Drug Coverage Guidelines – Oxford Clinical Policy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Endothelin System and Therapeutic Application of Endothelin Receptor
xperim ACCESS Freely available online & E en OPEN l ta a l ic P in h l a C r m f o a c l a o n l o r g u y o J Journal of ISSN: 2161-1459 Clinical & Experimental Pharmacology Research Article Endothelin System and Therapeutic Application of Endothelin Receptor Antagonists Abebe Basazn Mekuria, Zemene Demelash Kifle*, Mohammedbrhan Abdelwuhab Department of Pharmacology, School of Pharmacy, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia ABSTRACT Endothelin is a 21 amino acid molecule endogenous potent vasoconstrictor peptide. Endothelin is synthesized in vascular endothelial and smooth muscle cells, as well as in neural, renal, pulmonic, and inflammatory cells. It acts through a seven transmembrane endothelin receptor A (ETA) and endothelin receptor B (ETB) receptors belongs to G protein-coupled rhodopsin-type receptor superfamily. This peptide involved in pathogenesis of cardiovascular disorder like (heart failure, arterial hypertension, myocardial infraction and atherosclerosis), renal failure, pulmonary arterial hypertension and it also involved in pathogenesis of cancer. Potentially endothelin receptor antagonist helps the treatment of the above disorder. Currently, there are a lot of trails both per-clinical and clinical on endothelin antagonist for various cardiovascular, pulmonary and cancer disorder. Some are approved by FAD for the treatment. These agents are including both selective and non-selective endothelin receptor antagonist (ETA/B). Currently, Bosentan, Ambrisentan, and Macitentan approved -

NG198 Evidence Review E1
1 2 Research recommendations for review question: For people with mild to 3 moderate acne vulgaris what are the most effective treatment options? 4 Research question - physical modalities 5 What is the effectiveness of physical modalities (such as light devices) in the treatment of 6 acne vulgaris or persistent acne vulgaris-related scarring? 7 Why this is important 8 Physical treatments for acne are popular with people because they have the benefit of 9 treating a local area without systemic effects. They can be used in people with co-morbidities 10 or side effects where other treatments are unsuitable. They are currently available in the 11 private sector but there is no standardisation of treatment modalities or duration. Many 12 different physical therapies have been described for acne including: 13 • Comedone extraction 14 • Phototherapy – including UVB, intense pulsed light, blue and red light 15 • Photochemical therapy (e.g. photodynamic therapy) 16 • Laser 17 • Photopneumatic therapy (e.g. intense pulsed light + vacuum) 18 • Photothermal therapy (eg gold nanoparticles +light or laser) 19 Physical treatments are also used for acne scarring. These include: 20 • Punch excision 21 • CO2 laser 22 • Dermabrasion 23 • Radiofrequency (e.g. fractional microneedling, bipolar) 24 Further research is required to determine the most effective physical treatments for acne and 25 acne scarring. This could open the way to wider availability in the NHS. 26 Table 26: Research recommendation rationale Research question What is the effectiveness of physical modalities (such as light devices) in the treatment of acne vulgaris or persistent acne vulgaris-related scarring? Why is this needed Importance to ‘patients’ or the Physical treatments for acne are popular with people because population they have the benefit of treating a local area without systemic effects. -

The National Drugs List
^ ^ ^ ^ ^[ ^ The National Drugs List Of Syrian Arab Republic Sexth Edition 2006 ! " # "$ % &'() " # * +$, -. / & 0 /+12 3 4" 5 "$ . "$ 67"5,) 0 " /! !2 4? @ % 88 9 3: " # "$ ;+<=2 – G# H H2 I) – 6( – 65 : A B C "5 : , D )* . J!* HK"3 H"$ T ) 4 B K<) +$ LMA N O 3 4P<B &Q / RS ) H< C4VH /430 / 1988 V W* < C A GQ ") 4V / 1000 / C4VH /820 / 2001 V XX K<# C ,V /500 / 1992 V "!X V /946 / 2004 V Z < C V /914 / 2003 V ) < ] +$, [2 / ,) @# @ S%Q2 J"= [ &<\ @ +$ LMA 1 O \ . S X '( ^ & M_ `AB @ &' 3 4" + @ V= 4 )\ " : N " # "$ 6 ) G" 3Q + a C G /<"B d3: C K7 e , fM 4 Q b"$ " < $\ c"7: 5) G . HHH3Q J # Hg ' V"h 6< G* H5 !" # $%" & $' ,* ( )* + 2 ا اوا ادو +% 5 j 2 i1 6 B J' 6<X " 6"[ i2 "$ "< * i3 10 6 i4 11 6! ^ i5 13 6<X "!# * i6 15 7 G!, 6 - k 24"$d dl ?K V *4V h 63[46 ' i8 19 Adl 20 "( 2 i9 20 G Q) 6 i10 20 a 6 m[, 6 i11 21 ?K V $n i12 21 "% * i13 23 b+ 6 i14 23 oe C * i15 24 !, 2 6\ i16 25 C V pq * i17 26 ( S 6) 1, ++ &"r i19 3 +% 27 G 6 ""% i19 28 ^ Ks 2 i20 31 % Ks 2 i21 32 s * i22 35 " " * i23 37 "$ * i24 38 6" i25 39 V t h Gu* v!* 2 i26 39 ( 2 i27 40 B w< Ks 2 i28 40 d C &"r i29 42 "' 6 i30 42 " * i31 42 ":< * i32 5 ./ 0" -33 4 : ANAESTHETICS $ 1 2 -1 :GENERAL ANAESTHETICS AND OXYGEN 4 $1 2 2- ATRACURIUM BESYLATE DROPERIDOL ETHER FENTANYL HALOTHANE ISOFLURANE KETAMINE HCL NITROUS OXIDE OXYGEN PROPOFOL REMIFENTANIL SEVOFLURANE SUFENTANIL THIOPENTAL :LOCAL ANAESTHETICS !67$1 2 -5 AMYLEINE HCL=AMYLOCAINE ARTICAINE BENZOCAINE BUPIVACAINE CINCHOCAINE LIDOCAINE MEPIVACAINE OXETHAZAINE PRAMOXINE PRILOCAINE PREOPERATIVE MEDICATION & SEDATION FOR 9*: ;< " 2 -8 : : SHORT -TERM PROCEDURES ATROPINE DIAZEPAM INJ. -

June 2021 Therapeutic Research Center (TRC) Is the Leading Advisory Service on Drug Therapy and Medication Management
June 2021 Therapeutic Research Center (TRC) is the leading advisory service on drug therapy and medication management. Every month over 400,000 prescribers, pharmacists, and pharmacy technicians rely on our unbiased, evidence-based clinical recommendations to help them improve medication use, prevent medication errors, and improve patient care and outcomes. We also have one of the most extensive CE/CME course offerings in the industry. Our accredited continuing education and continuing medical education courses are trusted and relied on by hundreds of thousands of pharmacists, technicians, and prescribers every month. Therapeutic Research Center does not receive commercial support and does not accept any advertising. It is completely independent and is supported entirely by subscriptions. Credit is reported to CPE Monitor, AAFP, and CE Broker as appropriate. Accreditation Information: Therapeutic Research Center is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing education for physicians. Pharmacist’s Letter / Therapeutic Research Center is accredited by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education. Therapeutic Research Center / Prescriber’s Letter is accredited by the American Association of Nurse Practitioners as an approved provider of nurse practitioner continuing education. Provider number:080517. Select Therapeutic Research Center courses are also acceptable for American Academy of Family Physicians (AAFP) Prescribed credit, American Osteopathic Association (AOA) credit, and American College of Emergency Physicians (ACEP) Category I Credit. Please refer to the detailed accreditation statements available online for each course. Get started at TherapeuticResearchCenter.com. Log in to access your course list or purchase a course or subscription. For additional assistance, please call 209-472-2240 and we’ll be happy to help you. -

Supplement Ii to the Japanese Pharmacopoeia Fifteenth Edition
SUPPLEMENT II TO THE JAPANESE PHARMACOPOEIA FIFTEENTH EDITION Official From October 1, 2009 English Version THE MINISTRY OF HEALTH, LABOUR AND WELFARE Notice: This English Version of the Japanese Pharmacopoeia is published for the conven- ience of users unfamiliar with the Japanese language. When and if any discrepancy arises between the Japanese original and its English translation, the former is authentic. The Ministry of Health, Labour and Welfare Ministerial Notification No. 425 Pursuant to Paragraph 1, Article 41 of the Pharmaceutical Affairs Law (Law No. 145, 1960), we hereby revise a part of the Japanese Pharmacopoeia (Ministerial Notification No. 285, 2006) as follows*, and the revised Japanese Pharmacopoeia shall come into ef- fect on October 1, 2009. However, in the case of drugs which are listed in the Japanese Pharmacopoeia (hereinafter referred to as “previous Pharmacopoeia”) [limited to those listed in the Japanese Pharmacopoeia whose standards are changed in accordance with this notification (hereinafter referred to as “new Pharmacopoeia”)] and drugs which have been approved as of October 1, 2009 as prescribed under Paragraph 1, Article 14 of the same law [including drugs the Minister of Health, Labour and Welfare specifies (the Ministry of Health and Welfare Ministerial Notification No. 104, 1994) as those ex- empted from marketing approval pursuant to Paragraph 1, Article 14 of the Pharmaceu- tical Affairs Law (hereinafter referred to as “drugs exempted from approval”)], the Name and Standards established in the previous Pharmacopoeia (limited to part of the Name and Standards for the drugs concerned) may be accepted to conform to the Name and Standards established in the new Pharmacopoeia before and on March 31, 2011. -

Prednisolone Versus Dexamethasone for Croup: a Randomized Controlled Trial Colin M
Prednisolone Versus Dexamethasone for Croup: a Randomized Controlled Trial Colin M. Parker, MBChB, DCH, MRCPCH, FACEM,a,b Matthew N. Cooper, BCA, BSc, PhDc OBJECTIVES: The use of either prednisolone or low-dose dexamethasone in the treatment of abstract childhood croup lacks a rigorous evidence base despite widespread use. In this study, we compare dexamethasone at 0.6 mg/kg with both low-dose dexamethasone at 0.15 mg/kg and prednisolone at 1 mg/kg. METHODS: Prospective, double-blind, noninferiority randomized controlled trial based in 1 tertiary pediatric emergency department and 1 urban district emergency department in Perth, Western Australia. Inclusions were age .6 months, maximum weight 20 kg, contactable by telephone, and English-speaking caregivers. Exclusion criteria were known prednisolone or dexamethasone allergy, immunosuppressive disease or treatment, steroid therapy or enrollment in the study within the previous 14 days, and a high clinical suspicion of an alternative diagnosis. A total of 1252 participants were enrolled and randomly assigned to receive dexamethasone (0.6 mg/kg; n = 410), low-dose dexamethasone (0.15 mg/kg; n = 410), or prednisolone (1 mg/kg; n = 411). Primary outcome measures included Westley Croup Score 1-hour after treatment and unscheduled medical re-attendance during the 7 days after treatment. RESULTS: Mean Westley Croup Score at baseline was 1.4 for dexamethasone, 1.5 for low-dose dexamethasone, and 1.5 for prednisolone. Adjusted difference in scores at 1 hour, compared with dexamethasone, was 0.03 (95% confidence interval 20.09 to 0.15) for low-dose dexamethasone and 0.05 (95% confidence interval 20.07 to 0.17) for prednisolone. -

AHFS Pharmacologic-Therapeutic Classification System
AHFS Pharmacologic-Therapeutic Classification System Abacavir 48:24 - Mucolytic Agents - 382638 8:18.08.20 - HIV Nucleoside and Nucleotide Reverse Acitretin 84:92 - Skin and Mucous Membrane Agents, Abaloparatide 68:24.08 - Parathyroid Agents - 317036 Aclidinium Abatacept 12:08.08 - Antimuscarinics/Antispasmodics - 313022 92:36 - Disease-modifying Antirheumatic Drugs - Acrivastine 92:20 - Immunomodulatory Agents - 306003 4:08 - Second Generation Antihistamines - 394040 Abciximab 48:04.08 - Second Generation Antihistamines - 394040 20:12.18 - Platelet-aggregation Inhibitors - 395014 Acyclovir Abemaciclib 8:18.32 - Nucleosides and Nucleotides - 381045 10:00 - Antineoplastic Agents - 317058 84:04.06 - Antivirals - 381036 Abiraterone Adalimumab; -adaz 10:00 - Antineoplastic Agents - 311027 92:36 - Disease-modifying Antirheumatic Drugs - AbobotulinumtoxinA 56:92 - GI Drugs, Miscellaneous - 302046 92:20 - Immunomodulatory Agents - 302046 92:92 - Other Miscellaneous Therapeutic Agents - 12:20.92 - Skeletal Muscle Relaxants, Miscellaneous - Adapalene 84:92 - Skin and Mucous Membrane Agents, Acalabrutinib 10:00 - Antineoplastic Agents - 317059 Adefovir Acamprosate 8:18.32 - Nucleosides and Nucleotides - 302036 28:92 - Central Nervous System Agents, Adenosine 24:04.04.24 - Class IV Antiarrhythmics - 304010 Acarbose Adenovirus Vaccine Live Oral 68:20.02 - alpha-Glucosidase Inhibitors - 396015 80:12 - Vaccines - 315016 Acebutolol Ado-Trastuzumab 24:24 - beta-Adrenergic Blocking Agents - 387003 10:00 - Antineoplastic Agents - 313041 12:16.08.08 - Selective -

(19) United States (12) Patent Application Publication (10) Pub
US 20130289061A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2013/0289061 A1 Bhide et al. (43) Pub. Date: Oct. 31, 2013 (54) METHODS AND COMPOSITIONS TO Publication Classi?cation PREVENT ADDICTION (51) Int. Cl. (71) Applicant: The General Hospital Corporation, A61K 31/485 (2006-01) Boston’ MA (Us) A61K 31/4458 (2006.01) (52) U.S. Cl. (72) Inventors: Pradeep G. Bhide; Peabody, MA (US); CPC """"" " A61K31/485 (201301); ‘4161223011? Jmm‘“ Zhu’ Ansm’ MA. (Us); USPC ......... .. 514/282; 514/317; 514/654; 514/618; Thomas J. Spencer; Carhsle; MA (US); 514/279 Joseph Biederman; Brookline; MA (Us) (57) ABSTRACT Disclosed herein is a method of reducing or preventing the development of aversion to a CNS stimulant in a subject (21) App1_ NO_; 13/924,815 comprising; administering a therapeutic amount of the neu rological stimulant and administering an antagonist of the kappa opioid receptor; to thereby reduce or prevent the devel - . opment of aversion to the CNS stimulant in the subject. Also (22) Flled' Jun‘ 24’ 2013 disclosed is a method of reducing or preventing the develop ment of addiction to a CNS stimulant in a subj ect; comprising; _ _ administering the CNS stimulant and administering a mu Related U‘s‘ Apphcatlon Data opioid receptor antagonist to thereby reduce or prevent the (63) Continuation of application NO 13/389,959, ?led on development of addiction to the CNS stimulant in the subject. Apt 27’ 2012’ ?led as application NO_ PCT/US2010/ Also disclosed are pharmaceutical compositions comprising 045486 on Aug' 13 2010' a central nervous system stimulant and an opioid receptor ’ antagonist. -
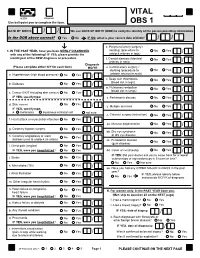
VITAL Jan 2019 Follow-Up
VITAL 6308 Request Use ball-point pen to complete the form. OBS 1 DATE OF BIRTH: / / We use DATE OF BIRTH (DOB) to verify the identity of the person providing information. Is the DOB above correct? Yes No IF NO, what is your correct date of birth? / / s. Peripheral artery surgery / 1. IN THE PAST YEAR, have you been NEWLY DIAGNOSED stenting (procedure to No Yes / with any of the following? IF YES, please provide the unblock arteries in legs) month/year of the NEW diagnosis or procedure. t. Carotid stenosis (blocked No Yes Answer NO/YES on each line. arteries in neck) / Diagnosis (Please complete either N/Y for each item) MO/YR u. Carotid artery surgery / stenting (procedure to No Yes / a. Hypertension (high blood pressure) No Yes / unblock arteries in neck) v. Deep vein thrombosis No Yes (blood clot in legs) / b. Diabetes No Yes / w. Pulmonary embolism No Yes (blood clot in lungs) / c. Cancer (NOT including skin cancer) No Yes / IF YES, specify type: _______________________ x. Parkinson's disease No Yes / d. Skin cancer No Yes / y. Multiple sclerosis No Yes IF YES, specify type: / e. melanoma squamous or basal cell not sure z. Cataract surgery (extraction) No Yes / f. Heart attack or myocardial infarction No Yes / aa. Macular degeneration No Yes / g. Coronary bypass surgery No Yes / bb. Dry eye syndrome No Yes or dry eye disease / h. Coronary angioplasty or stent No Yes (balloon used to unblock an artery) / cc. Periodontal disease No Yes (gum disease) / i. Chest pain (angina) No Yes / IF YES, were you hospitalized? No Yes dd. -

Refreshing the Biologic Pipeline 2020
news feature Credit: Science Lab / Alamy Stock Photo Refreshing the biologic pipeline 2020 In the absence of face-to-face meetings, FDA and industry implemented regulatory workarounds to maintain drug and biologics approvals. These could be here to stay. John Hodgson OVID-19 might have been expected since 1996) — a small miracle in itself “COVID-19 confronted us with the need to severely impair drug approvals (Fig. 1 and Table 1). to better triage sponsors’ questions,” says Cin 2020. In the event, however, To the usual crop of rare disease and Peter Marks, the director of the Center for industry and regulators delivered a small genetic-niche cancer treatments, 2020 Biologics Evaluation and Research (CBER) miracle. They found workarounds and also added a chimeric antigen receptor at the FDA. “That was perhaps the single surrogate methods of engagement. Starting (CAR)-T cell therapy with a cleaner biggest takeaway from the pandemic related in January 2020, when the outbreak veered manufacturing process and the first to product applications.” Marks says that it westward, the number of face-to face approved blockbuster indication for a became very apparent with some COVID- meetings declined rapidly; by March, small-interfering RNA (siRNA) — the 19-related files that resolving a single they were replaced by Webex and Teams. European Medicines Agency’s (EMA) issue can help a sponsor enormously and (Secure Zoom meeting are to be added registration of the RNA interference accelerate the development cycle. Before this year.) And remarkably, by 31 December, (RNAi) therapy Leqvio (inclisiran) for COVID-19, it was conceivable that a small the US Food and Drug Administration cardiovascular disease. -

Regulatory News
WHO Drug Information Vol. 28, No. 4, 2014 Regulatory news Ebola curative – transfusions of whole blood or blood plasma from recovered patients Update on treatments and vaccines have been scheduled to be conducted in Liberia, in line with WHO technical The Ebola crisis has prompted an guidelines (4). unprecedented cooperation between regulators In September the European Medicines to support WHO and to advise on possible Agency (EMA) established an expert pathways for the development, evaluation and group to review available information approval of medicines to fight Ebola. Progress on Ebola experimental treatments – towards provision of treatments and vaccines is excluding convalescent therapies – and summarized below. invited developers to submit their data (5). In August 2014, a WHO-convened panel Vaccines had agreed unanimously that is ethically On 29–30 September, 70 experts acceptable to use of experimental attended a WHO-convened consultation medicines and vaccines under the on Ebola vaccines. They took stock of the exceptional circumstances of the Ebola many ongoing efforts to rapidly evaluate epidemic (1). In early September, WHO the safety and efficacy of Ebola vaccines convened a consultation on potential for deployment as soon as possible to Ebola therapies and vaccines (2). The critical frontline workers and ultimately to importance of supportive care and populations at risk in mass vaccination community response was stressed in this campaigns. Two candidate vaccines have and subsequent discussions. clinical-grade vials available for safety trials. (6) Treatments In October, WHO convened industry In September, more than 200 experts leaders and key partners to discuss trials from around the world met at WHO and production of Ebola vaccine (7). -

(KPIC) PPO and Out-Of- Area Indemnity (OOA) Drug Formulary with Specialty Drug Tier
Kaiser Permanente Insurance Company (KPIC) PPO and Out-of- Area Indemnity (OOA) Drug Formulary with Specialty Drug Tier This Drug Formulary was updated: September 1, 2021 NOTE: This drug formulary is updated often and is subject to change. Upon revision, all previous versions of the drug formulary are no longer in effect. This document contains information regarding the drugs that are covered when you participate in the California Nongrandfathered PPO and Out-of- Area Indemnity (OOA) Health Insurance Plans with specialty drug tier offered by Kaiser Permanente Insurance Company (KPIC) and fill your prescription at a MedImpact network pharmacy. Access to the most current version of the Formulary can be obtained by visiting kp.org/kpic-ca-rx-ppo-ngf. For help understanding your KPIC insurance plan benefits, including cost sharing for drugs under the prescription drug benefit and under the medical benefit, please call 1-800-788-0710 or 711 (TTY) Monday through Friday, 7a.m. to 7p.m. For help with this Formulary, including the processes for submitting an exception request and requesting prior authorization and step therapy exceptions, please call MedImpact 24 hours a day, 7 days a week, at 1-800-788-2949 or 711 (TTY). For cost sharing information for the outpatient prescription drug benefits in your specific plan, please visit: kp.org/kpic-ca-rx-ppo-ngf. For help in your preferred language, please see the Kaiser Permanente Insurance Company Notice of Language Assistance in this document. KPIC PPO NGF Table of Contents Informational Section................................................................................................................................2