Psychiatric History and Overactive Bladder Symptom Severity in Ambulatory Urogynecological Patients
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

January 2021 Update
PUBLISHED JULY 08, 2021 OCTOBER/DECEMBER 2020; JANUARY 2021 UPDATE CHANGES TO THE HIGHMARK DRUG FORMULARIES Following is the update to the Highmark Drug Formularies and pharmaceutical management procedures for January 2021. The formularies and pharmaceutical management procedures are updated on a bimonthly basis, and the following changes reflect the decisions made in October, December, and January by our Pharmacy and Therapeutics Committee. These updates are effective on the dates noted throughout this document. Please reference the guide below to navigate this communication: Section I. Highmark Commercial and Healthcare Reform Formularies A. Changes to the Highmark Comprehensive Formulary and the Highmark Comprehensive Healthcare Reform Formulary B. Changes to the Highmark Healthcare Reform Essential Formulary C. Changes to the Highmark Core Formulary D. Changes to the Highmark National Select Formulary E. Updates to the Pharmacy Utilization Management Programs 1. Prior Authorization Program 2. Managed Prescription Drug Coverage (MRxC) Program 3. Formulary Program 4. Quantity Level Limit (QLL) Programs As an added convenience, you can also search our drug formularies and view utilization management policies on the Provider Resource Center (accessible via NaviNet® or our website). Click the Pharmacy Program/Formularies link from the menu on the left. Highmark Blue Cross Blue Shield Delaware is an independent licensee of the Blue Cross and Blue Shield Association. NaviNet is a registered trademark of NaviNet, Inc., which is an independent company that provides secure, web-based portal between providers and health insurance companies. IMPORTANT DRUG SAFETY UPDATES 03/31/2021 – Studies show increased risk of heart rhythm problems with seizure and mental health medicine lamotrigine (Lamictal) in patients with heart disease. -
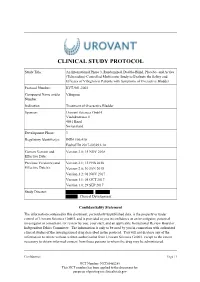
Study Protocol
CLINICAL STUDY PROTOCOL Study Title: An International Phase 3, Randomized, Double-Blind, Placebo- and Active (Tolterodine)-Controlled Multicenter Study to Evaluate the Safety and Efficacy of Vibegron in Patients with Symptoms of Overactive Bladder Protocol Number: RVT-901-3003 Compound Name and/or Vibegron Number: Indication Treatment of Overactive Bladder Sponsor: Urovant Sciences GmbH Viaduktstrasse 8 4051 Basel Switzerland Development Phase: 3 Regulatory Identifier(s): IND# 106,410 EudraCT# 2017-003293-14 Current Version and Version 3.0; 15 NOV 2018 Effective Date: Previous Version(s) and Version 2.1; 12 FEB 2018 Effective Date(s): Version 2.0; 30 JAN 2018 Version 1.2; 01 NOV 2017 Version 1.1; 05 OCT 2017 Version 1.0; 29 SEP 2017 Study Director: , , Clinical Development Confidentiality Statement The information contained in this document, particularly unpublished data, is the property or under control of Urovant Sciences GmbH, and is provided to you in confidence as an investigator, potential investigator or consultant, for review by you, your staff, and an applicable Institutional Review Board or Independent Ethics Committee. The information is only to be used by you in connection with authorized clinical studies of the investigational drug described in the protocol. You will not disclose any of the information to others without written authorization from Urovant Sciences GmbH. except to the extent necessary to obtain informed consent from those persons to whom the drug may be administered. Confidential Page | 1 NCT Number: NCT03492281 This NCT number has been applied to the document for purposes of posting on clinicaltrials.gov Clinical Study Protocol RVT-901-3003 Urovant Sciences GmbH Effective: 15 NOV 2018 SUMMARY OF CHANGES Version Location Description of Change 3.0 Global Minor typographical/formatting errors were corrected. -

Gemtesa® (Vibegron) – New Drug Approval
Gemtesa® (vibegron) – New drug approval • On December 23, 2020, Urovant Sciences announced the FDA approval of Gemtesa (vibegron), for the treatment of overactive bladder (OAB) with symptoms of urge urinary incontinence, urgency, and urinary frequency in adults. • OAB is a common condition that occurs when the bladder muscle contracts involuntarily. Over 30 million Americans are estimated to suffer from bothersome symptoms of OAB. • Gemtesa is a selective human beta-3 adrenergic receptor agonist. Activation of the beta-3 adrenergic receptor increases bladder capacity by relaxing the detrusor smooth muscle during bladder filling. • The efficacy of Gemtesa was established in a 12-week, double-blind, randomized, placebo- controlled, and active-controlled study in 1,515 patients with OAB (urge urinary incontinence, urgency, and urinary frequency). The co-primary endpoints were change from baseline in average daily number of micturitions and average daily number of urge urinary incontinence (UUI) episodes at week 12. — The change from baseline at week 12 in the average daily number of micturitions was -1.8 and -1.3 for Gemtesa and placebo, respectively (difference of -0.5, 95% CI: -0.8, -0.2; p < 0.001). — The change from baseline at week 12 in the average daily number of UUI episodes was -2.0 and -1.4 for Gemtesa and placebo, respectively (difference of -0.6, 95% CI: -0.9, -0.3; p < 0.0001). • A warning and precaution for Gemtesa is urinary retention. • The most common adverse reactions (2%) with Gemtesa use were headache, urinary tract infection, nasopharyngitis, diarrhea, nausea, and upper respiratory tract infection. • The recommended dose of Gemtesa is one 75 mg tablet orally, once daily with or without food. -

213006Orig1s000 OTHER REVIEW(S)
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 213006Orig1s000 OTHER REVIEW(S) Department of Health and Human Services Public Health Service Food and Drug Administration Center for Drug Evaluation and Research Office of Medical Policy PATIENT LABELING REVIEW Date: November 20, 2020 To: Nenita Crisostomo, RN Regulatory Project Manager Division of Urology, Obstetrics and Gynecology (DUOG) Through: LaShawn Griffiths, MSHS-PH, BSN, RN Associate Director for Patient Labeling Division of Medical Policy Programs (DMPP) Sharon Williams, MSN, BSN, RN Senior Patient Labeling Reviewer Division of Medical Policy Programs (DMPP) From: Lonice Carter, MS, RN, CNL Patient Labeling Reviewer Division of Medical Policy Programs (DMPP) Elvy Varghese, PharmD. Regulatory Review Officer Office of Prescription Drug Promotion (OPDP) Subject: Review of Patient Labeling: Patient Package Insert (PPI) Drug Name (established GEMTESA (vibegron) name): Dosage Form and Route: tablets, for oral use Application NDA 213006 Type/Number: Applicant: Urovant Sciences GmbH (Urovant) Reference ID: 4705052 1 INTRODUCTION On December 26, 2019, Urovant Sciences GmbH (Urovant) submitted for the Agency’s review an original New Drug Application (NDA)/New Molecular Entity 213006 for GEMTESA (vibegron) tablets, for oral use. The purpose of this NDA is to propose an indication for the treatment of overactive bladder with symptoms of urge urinary incontinence, urgency, and urinary frequency. This collaborative review is written by the Division of Medical Policy Programs (DMPP) and the Office of Prescription Drug Promotion (OPDP) in response to a request by the Division of Urology, Obstetrics and Gynecology (DUOG) on February 4, 2020, for DMPP and OPDP to review the Applicant’s proposed Patient Package Insert (PPI) for GEMTESA (vibegron) tablets, for oral use. -

WO 2018/224989 Al 13 December 2018 (13.12.2018) W P O PCT
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2018/224989 Al 13 December 2018 (13.12.2018) W P O PCT (51) International Patent Classification: A61K 31/519 (2006.01) A61K 31/496 (2006.01) A61K 45/06 (2006.01) A61K 31/554 (2006 .0 1) A61P 13/10 (2006.01) A61K 31/7048 (2006.01) 5 57 (2006.01) (21) International Application Number: PCT/IB20 18/054069 (22) International Filing Date: 06 June 2018 (06.06.2018) (25) Filing Language: English (26) Publication Language: English (30) Priority Data: 62/5 15,996 06 June 2017 (06.06.2017) US 62/635,146 26 February 2018 (26.02.2018) US 62/637,961 02 March 2018 (02.03.2018) US (71) Applicant: UROVANT SCIENCES GMBH [CH/CH]; CI O Vischer AG, Aeschenvorstadt 4, 405 1 Basel (CH). = (72) Inventors: PISCITELLI, Stephen C ; c/o Roivant = Sciences, Inc., 324 Blackwell Street, Suite 1220, Durham, = North Carolina 27701 (US). MUDD, Paul; c/o Roivant = Sciences, Inc., 324 Blackwell Street, Suite 1220, Durham, = North Carolina 27701 (US). (81) Designated States (unless otherwise indicated, for every — kind of national protection available): AE, AG, AL, AM, = AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, BZ, ≡ CA, CH, CL, CN, CO, CR, CU, CZ, DE, DJ, DK, DM, DO, = DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, = HR, HU, ID, IL, IN, IR, IS, JO, JP, KE, KG, KH, KN, KP, = KR, KW,KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, = MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, = OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, = TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. -

A Review of Pharmacotherapy in the Treatment of Urinary Disorders
International Journal of Innovative Research in Medical Science (IJIRMS) Volume 04, Issue 06, June 2019, https://doi.org/10.23958/ijirms/vol04-i06/672 Original article A Review of Pharmacotherapy in the Treatment of Urinary Disorders Dr Manoj G Tyagi Department of Pharmacology, KM Medical College, Mathura, Uttar Pradesh * Author for Correspondence: Dr Manoj G Tyagi; ttyagi243 @ yahoo.co.in Received 26 May 2019; Accepted 14 June 2019; Published 17 June 2019 Abstract Urinary tract infections and other related pathophysiological conditions are a plethora of ailments affecting mankind. Ailments that are as common as the urinary tract infection, uropathy, incontinence, calculi and many other disorders. With the advancement of research into newer and more potent drugs with better efficacy and lesser side effects, treatment is becoming more specific and efficacious. This review examines the recent development in the treatment of these disorders and impressive progress in the pharmacotherapy, it also gives an overview of current and future prospects of drugs for bladder disorders. Keywords: Bladder, incontinence, urinary, anti-cholinergic, disorder Introduction urine until the brain signals the bladder that the person is ready to void it[3]. A normal, healthy bladder can hold up to 16 ounces i.e Urinary tract disorders are one of the common disorders of human almost half a liter of urine comfortably for two to five hours. beings. The Urinary tract system comprises of the ureters, bladders and urethra and these are the key excretory system for not just metabolic by products, toxins and xenobiotics and always under a lot of pressure and stress[1]. -

Focus on Overactive Bladder: a Fine‐Tuned Approach to Attain Outcome Targets
Friday General Session Focus on Overactive Bladder: A Fine‐Tuned Approach to Attain Outcome Targets Scott A. MacDiarmid, MD, FRCPSC Director of the Bladder Control and Pelvic Pain Center Alliance Urology Specialists Greensboro, North Carolina Educational Objectives By completing this educational activity, the participant should be better able to: 1. Proactively evaluate and screen at‐risk individuals for overactive bladder (OAB). 2. Utilize communication strategies aimed to evaluate the impact of OAB on quality of life and educate patients on appropriate treatment options and expectations. 3. Select patients with OAB who would benefit from combination therapy to maximize efficacy and tolerability. Speaker Disclosure Dr. MacDiarmid has disclosed that he is on the advisory committee and speaker’s bureau for Allergan, Astellas, and Urovant. Supporter Disclosure This educational activity is supported by an educational grant from Astellas. It has been planned and produced by VemCo MedEd with Texas Academy of Family Physicians strictly as an accredited continuing medical education activity. 2 FACULTY AND DISCLOSURE Jointly proved by Center for Independent Healthcare Education and Vemco MedEd Supported by an educational grant from Astellas Scientific and Medical Affairs, Inc. Scott A. MacDiarmid, MD, FRCPSC Alliance Urology Specialists Clinical Associate Professor Department of Urology University of North Carolina Chapel Hill, NC Scott MacDiarmid, MD has relevant financial relationships with ineligible companies to disclose: Speaker’s Bureau: Astellas Pharm, Urovant Sciences Consultant: Astellas Pharm, Urovant Sciences, Allergan All relevant financial relationships have been mitigated. Dr. MacDiarmid does not intend to discuss the off-label use of a product. No (other) speakers, authors, planners or content reviewers have any relevant financial relationships to disclose. -

213006Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 213006Orig1s000 RISK ASSESSMENT and RISK MITIGATION REVIEW(S) Division of Risk Management (DRM) Office of Medication Error Prevention and Risk Management (OMEPRM) Office of Surveillance and Epidemiology (OSE) Center for Drug Evaluation and Research (CDER) Application Type NDA Application Number 213006 PDUFA Goal Date December 26, 2020 OSE RCM # 2019-2648 Reviewer Name Theresa Ng, PharmD, BCPS Team Leader Laura Zendel, PharmD, BCPS Deputy Division Director Cynthia LaCivita, PharmD Review Completion Date December 9, 2020 Subject Evaluation of Need for a REMS Established Name Vibegron Trade Name Gemtesa Name of Applicant Urovant Sciences Therapeutic Class Beta-3 adrenergic agonist Formulation(s) 75 mg tablet Dosing Regimen One tablet orally once daily with or without food 1 Reference ID: 4714124 Table of Contents EXECUTIVE SUMMARY ......................................................................................................................................................... 3 1 Introduction ..................................................................................................................................................................... 3 2 Background ...................................................................................................................................................................... 3 2.1 Product Information .......................................................................................................................................... -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

Appendix B - Product Name Sorted by Applicant
JUNE 2021 - APPROVED DRUG PRODUCT LIST B - 1 APPENDIX B - PRODUCT NAME SORTED BY APPLICANT ** 3 ** 3D IMAGING DRUG * 3D IMAGING DRUG DESIGN AND DEVELOPMENT LLC AMMONIA N 13, AMMONIA N-13 FLUDEOXYGLUCOSE F18, FLUDEOXYGLUCOSE F-18 SODIUM FLUORIDE F-18, SODIUM FLUORIDE F-18 3M * 3M CO PERIDEX, CHLORHEXIDINE GLUCONATE * 3M HEALTH CARE INC AVAGARD, ALCOHOL (OTC) DURAPREP, IODINE POVACRYLEX (OTC) 3M HEALTH CARE * 3M HEALTH CARE INFECTION PREVENTION DIV SOLUPREP, CHLORHEXIDINE GLUCONATE (OTC) ** 6 ** 60 DEGREES PHARMS * 60 DEGREES PHARMACEUTICALS LLC ARAKODA, TAFENOQUINE SUCCINATE ** A ** AAA USA INC * ADVANCED ACCELERATOR APPLICATIONS USA INC LUTATHERA, LUTETIUM DOTATATE LU-177 NETSPOT, GALLIUM DOTATATE GA-68 AAIPHARMA LLC * AAIPHARMA LLC AZASAN, AZATHIOPRINE ABBVIE * ABBVIE INC ANDROGEL, TESTOSTERONE CYCLOSPORINE, CYCLOSPORINE DEPAKOTE ER, DIVALPROEX SODIUM DEPAKOTE, DIVALPROEX SODIUM GENGRAF, CYCLOSPORINE K-TAB, POTASSIUM CHLORIDE KALETRA, LOPINAVIR NIASPAN, NIACIN NIMBEX PRESERVATIVE FREE, CISATRACURIUM BESYLATE NIMBEX, CISATRACURIUM BESYLATE NORVIR, RITONAVIR SYNTHROID, LEVOTHYROXINE SODIUM ** TARKA, TRANDOLAPRIL TRICOR, FENOFIBRATE TRILIPIX, CHOLINE FENOFIBRATE ULTANE, SEVOFLURANE ZEMPLAR, PARICALCITOL ABBVIE ENDOCRINE * ABBVIE ENDOCRINE INC LUPANETA PACK, LEUPROLIDE ACETATE ABBVIE ENDOCRINE INC * ABBVIE ENDOCRINE INC LUPRON DEPOT, LEUPROLIDE ACETATE LUPRON DEPOT-PED KIT, LEUPROLIDE ACETATE ABBVIE INC * ABBVIE INC DUOPA, CARBIDOPA MAVYRET, GLECAPREVIR NORVIR, RITONAVIR ORIAHNN (COPACKAGED), ELAGOLIX SODIUM,ESTRADIOL,NORETHINDRONE ACETATE -

Polypharmacy-Associated Potential Contraindications of Drug
Tanaka et al. Journal of Pharmaceutical Health Care and Sciences (2021) 7:17 https://doi.org/10.1186/s40780-021-00196-w RESEARCH ARTICLE Open Access Polypharmacy-associated potential contraindications of drug prescriptions in patients with primary angle closure disease in a real-world setting Fumiaki Tanaka1,2, Naoki Shibatani1,2, Kazumi Fujita1,2, Hiroaki Ikesue2, Satoru Yoshimizu3, Nobuyuki Muroi1,2*, Yasuo Kurimoto3 and Tohru Hashida2 Abstract Background: Primary angle closure disease (PACD) is a type of glaucoma in which the intraocular pressure (IOP) is increased because of the blockage of the anterior chamber angle. Medications contraindicated for patients with PACD, such as anticholinergics, cause mydriasis, and can elevate IOP. However, anticholinergics are currently contraindicated only for primary angle closure glaucoma (PACG) in Japanese package inserts. In this study, we investigated the prescription status of medications contraindicated for PACD, such as anticholinergics, in patients with PACD scheduled for eye surgeries. Methods: Forty-three Japanese patients diagnosed with PACD at Kobe City Eye Hospital, Japan, and scheduled hospitalization for eye surgeries between December 2017 and July 2018, were included. Data, including sex, age, diagnosis, IOP, anterior chamber depth, and patients’ regular medications prior to hospitalization, were collected for each patient from the electronic medical records. Results: The number of patients with chronic primary angle closure (CPAC) and acute primary angle closure (APAC) was 35 (81.4%) and 8 (18.6%), respectively. Among all the 43 patients with PACD, 8 (18.6%) received 15 medications that are potentially contraindicated for PACD by non-ophthalmologist. According to medication categories, benzodiazepine hypnotics were the most commonly prescribed. -

Meta-Analysis of the Efficacy and Safety of Imidafenacin for Overactive Bladder Induced by Benign Prostatic Hyperplasia in Men Receiving Alpha-Blocker Therapy
INTERNATIONAL NEUROUROLOGY JOURNAL INTERNATIONAL INJ pISSN 2093-4777 eISSN 2093-6931 Original Article Int Neurourol J 2020;24(4):365-374 NEU INTERNATIONAL RO UROLOGY JOURNAL https://doi.org/10.5213/inj.2040146.073 pISSN 2093-4777 · eISSN 2093-6931 Volume 19 | Number 2 June 2015 Volume pages 131-210 Official Journal of Korean Continence Society / Korean Society of Urological Research / The Korean Children’s Continence and Enuresis Society / The Korean Association of Urogenital Tract Infection and Inflammation einj.org Mobile Web Meta-Analysis of the Efficacy and Safety of Imidafenacin for Overactive Bladder Induced by Benign Prostatic Hyperplasia in Men Receiving Alpha-Blocker Therapy Tong Cai 1,2,*, Ning Wang2,*, Liye Liang3, Zhongbao Zhou2, Yong Zhang4, Yuanshan Cui2,4 1School of Clinical Medicine, Binzhou Medical University, Yantai, Shandong, China 2Department of Urology, The Affiliated Yantai Yuhuangding Hospital of Qingdao University, Yantai, Shandong, China 3Department of Urology, Rizhao traditional Chinese Hospital, Rizhao, Shandong, China 4Department of Urology, Beijing Tiantan Hospital, Capital Medical University, Beijing, China Purpose: The aim of this meta-analysis was to evaluate the efficacy and safety of imidafenacin for overactive bladder (OAB) induced by benign prostatic hyperplasia (BPH) in men receiving alpha-blocker monotherapy. Methods: We performed a systematic research of the PubMed, Embase, and Cochrane Library databases, and searched for studies about alpha-blocker with or without imidafenacin treatment for OAB in patients with BPH. We also investigated the original references of the included texts. Results: Four randomized controlled trials including 779 participants with BPH (389 in the alpha-blocker+imidafenacin group and 390 in the alpha-blocker only group) were studied.