SARS-Cov-2 Vaccines Strategies: a Comprehensive Review of Phase 3 Candidates ✉ Nikolaos C
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ifs Recommendations for Covid 19 Vaccination Before Art
16 – 17 JULY 2020 PRAGATI MAIDAN - DELHI INDIAN FERTILITY SOCIETY IFS RECOMMENDATIONS FOR COVID 19 VACCINATION BEFORE ART IFS SECRETARIAT +91 11 40018184 +91 9899308083 indianferlitysociety [email protected] www.indianferlitysociety.org indianferlitysociety 302, 3rd Floor, Kailash Building, ifsdelhi 26, Kasturba Gandhi Marg, C.P. New Delhi - 110001 Cosmo Tech is the Most Important Trade show for the Suppliers to EXPAND Strengthen Increase Multiply Profits New Markets Pan New Market Customer Base India & World Customer Soaring Boost Network Brand Sales Brand Recall Value with the Industry Visibility ORGANIZED BY CALL EMAIL +91 9971811937 [email protected] +91 9999302797 [email protected] +91 9811141938 [email protected] W W W .C O SMO TEC HEXPO IND IA .C O M Dr. Sudha Prasad Dr. Neena Malhotra President Secretary General Indian Fertility Society Indian Fertility Society Director, Matritava Advanced IVF & Professor, ART Centre, Department of Training Cenre, Vasant Vihar, New Delhi Obstetrics and Gynaecology, AIIMS, New Delhi Dr. Sonia Malik Dr. Kuldeep Jain Past President Indian Fertility Society, Past President Indian Fertility Society, Director & Nova Southend Fertility & Director, KJIVF New Delhi IVF Delhi NCR Dr. KU Kunjumoideen Dr. A K Pandey Joint Secretary Indian Fertility Society, Dean Academics &. Co Ordinator Director ARMC IVF Calicut. Molecular Lab. ESI Medical college Faridabad Dr. Charu Jandial Dr. Sumita Aggarwal Member IFS, Consultant, Member IFS, Fellow, Nova Southend Fertility & IVF Delhi NCR Nova Southend Fertility & IVF Delhi NCR Introduction The coronavirus pandemic has wreaked havoc on life In these trying mes, as sociees are gradually trying to and healthcare globally. According to WHO database as return to a state of normalcy, it is also important to on 7th June 2021, there have been 173 million consider sexual and reproducve health of people. -

Review of COVID-19 Vaccine Subtypes, Efficacy and Geographical Distributions Andre Ian Francis ,1 Saudah Ghany,1 Tia Gilkes,1 Srikanth Umakanthan2
Review Postgrad Med J: first published as 10.1136/postgradmedj-2021-140654 on 6 August 2021. Downloaded from Review of COVID-19 vaccine subtypes, efficacy and geographical distributions Andre Ian Francis ,1 Saudah Ghany,1 Tia Gilkes,1 Srikanth Umakanthan2 1Department of Clinical Medical ABSTRACT 2021, the Ad26.COV2.S, developed by Janssen Sciences, The Faculty of Medical As of 1 May 2021, there have been 152 661 445 (Johnson & Johnson) and Moderna on 30 April.4 Sciences, The University of the COVAX, coordinated by WHO, Gavi: The West Indies, St. Augustine, Covid-19 cases with 3 202 256 deaths globally. Trinidad and Tobago This pandemic led to the race to discover a vaccine Vaccine Alliance, the Coalition for Epidemic 2Pathology unit, Department to achieve herd immunity and curtail the damaging Preparedness Innovations (CEPI), acts as a of Paraclinical Sciences, The effects of Covid-19. This study aims to discuss the most programme that supports the development of University Of The West Indies, St. COVID-19 vaccine candidates and negotiates their Augustine, Trinidad and Tobago recent WHO-approved Covid-19 vaccine subtypes, their status and geographical scheduled updates as of 4 pricing to ensure low- and- middle- income countries have a fair shot at receiving vaccines.5 Correspondence to May 2021. The keywords “Covid-19, Vaccines, Pfizer, Mr. Andre Ian Francis, The BNT162b2, AstraZeneca, AZD1222, Moderna, mRNA- This article aims at discussing the most recent University of the West Indies, St. 1273, Janssen, Ad26.COV2.S” were typed into PubMed. WHO- approved COVID-19 vaccine subtypes, their Augustine, Trinidad and Tobago; Thirty Two relevant PubMed articles were included in status and geographical scheduled updates as of 4 andre. -

Combined Live Measles-Mumps Virus Vaccine ROBERT E
Arch Dis Child: first published as 10.1136/adc.48.7.532 on 1 July 1973. Downloaded from Archives of Disease in Childhood, 1973, 48, 532. Combined live measles-mumps virus vaccine ROBERT E. WEIBEL, VICTOR M. VILLAREJOS, GUILLERMO HERNANDEZ C., JOSEPH STOKES, JR.,* EUGENE B. BUYNAK, and MAURICE R. HILLEMAN From the Department of Pediatrics, University of Pennsylvania School of Medicine, Philadelphia, Pennsylvania; Louisiana State University International Center for Medical Research and Training, San Jose, Costa Rica; and the Division of Virus and Cell Biology Research, Merck Institutefor Therapeutic Research, West Point, Pennsylvania, U.S.A. Weibel, R. E., Villarejos, V. M., Hernandez C., G., Stokes, J., Jr., Buynak, E. B., and Hilleman, M. R. (1973). Archives of Disease in Childhood, 48, 532. Combined live measles-mumps virus vaccine. Four lots of combined bivalent live Moraten measles-Jeryl Lynn mumps virus vaccine were administered to a total of 334 children 10 months to 6 years of age, who were initially without antibody against either virus. Overall, 99 % of the children responded serologically to the measles virus and 96 % to mumps. The geometric mean titres were of the same general height as those obtained when the individual vaccines were given alone, and there was no indication of immunological suppression. There was no increase in clinical reaction beyond the mild fever and other reactions that follow the administration of Moraten measles vaccine given alone. The combined measles-mumps vaccine provides a simple means for immunization against both these viruses with no apparent alteration in the immunological or clinical responses. copyright. The need to simplify administration, reduce costs, children) (Mumpsvax) for control purpose. -
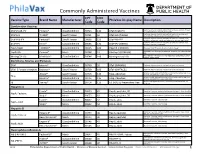
Commonly Administered Vaccines
Commonly Administered Vaccines CPT CVX Vaccine Type Brand Name Manufacturer PhilaVax Display Name Description Code Code Combination Vaccines Diptheria, tetanus toxoids and acellular pertussis vaccine, Hepati- DTaP-HepB-IPV Pediarix® GlaxoSmithKline 90723 110 DTaP-HepB-IPV tis B and poliovirus vaccine, inactivated Diptheria, tetanus toxoids and acellular pertussis vaccine and DTaP-Hib TriHIBit® Sanofi Pasteur 90721 50 DTaP-Hib (TriHIBit) Haemophilus influenzae type b conjugate vaccine Diptheria, tetanus toxoids and acellular pertussis vaccine, Hae- DTaP-Hib-IPV Pentacel® Sanofi Pasteur 90698 120 DTaP-Hib-IPV mophilus influenzae type b, and poliovirus vaccine, inactivated Diptheria, tetanus toxoids and acellular pertussis vaccine, and DTaP-IPV Kinrix® GlaxoSmithKline 90696 130 DTaP-IPV (KINRIX) poliovirus vaccine, inactivated HepA-HepB TWINRIX® GlaxoSmithKline 90636 104 HepA/B (TWINRIX) Hepatisis A and Hepatitis B vaccine, adult dosage Hepatitis B and Hemophilus influenza b vaccine, for intramuscular HepB-Hib Comvax® Merck 90748 51 Hib-Hep B (COMVAX) use Haemophilus influenza b and meningococcal sero groups C and Y MeningC/Y-Hib Menhibrix® GlaxoSmithKline 90644 148 Meningococcal-Hib vaccine, 4 dose series Diphtheria, Tetanus and Pertussis DTaP Infanrix® GlaxoSmithKline 90700 20 DTaP (INFANRIX) Diptheria, tetanus toxoids and acellular pertussis vaccine DTaP, 5 Pertussis Antigens Daptacel® Sanofi Pasteur 90700 106 DTaP (DAPTACEL) Diptheria, tetanus toxoids and acellular pertussis vaccine Tetanus toxoid, reduced diphtheria toxoid, and acellular -

Vaccine Hesitancy
Vaccine Hesitancy Dr Brenda Corcoran National Immunisation Office Presentation Outline An understanding of the following principles: • Overview of immunity • Different types of vaccines and vaccine contents • Vaccine failures • Time intervals between vaccine doses • Vaccine overload • Adverse reactions • Herd immunity Immunity Immunity • The ability of the human body to protect itself from infectious disease The immune system • Cells with a protective function in the – bone marrow – thymus – lymphatic system of ducts and nodes – spleen –blood Types of immunity Source: http://en.wikipedia.org/wiki/Immunological_memory Natural (innate) immunity Non-specific mechanisms – Physical barriers • skin and mucous membranes – Chemical barriers • gastric and digestive enzymes – Cellular and protein secretions • phagocytes, macrophages, complement system ** No “memory” of protection exists afterwards ** Passive immunity – adaptive mechanisms Natural • maternal transfer of antibodies to infant via placenta Artificial • administration of pre- formed substance to provide immediate but short-term protection (antitoxin, antibodies) Protection is temporary and wanes with time (usually few months) Active immunity – adaptive mechanisms Natural • following contact with organism Artificial • administration of agent to stimulate immune response (immunisation) Acquired through contact with an micro-organism Protection produced by individual’s own immune system Protection often life-long but may need boosting How vaccines work • Induce active immunity – Immunity and immunologic memory similar to natural infection but without risk of disease • Immunological memory allows – Rapid recognition and response to pathogen – Prevent or modify effect of disease Live attenuated vaccines Weakened viruses /bacteria – Achieved by growing numerous generations in laboratory – Produces long lasting immune response after one or two doses – Stimulates immune system to react as it does to natural infection – Can cause mild form of the disease (e.g. -

Different Types of COVID-19 Vaccines
Pfizer-BioNTech Help stop the pandemic Type of vaccine: Messenger RNA, or mRNA, a genetic Different Types material that tells your body how to make proteins that by getting vaccinated triggers an immune response inside our bodies of COVID-19 Effectiveness: 95% based on clinical trials Even if you are undocumented Common side effects: Pain and/or swelling in the arm and/or don’t have insurance, you and tiredness, headache, muscle pain, chills, fever, or can get the vaccine—for free. Vaccines: nausea in the body that may last two days Recommended Ages: 16 and older (currently testing the vaccine in kids ages 12-15) Understanding How Dosage: Two shots, 21 days apart They Work Visit VaccinateALL58.com Moderna for the newest information about when and where the vaccine Type of vaccine: Messenger RNA, or mRNA, a genetic will be available to you. material that tells your body how to make proteins that triggers an immune response inside our bodies Sign up at myturn.ca.gov or Effectiveness: 94.1% based on clinical trials call 1-833-422-4255 to find out Common side effects: Pain and/or swelling in the arm if it’s your turn to get vaccinated and and tiredness, headache, muscle pain, chills, fever, or schedule vaccination appointments. nausea in the body that may last two days Recommended Ages: 18 years and older (currently testing the vaccine in kids ages 12-17) Dosage: Two shots, 28 days apart Johnson & Johnson Follow us on social media for more COVID-19 tips and information. Type of vaccine: A viral vector, it uses a harmless version of a different -

Prevention's New Profits
BACKWATER NO MORE: 26 Expected growth of vaccine industry through 2012: 10.5% // Merck’s vaccine sales in 2007: $4.3 billion // Sales from Wyeth’s Prevnar: $2.4 billion // Interest in vaccines: restored. Prevention’s New Profits by Deborah Kelly and Charles slack ntil the late 1960s, for millions of children, 1953 of trials for a vaccine made him a hero—and the news coming down with mumps meant a week two years later that his vaccine had been deemed ready for U or two away from school with fever, sore mass distribution only increased his stature. Measles, rubella throat and painful swollen glands. But in and several dangerous flu strains fell in quick succession, and a fraction of cases, the consequences were it began to seem as if anything were possible. In 1967, U.S. dire, with complications that could include Surgeon General William H. Stewart announced that it was meningitis, paralysis and sterility. Carried on droplets of sa- time to “close the book on infectious diseases.” liva, the virus was so infectious that a child could get it just by Gradually, though, that unbridled optimism gave way to standing near someone who laughed. With time as the only financial and medical realities. As it turned out, vaccines cure, it seemed to be an affliction that might be with us for- weren’t that great a business proposition for private phar- ever. Then one day mumps messed with the wrong little girl. maceutical companies. Vaccines are hugely labor-intensive to When five-year-old Jeryl Lynn Hilleman awoke with a sore develop, and because most combat a single virus, the process throat and swollen glands, her father, virologist Maurice Hille- must be repeated from scratch for each new strain. -

Adenoviral Vector COVID-19 Vaccines: Process and Cost Analysis
processes Article Adenoviral Vector COVID-19 Vaccines: Process and Cost Analysis Rafael G. Ferreira 1,* , Neal F. Gordon 2, Rick Stock 2 and Demetri Petrides 3 1 Intelligen Brasil, Sao Paulo 01227-200, Brazil 2 BDO USA, LLP, Boston, MA 02110, USA; [email protected] (N.F.G.); [email protected] (R.S.) 3 Intelligen, Inc., Scotch Plains, NJ 07076, USA; [email protected] * Correspondence: [email protected] Abstract: The COVID-19 pandemic has motivated the rapid development of numerous vaccines that have proven effective against SARS-CoV-2. Several of these successful vaccines are based on the adenoviral vector platform. The mass manufacturing of these vaccines poses great challenges, especially in the context of a pandemic where extremely large quantities must be produced quickly at an affordable cost. In this work, two baseline processes for the production of a COVID-19 adenoviral vector vaccine, B1 and P1, were designed, simulated and economically evaluated with the aid of the software SuperPro Designer. B1 used a batch cell culture viral production step, with a viral titer of 5 × 1010 viral particles (VP)/mL in both stainless-steel and disposable equipment. P1 used a perfusion cell culture viral production step, with a viral titer of 1 × 1012 VP/mL in exclusively disposable equipment. Both processes were sized to produce 400 M/yr vaccine doses. P1 led to a smaller cost per dose than B1 ($0.15 vs. $0.23) and required a much smaller capital investment ($126 M vs. $299 M). The media and facility-dependent expenses were found to be the main contributors to the operating cost. -
An Overview of COVID Vaccine Clinical Trial Results & Some Challenges
An overview of COVID vaccine clinical trial results & some challenges DCVMN Webinar December 8th, 2020 Access to COVID-19 tools ACCESSACCESS TO TOCOVID-19 COVID-19 TOOLS TOOLS (ACT) (ACT) ACCELERATOR ACCELERATOR (ACT) accelerator A GlobalA GlobalCollaboration Collaboration to Accelerate tothe AccelerateDevelopment, the Production Development, and Equitable Production Access to New and Equitable AccessCOVID-19 to New diagnostics, COVID-19 therapeutics diagnostics, and vaccines therapeutics and vaccines VACCINES DIAGNOSTICS THERAPEUTICS (COVAX) Development & Manufacturing Led by CEPI, with industry Procurement and delivery at scale Led by Gavi Policy and allocation Led by WHO Key players SOURCE: (ACT) ACCELERATOR Commitment and Call to Action 24th April 2020 ACT-A / COVAX governance COVAX COORDINATION MEETING CEPI Board Co-Chair: Jane Halton Co-Chair: Dr. Ngozi Gavi Board Workstream leads + DCVMN and IFPMA-selected Reps As needed – R&D&M Chair; COVAX IPG Chair Development & Manufacturing Procurement and delivery Policy and allocation (COVAX) at scale Led by (with industry) Led by Led by R&D&M Investment Committee COVAX Independent Product Group Technical Review Group Portfolio Group Vaccine Teams SWAT teams RAG 3 COVAX SWAT teams are being set up as a joint platform to accelerate COVID- 19 Vaccine development and manufacturing by addressing common challenges together Timely and targeted Multilateral Knowledge-based Resource-efficient Addresses specific cross- Establishes a dialogue Identifies and collates Coordinates between developer technical and global joint effort most relevant materials different organizations/ challenges as they are across different COVID-19 and insights across the initiatives to limit raised and/or identified vaccines organizations broader COVID-19 duplications and ensure on an ongoing basis (incl. -

Update 50 (15Th of December 2020)
Update 50 (15th of December 2020) Information about Infection disease COVID-19 (novel coronavirus) Force Health Protection Branch FHPB (former DHSC) NATO MILMED COE in Munich 15th of December 2020 email: [email protected] In December 2019, a novel coronavirus emerged in Wuhan City, China. Since then the virus spread to 65 countries including Europe and America. Since then the virus showed evidence for human-to-human transmission as well as evidence of asymptomatic transmission. At 30th January 2020 WHO declared a Public Health Emergency of International Concern. The disease was formally named COVID-19 on 11th of February. The virus itself has been named SARS-CoV-2. On 11th of March 2020 WHO characterized the disease as a pandemic. HIGHLIGHTS/NEWS GLOBALLY ↗ • GBR/WHO: A new variant of the virus could be responsible for the renewed high number of cases in the UK, among other things, which 72 879 777 confirmed cases could be "in connection with the faster spread in the south of England". 47 710 950 recovered So far, 1000 cases have been identified. 1 622 200 deaths The WHO emphasized that the new variant would now be examined. EU/EEA and the UK ↘ However, there is no evidence that the strain behaves differently than 21 936 276 existing virus types. "We saw many variants, this virus evolves and confirmed cases changes over time." 10 689 950 recovered • Sputnik V: The developers of the Russian coronavirus vaccine Sputnik 479 566 deaths V explain that it creates 91.4 percent protection against the lung disease USA ↗ Covid-19. -

Dynamic Transmission Model of Routine Mumps Vaccination in Japan Cambridge.Org/Hyg
Epidemiology and Infection Dynamic transmission model of routine mumps vaccination in Japan cambridge.org/hyg Taito Kitano1,2 1 2 Original Paper Department of Neonatal Intensive Care Unit, Nara Prefecture General Medical Center, Nara, Japan and Master of Public Health Degree Program, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, USA Cite this article: Kitano T (2019). Dynamic transmission model of routine mumps Abstract vaccination in Japan. Epidemiology and Infection 147, e60, 1–8. https://doi.org/ The mumps vaccine is not included in the national immunisation programme (NIP) of 10.1017/S0950268818003230 approximately 80 countries including Japan. To investigate the vaccine’s cost-effectiveness, we developed a dynamic transmission model for routine one- and two-dose mumps vaccin- Received: 5 January 2018 ation programs in Japan. We calculated the incremental cost-effectiveness ratio compared Revised: 10 September 2018 Accepted: 4 November 2018 with a current programme over a projected 50-year period. We created a Japanese population model and performed dynamic simulation to estimate the number of patients enrolled in the Key words: current programme, the routine one-dose programme, and the routine two-dose programme Cost-benefit analysis; immunisation over the next 50 years using the Berkeley Madonna program. We estimated the medical and programme; mumps vaccine; quality-adjusted life years social costs of natural mumps infections and vaccinations to analyse cost-effectiveness. Finally, we performed a sensitivity analysis with parameters including vaccine cost, vaccine efficacy, Author for correspondence: medical costs per case, social costs per case, incidence of adverse events and discount rate. Taito Kitano, E-mail: taito.kitano.0110@gmail. -
Criteria for Reviewing Pneumococcal Conjugate Vaccine
Draft—3/11/10 Oregon School/Facility Immunization Advisory Committee: Review of Pneumococcal Conjugate Vaccine Against Twelve Criteria for Children’s Facility Immunization Requirements Oregon Department of Human Services Public Health Division Office of Family Health Immunization Program 800 NE Oregon Street, Suite 370 Portland, Oregon 97232 Phone: 971-673-0300 Fax: 971-673-0278 Web: www.oregon.gov/DHS/ph/imm Page 1–Review of Pneumococcal Conjugate Vaccine Against Criteria for School Law Immunization Requirements Oregon School/Facility Immunization Advisory Committee: Review of Pneumococcal Conjugate Vaccine Against Twelve Criteria for School/Facility/College Immunization Requirements Process for Reviewing Antigens for Potential Inclusion in OAR 333-050-0050, 333-050-0130 and 333-050-0140. Request for the inclusion of additional antigens or vaccines can come from the Oregon Immunization Program, IPAT (Immunization Policy Advisory Team), or from the community. Proposed changes to vaccine requirements are discussed with IPAT either in a regularly scheduled meeting or through electronic communication. IPAT will submit their comments and a request for consideration to the Oregon Immunization School Law Advisory Committee. The Oregon School/Facility Immunization Advisory Committee was established as a part of the school law immunization requirements when the original legislation was passed in 1980. This Committee is composed of immunization stakeholders from the fields of public health, school health, school administration, medicine, day care, child advocacy and consumers (parents). Through consensus, the committee determines what vaccines (antigens) should be included in Oregon school immunization requirements. Information about new vaccines and the diseases they prevent, including transmission within schools, burden of disease, cost-effectiveness, effect on schools/counties and vaccine availability is presented at a scheduled meeting for committee consideration.