os dermatologistas, mesmo para os que não realizam grandes procedimentos cirúrgicos, devido à elevada complexidade de estruturas envolvidas nos procedimentos dermatológicos realizados nesta região. O conhecimento detalhado da anatomia facial é o que diferencia o profissional qualificado, seja na realização de procedimentos mini- mamente invasivos, como toxina botulínica e preenchimentos, seja nas exéreses de lesões dermatoló- Correspondence: Dr. Eliandre Costa Palermo gicas, evitando complicações e assegurando os melhores resultados, tanto estéticos quanto corretivos. Av. São Gualter, 615 Trataremos neste artigo da revisão da anatomia da região órbito-palpebral e das estruturas importan- Cep: 05455 000 Alto de Pinheiros—São tes correlacionadas à realização dos procedimentos dermatológicos. -

Surgical Management of Carcinoma Ofeyelids and Periorbital Skin
Br J Ophthalmol: first published as 10.1136/bjo.63.8.578 on 1 August 1979. Downloaded from British Journal of Ophthalmology, 1979, 63, 578-585 Surgical management of carcinoma of eyelids and periorbital skin HEMANT MEHTA From the Department of Ophthalmology, Caernarvonshire and Anglesey General Hospital, Bangor, Gwynedd SUMMARY An appraisal of a personal series of 115 unselected and surgically treated cutaneous cancers of palpebral region is presented. Histological confirmation of the diagnosis and adequacy of excision was obtained for all lesions. Seven of the 8 patients with doubtful clearance were successfully treated with further surgery very soon. Complications were few, the incidence of re- operations low, and cosmetic as well as functional results were mostly satisfactory. Tumour recurred in 1 case (087%). Two patients had a poor cosmetic result. Seventy-nine cases (69%) were treated as day cases under local anaesthesia even for major repairs like full-thickness reconstruction of two-thirds of the lower eyelid and repairs with large full-thickness skin grafts of up to 20 x 55 mm by a new simple technique of graft fixation. The use of longer-acting local anaesthetics in oculoplastic surgery is described. Attention is drawn to the dangers of using direct wound closure for repair. Apart from the readily observable cosmetic blemish 2 by radiotherapy and 4 by surgery, including a that they produce malignant tumours of the skin rodent ulcer that was curetted elsewhere, having of the eyelids and periorbita differ from cutaneous been mistaken for a meibomian cyst. All excised malignancies elsewhere by their tendency to damage lesions were examined histologically for confirma- the ocular and adnexal structures either by direct tion of diagnosis and completeness of excision. -

Jemds.Com Original Research Article
Jemds.com Original Research Article ANALYSIS OF 34 CASES OF ENDONASAL ENDOSCOPIC DACRYOCYSTORHINOSTOMY- SURGICAL SUCCESS AND PATIENT SATISFACTION, A CASE SERIES, OUR EXPERIENCE N. Gopinathan Pillai1, Binu Babu2, Anjana Mary Reynolds3, Subadhra S4 1Associate Professor, Department of Otorhinolaryngology, PIMSRC, Thiruvalla. 2Assistant Professor, Department of Otorhinolaryngology, PIMSRC, Thiruvalla. 3Assistant Professor, Department of Otorhinolaryngology, PIMSRC, Thiruvalla. 4Junior Resident, Department of Otorhinolaryngology, PIMSRC, Thiruvalla. ABSTRACT BACKGROUND The conventional treatment of dacryocystitis is external dacryocystorhinostomy. Its success rate varies from 80 - 98%.1-4 But patient’s satisfaction was poor due to facial scar, disruption of medial canthus anatomy and dysfunction of lacrimal pump mechanism. Endoscopic DCR has neither facial scar nor any postoperative distortion of lacrimal pump mechanism and medial canthal anatomy. The objective of this study is to assess the surgical success rate and patient’s satisfaction after endonasal endoscopic Dacryocystorhinostomy (DCR). Study Design- This study was done at Pushpagiri Institute of Medical Sciences and Research Centre, Thiruvalla, between January 2012 and August 2016. There were 34 patients included in this study. Females are more commonly affected than males. Unilateral cases are more than bilateral cases. Their age ranges from 13 - 83 years. Mean age is 35 years. MATERIALS AND METHODS Patients presented with epiphora or swelling below the medial canthus of eye with or without pain, mucopurulent regurgitation from the lacrimal sac into the eye on pressing the swelling. Five patients had concomitant deviated nasal septum, for which septoplasty was done along with DCR. The patency of nasolacrimal duct was assessed by syringing and diagnostic nasal endoscopy. RESULTS The success rate is comparable to other studies of endonasal DCR. -

Diagnostic Imaging of the Nasolacrimal Drainage System. Part
REVIEW ARTICLES e-ISSN 1643-3750 © Med Sci Monit, 2014; 20: 628-638 DOI: 10.12659/MSM.890098 Received: 2013.11.27 Accepted: 2014.01.16 Diagnostic imaging of the nasolacrimal drainage Published: 2014.04.17 system. Part I. Radiological anatomy of lacrimal pathways. Physiology of tear secretion and tear outflow Authors’ Contribution: ABCDEFG 1 Artur Maliborski 1 Department of Medical Radiology, Military Institute of Medicine, Warsaw, Poland Study Design A ABCG 2 Radosław Różycki 2 Department of Ophthalmology, Military Institute of Medicine, Warsaw, Poland Data Collection B Statistical Analysis C Data Interpretation D Manuscript Preparation E Literature Search F Funds Collection G Corresponding Author: Artur Maliborski, e-mail: [email protected] Source of support: Departmental sources Excessive watering of the eye is a common condition in ophthalmological practice. It may be the result of ex- cessive production of tear fluid or obstruction and insufficiency of efferent tear pathways. The differentia- tion between obstruction and insufficiency of the lacrimal pathways is still clinically questionable. In the -di agnostic process it is necessary to perform clinical tests and additional diagnostic imaging is often needed. Dacryocystography, with or without the extension of the dynamic phase or subtraction option, still remains the criterion standard for diagnostic imaging of the lacrimal obstruction. It may help to clarify the cause and exact place of the obstruction and provide information for further management, especially surgical treatment. Increasingly, new techniques are used in diagnostic imaging of the lacrimal tract, such as computed tomogra- phy, magnetic resonance, and isotopic methods. Adequate knowledge of the anatomy and physiology of the lacrimal system and the secretion and outflow of tears is the basis for proper diagnostic imaging. -
Principles and Procedure for Eye Assessment and Cleansing
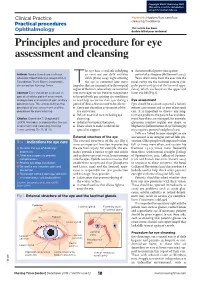
Copyright EMAP Publishing 2019 This article is not for distribution except for journal club use Clinical Practice Keywords Hygiene/Eye care/Eye cleansing/Swabbing Practical procedures This article has been Ophthalmology double-blind peer reviewed Principles and procedure for eye assessment and cleansing he eyes have a vital role in helping l Antimicrobial protection against Authors Tendai Gwenhure is clinical us carry out our daily activities potential pathogens (McDermott, 2013). educator, Moorfields Eye Hospital NHS safely (Shaw, 2014). Light entering Tears drain away from the eyes into the Foundation Trust; Eileen Shepherd is Tthe eye is converted into nerve nasal cavity via the lacrimal puncta (sin- clinical editor, Nursing Times. impulses that are transmitted to the occipital gular punctum) (part of the lacrimal appa- region of the brain, where they are converted ratus), which are found on the upper and Abstract Eyes should be assessed as into the images we see. Patients may present lower eye lids (Fig 1). part of a holistic patient assessment to hospital with pre-existing eye conditions and eye care is an essential part of daily or need help to care for their eyes during a Eye assessment personal care. This article outlines the period of illness. Nurses need to be able to: Eyes should be assessed as part of a holistic principles of eye assessment and the l Carry out a baseline assessment of the patient assessment and as part of personal procedure for eye cleansing. eye and vision; care. It is important to discuss any long- l Deliver essential care including eye term eye problems the patient has and docu- Citation Gwenhure T, Shepherd E cleansing; ment how these are managed; for example, (2019) Principles and procedure for eye l Administer topical therapies; glaucoma requires regular eye drops, or assessment and cleansing. -

Anatomy 2-Orbicularis
INJECTABLES ANATOMY www.aestheticmed.co.uk Eye for detail Dr Sotirios Foutsizoglou on understanding the anatomy and function of the orbicularis oculi 60 Aesthetic Medicine • March 2017 INJECTABLES www.aestheticmed.co.uk ANATOMY he orbicularis oculi forms part of the muscles of Its lateral fibres cause a radiating folding of the skin facial expression. It develops from mesenchyme which may develop into the permanent “crow’s feet” of the second pharyngeal arch and supplied by wrinkles of older age. its nerve, the seventh cranial nerve (CN VII). The It assists the flow of lacrimal fluid (tears) by bringing the orbicularis oculi is the sphincter of the eyelid and lids together, closing the palpebral fissure in a lateral to Tresides almost entirely within a fibromuscular sheet, best medial direction, gently pushing the lacrimal secretions known as the superficial musculoaponeurotic system. near the lacrimal caruncle in the lacrimal lake at the Its fibres attach primarily to the medial orbital margins medial angle of the eye. and medial palpebral ligament (medial canthal tendon), It is involved in lacrimal drainage. Contraction of the sweeping in concentric circles around the orbital margin pretarsal muscle shortens and closes the canaliculi, and eyelids. Laterally, the muscle fibres do not have a direct whereas the preseptal muscle pulls on the lacrimal bony attachment, but are stabilized to the orbital rim by a diaphragm, resulting in a negative pressure within the ligamentous connection at the lateral canthus. lacrimal sac. Upon relaxation, tears pass to the nasal cavity through the nasolacrimal duct (Fig 1).2 Primary actions of the Orbicularis Oculi The orbicularis oculi (palpebral part) is the main protractor Anatomy of the Orbicularis Oculi of the eyelids. -

2009 CPT Codes of Interest to Ophthalmology 65091 - 68899 Eye Codes
2009 CPT codes of interest to Ophthalmology 65091 - 68899 Eye Codes 65091 - 65290 Eye Ball 65091 - 65114 Removal Of Eye 65091 Evisceration, ocular contents; w/o implant 65093 Evisceration, ocular contents; w/ implant 65101 Enucleation, eye; w/o implant 65103 Enucleation, eye; w/ implant, muscles not attached 65105 Enucleation, eye; w/ implant, muscles attached 65110 Exenteration, orbit 65112 Exenteration, orbit; w/ therapeutic removal, bone 65114 Exenteration, orbit; w/ muscle/myocutaneous flap 65125 - 65175 Secondary Implant Procedures 65125 Modification, ocular implant w/ placement/replacement of pegs 65130 Insertion, ocular implant secondary; after evisceration, scleral shell 65135 Insertion, ocular implant secondary; after enucl., muscles not attached 65140 Insertion, ocular implant secondary; after enucleation, muscles attached 65150 Reinsertion of ocular implant 65155 Reinsertion of ocular implant; w/ reinforcement 65175 Removal, ocular implant 65205 - 65265 Removal Of Foreign Body 65205 Removal, foreign body, external eye; conjunctival superficial 65210 Removal, foreign body, external eye; conjunctival embedded 65220 Removal, foreign body, external eye; corneal, w/o slit lamp 65222 Removal, foreign body, external eye; corneal, w/ slit lamp 65235 Removal, foreign body, intraocular; from anterior chamber/lens 65260 Removal, foreign body, intraocular; from posterior segment 65265 Removal, foreign body, intraocular; from posterior segment, non-magnetic extraction 65270 - 65290 Repair Of Laceration 65270 Repair, laceration; conjunctiva, -

Syndromic and Nonsyndromic Systemic Associations of Congenital Lacrimal Drainage Anomalies: a Major Review
MAJOR REVIEW Syndromic and Nonsyndromic Systemic Associations of Congenital Lacrimal Drainage Anomalies: A Major Review Mohammad Javed Ali, F.R.C.S.*† and Friedrich Paulsen, M.D.† *Govindram Seksaria Institute of Dacryology, L.V. Prasad Eye Institute, Hyderabad, India; and †Institut für Anatomie, Friedrich-Alexander-Universität Erlangen-Nürnberg, Erlangen, Germany. of 223 children in their series to have craniofacial abnormalities, Purpose: To review and summarize the syndromic, and Barnes et al.8 found 8% (10/121) of his patients had systemic nonsyndromic, and systemic associations of congenital lacrimal associations. It may therefore be helpful to review the embryo- drainage anomalies. genesis of the lacrimal system, to be able to better appreciate Methods: The authors performed a PubMed search of all their associations with multiple craniofacial syndromes. articles published in English on congenital lacrimal anomalies The lacrimal drainage system develops as a fold of ecto- (1933–2016). Patients of these articles were reviewed along derm (lacrimal lamina) along the line of cleft between the lat- with the literature of direct references to syndromes and other eral nasal and maxillary processes during the Carnegie stage systemic associations. Data reviewed included syndromic 16 of the embryonic development. The lamina separates from descriptions, systemic details, demographics, lacrimal the ectoderm to form a lacrimal cord (Carnegie stage 19). The presentations, management, and outcomes. lateral end of the cord bifurcates to form canaliculi and the other Results: Syndromic and systemic associations with end gets arranged lateral and inferior to the inferior meatal lam- congenital lacrimal drainage disorders are not known to be ina (Carnegie stage 20). -
Lacrimal Drainage Anatomy in the Japanese Population
Annals of Anatomy 223 (2019) 90–99 Contents lists available at ScienceDirect Annals of Anatomy jou rnal homepage: www.elsevier.com/locate/aanat ଝ Lacrimal drainage anatomy in the Japanese population a a,∗ b b Ma. Regina Paula Valencia , Yasuhiro Takahashi , Munekazu Naito , Takashi Nakano , c a Hiroshi Ikeda , Hirohiko Kakizaki a Department of Oculoplastic, Orbital, and Lacrimal Surgery, Aichi Medical University Hospital, 1-1 Yazako-Karimata, Nagakute, Aichi 480-1195, Japan b Department of Anatomy, Aichi Medical University, 1-1 Yazako-Karimata, Nagakute, Aichi, Japan c Department of Pathology, Aichi Medical University, 1-1 Yazako-Karimata, Nagakute, Aichi, Japan a r t i c l e i n f o a b s t r a c t Article history: Purpose: The aim of this study is to provide a comprehensive and clinically relevant review of the lacrimal Received 16 January 2019 drainage anatomy in the Japanese population. Received in revised form 29 January 2019 Methods: A thorough search on the lacrimal drainage anatomy in the Japanese population was performed Accepted 29 January 2019 using PubMed and Ichushi Web, which is managed by the Japan Medical Abstracts Society, for related studies up to December 2018. Published books on the same topic were also reviewed. Data from all Keywords: articles and book chapters were reviewed, analyzed, and incorporated in this review. Lacrimal drainage Results: This review presents the subparts of the lacrimal drainage anatomy in a chronological manner, Anatomy Japanese from proximal to distal. The location, dimensions, position or angle, histology (with some reference to the essential clinical functions and physiology of the lacrimal drainage system) are described in this review.