Texas Higher Education Coordinating Board • Kenneth I
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Policy Report Texas Fact Book 2010
Texas Fact Book 2010 Legislative Budget Board LEGISLATIVE BUDGET BOARD EIGHTY-FIRST TEXAS LEGISLATURE 2009 – 2010 DAVID DEWHURST, JOINT CHAIR Lieutenant Governor JOE STRAUS, JOINT CHAIR Representative District 121, San Antonio Speaker of the House of Representatives STEVE OGDEN Senatorial District 5, Bryan Chair, Senate Committee on Finance ROBERT DUNCAN Senatorial District 28, Lubbock JOHN WHITMIRE Senatorial District 15, Houston JUDITH ZAFFIRINI Senatorial District 21, Laredo JIM PITTS Representative District 10, Waxahachie Chair, House Committee on Appropriations RENE OLIVEIRA Representative District 37, Brownsville Chair, House Committee on Ways and Means DAN BRANCH Representative District 108, Dallas SYLVESTER TURNER Representative District 139, Houston JOHN O’Brien, Director COVER PHOTO COURTESY OF HOUSE PHOTOGRAPHY CONTENTS STATE GOVERNMENT STATEWIDE ELECTED OFFICIALS . 1 MEMBERS OF THE EIGHTY-FIRST TEXAS LEGISLATURE . 3 The Senate . 3 The House of Representatives . 4 SENATE STANDING COMMITTEES . 8 HOUSE OF REPRESENTATIVES STANDING COMMITTEES . 10 BASIC STEPS IN THE TEXAS LEGISLATIVE PROCESS . 14 TEXAS AT A GLANCE GOVERNORS OF TEXAS . 15 HOW TEXAS RANKS Agriculture . 17 Crime and Law Enforcement . 17 Defense . 18 Economy . 18 Education . 18 Employment and Labor . 19 Environment and Energy . 19 Federal Government Finance . 20 Geography . 20 Health . 20 Housing . 21 Population . 21 Science and Technology . 22 Social Welfare . 22 State and Local Government Finance . 22 Transportation . 23 Border Facts . 24 STATE HOLIDAYS, 2010 . 25 STATE SYMBOLS . 25 POPULATION Texas Population Compared with the U .s . 26 Texas and the U .s . Annual Population Growth Rates . 27 Resident Population, 15 Most Populous States . 28 Percentage Change in Population, 15 Most Populous States . 28 Texas Resident Population, by Age Group . -
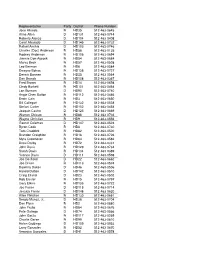
82Nd Leg Members
Representative Party District Phone Number Jose Aliseda R HD35 512-463-0645 Alma Allen D HD131 512-463-0744 Roberto Alonzo D HD104 512-463-0408 Carol Alvarado D HD145 512-463-0732 Rafael Anchia D HD103 512-463-0746 Charles (Doc) Anderson R HD56 512-463-0135 Rodney Anderson R HD106 512-463-0694 Jimmie Don Aycock R HD54 512-463-0684 Marva Beck R HD57 512-463-0508 Leo Berman R HD6 512-463-0584 Dwayne Bohac R HD138 512-463-0727 Dennis Bonnen R HD25 512-463-0564 Dan Branch R HD108 512-463-0367 Fred Brown R HD14 512-463-0698 Cindy Burkett R HD101 512-463-0464 Lon Burnam D HD90 512-463-0740 Angie Chen Button R HD112 512-463-0486 Erwin Cain R HD3 512-463-0650 Bill Callegari R HD132 512-463-0528 Stefani Carter R HD102 512-463-0454 Joaquin Castro D HD125 512-463-0669 Warren Chisum R HD88 512-463-0736 Wayne Christian R HD9 512-463-0556 Garnet Coleman D HD147 512-463-0524 Byron Cook R HD8 512-463-0730 Tom Craddick R HD82 512-463-0500 Brandon Creighton R HD16 512-463-0726 Myra Crownover R HD64 512-463-0582 Drew Darby R HD72 512-463-0331 John Davis R HD129 512-463-0734 Sarah Davis R HD134 512-463-0389 Yvonne Davis D HD111 512-463-0598 Joe Deshotel D HD22 512-463-0662 Joe Driver R HD113 512-463-0574 Dawnna Dukes D HD46 512-463-0506 Harold Dutton D HD142 512-463-0510 Craig Eiland D HD23 512-463-0502 Rob Eissler R HD15 512-463-0797 Gary Elkins R HD135 512-463-0722 Joe Farias D HD118 512-463-0714 Jessica Farrar D HD148 512-463-0620 Allen Fletcher R HD130 512-463-0661 Sergio Munoz, Jr. -

State Representative Jim Pitts
State Representative Jim Pitts District 10 Chairman, House Appropriations Jim Pitts, of Waxahachie, Texas, was born in Dallas, Texas. He attended Southern Methodist University where he received a bachelor of Business Administration with a major in Accounting, Masters of Business Administration, and a Juris Doctorate. Jim and his late wife, Evelyn Eastham Pitts, have three children, two daughters: Duffy Pitts Bloemendal and Ashley Eastham Pitts, and one son: James Ryan Pitts. He is the proud grandfather of three grandsons. Jim is the son of the late Roy and Agnes Pitts. Jim has a twin brother, John, who lives in Houston, Texas, and a sister, Rosemary Burns, who lives in Henderson County. A fourteen-year member of the Board of Trustees for the Waxahachie Independent School District, Jim was serving as President of the Board when he was elected to the Texas House of Representatives. Other offices include director of Citizens National Bank in Waxahachie, director of Sims Library, a past-president of the Waxahachie Chamber of Commerce and immediate past-president and treasurer of the Board of Trustees of Presbyterian Children's Services. He also currently serves on the Community Advisory Council for the Scottish Rite Learning Center. The people of District 10, which consists of Hill and Ellis Counties, elected Jim as their state representative on November 3, 1992. It was a new district resulting from the 1991 redistricting of the state. During the 1993 session of the Texas Legislature, Jim served on the House Committees on Economic Development and Transportation. The 74th session found him serving on the Criminal Jurisprudence Committee and the Corrections Committee. -

Memo (7-31-13) Hazlewood Legacy Act Reimbustments Corrections
TEXAS HIGHER EDUCATION COORDINATING BOARD P.O. Box 12788 Austin, Texas 78711 Fred W. Heldenfels IV CHAIR July 31, 2013 Harold W. Hahn VICE CHAIR Dennis D. Golden, O.D. TO: Ursula Parks, Director SECRETARY OF THE BOARD Legislative Budget Board Alice Schneider STUDENT REPRESENTATIVE Durga D. Agrawal, Ph.D. FROM: Raymund A. Paredes Christopher M. Huckabee Robert W. Jenkins, Jr. Munir Abdul Lalani SUBJECT: Formula for Distributing Hazlewood Legacy Act Reimbursements Janelle Shepard David D. Teuscher, M.D. Raymund A. Paredes COMMISSIONER House Bill 1025, passed by the 83rd Legislature, Regular Session, appropriates $30 OF HIGHER EDUCATION million to reimburse public institutions of higher education for costs associated with 512/ 427-6101 the Hazlewood Legacy Program (TEC 54.341(k)). The Legislation directs the Fax 512/ 427-6127 Coordinating Board to develop a plan to allocate the appropriations according to the Web site: http://www.thecb.state.tx.us proportion of each institution's respective share of the aggregate cost of the exemption for students under the Legacy Program, subject to input by institutions for their respective share, and present the plan to the Legislative Budget Board no later than August 1, 2013. On June 7, all institutions were advised via memo that the allocation of the HB 1025 funding would be based on their FY2012 data regarding Legacy students as they reported in the Hazlewood Exemption Database Report, and that they had until July 15 to review, revise and correct any misreported data. A June 28 notice was sent to Hazlewood contacts to remind them of the deadline. -

Policy Report Texas Fact Book 2006
Te x a s F a c t Book 2006 LEGISLATIVE BUDGET BOARD LEGISLATIVE BUDGET BOARD SEVENTY-NINTH TEXAS LEGISLATURE 2005 – 2006 DAVID DEWHURST, CO-CHAIR Lieutenant Governor, Austin TOM CRADDICK, CO-CHAIR Representative District 82, Midland Speaker of the House of Representatives STEVE OGDEN Senatorial District 5, Bryan Chair, Senate Committee on Finance ROBERT DUNCAN Senatorial District 28, Lubbock JOHN WHITMIRE Senatorial District 15, Houston JUDITH ZAFFIRINI Senatorial District 21, Laredo JIM PITTS Representative District 10, Waxahachie Chair, House Committee on Appropriations JAMES KEFFER Representative District 60, Eastland Chair, House Committee on Ways and Means FRED HILL Representative District 112, Richardson VILMA LUNA Representative District 33, Corpus Christi JOHN O’BRIEN, Deputy Director CONTENTS STATE GOVERNMENT STATEWIDE ELECTED OFFICIALS . 1 MEMBERS OF THE SEVENTY-NINTH TEXAS LEGISLATURE . 3 The Senate . 3 The House of Representatives . 4 SENATE STANDING COMMITTEES . 8 HOUSE OF REPRESENTATIVES STANDING COMMITTEES . 10 BASIC STEPS IN THE TEXAS LEGISLATIVE PROCESS . 14 TEXAS AT A GLANCE GOVERNORS OF TEXAS . 15 HOW TEXAS RANKS Agriculture . 17 Crime and Law Enforcement . 17 Defense . 18 Economy . 18 Education . 18 Employment and Labor . 19 Environment and Energy . 19 Federal Government Finance . 20 Geography . 20 Health . 20 Housing. 21 Population . 21 Social Welfare . 22 State and Local Government Finance . 22 Technology . 23 Transportation . 23 Border Facts . 24 STATE HOLIDAYS, 2006 . 25 STATE SYMBOLS . 25 POPULATION Texas Population Compared with the U.S. 26 Texas and the U.S. Annual Population Growth Rates . 27 Resident Population, 15 Most Populous States . 28 Percentage Change in Population, 15 Most Populous States . 28 Texas Resident Population, by Age Group . -

Texas Fact Book
LEGISLATIVE BUDGET BOARD Texas Fact Book LEGISLATIVE BUDGET BOARD 2014 YELLOW (PMS 7403C): C5, M15, Y57 .25” BLEED ON ALL 4 SIDES Texas Fact Book LEGISLATIVE BUDGET BOARD 2014 LEGISLATIVE BUDGET BOARD EIGHTY-THIRD TEXAS LEGISLATURE DAVID DEWHURST, CO-CHAIR Lieutenant Governor, Austin JOE STRAUS, CO-CHAIR Representative District 121, San Antonio Speaker of the House of Representatives TOMMY WILLIAMS* Senatorial District 5, Th e Woodlands Chair, Senate Committee on Finance ROBERT DUNCAN Senatorial District 28, Lubbock JUAN “CHUY” HINOJOSA Senatorial District 20, McAllen JUDITH ZAFFIRINI Senatorial District 21, Laredo JIM PITTS Representative District 10, Waxahachie Chair, House Committee on Appropriations HARVEY HILDERBRAN Representative District 53, Kerrville Chair, House Committee on Ways and Means DAN BRANCH Representative District 108, Dallas SYLVESTER TURNER Representative District 139, Houston *Chairman Williams resigned from the Texas Senate on October 26, 2013 CONTENTS STATE GOVERNMENT Statewide Elected Officials.................................................................... 1 Members of the Eighty-third Texas Legislature ............................................ 3 The Senate ........................................................................................ 3 The House of Representatives .......................................................... 4 Senate Standing Committees................................................................ 9 House of Representatives Standing Committees.......................................11 -

Supreme Court of the United States
No. 02-102 ================================================================ In The Supreme Court of the United States --------------------------------- ♦ --------------------------------- JOHN GEDDES LAWRENCE AND TYRONE GARNER, Petitioners, v. STATE OF TEXAS, Respondent. --------------------------------- ♦ --------------------------------- On Writ Of Certiorari To The Court Of Appeals Of Texas, Fourteenth District --------------------------------- ♦ --------------------------------- BRIEF OF AMICI CURIAE TEXAS LEGISLATORS, REPRESENTATIVE WARREN CHISUM, ET AL., IN SUPPORT OF RESPONDENT --------------------------------- ♦ --------------------------------- SCOTT ROBERTS KELLY SHACKELFORD 1206 Oakwood Trail Counsel of Record Southlake, Texas 76092 HIRAM S. SASSER III (817) 424-3923 LIBERTY LEGAL INSTITUTE 903 18th Street, Suite 230 Plano, Texas 75074 (972) 423-3131 ================================================================ COCKLE LAW BRIEF PRINTING CO. (800) 225-6964 OR CALL COLLECT (402) 342-2831 Amici are: Texas Legislators: Representative Warren Chisum; Representative Will Hartnet, Chair, House Committee on Judicial Affairs; Representative Diane Delisi; Representative Mary Denny; Representative Rob Eissler; Representative Mike Flynn; Representative Toby Goodman; Representative Mike Hamilton; Representative Anna Mowery; Representative Beverly Wooley; Representative Geanie Morrison; Representative Phil King; Representative Carl Isett; Representative Charlie Howard; Representative Leo Berman; Representative Dwayne Bohac; Representative -

Commission and Foundation Applaud the Legislature for Providing Legal Aid Funding
UPDATE September 2011 Increasing access to justice for low-income Texans Commission and Foundation Applaud the Legislature for Providing Legal Aid Funding In a tremendous show of bipartisan a privilege to offer this amendment to help want to speak at funerals. I want to speak at support, the Texas Legislature appropriated protect Texans' fundamental right to fair commencements and places we've invested $17.5 million for civil legal aid and $7.6 legal representation,” Pitts said. in folks at a bad time in their lives," she said. million for county indigent defense Rep. Will Hartnett and Rep. Jerry Madden Sen. José Rodriguez, Rep. Pete P. Gallego programs in general revenue for the were also among the many supporters and James B. Sales, Chair Emeritus of the biennieum during the recent special session. in the House. “Assuring access to basic TAJC, also spoke at the briefing in support Gov. Rick Perry signed Senate Bill 2 that legal services is a vital role of our state of funding for legal aid in Texas. included an amendment for funding civil government,” Hartnett said. “I am delighted legal services on July 19. that the House has renewed the funding of This funding mitigates the decline in this important program.” Interest on Lawyers’ Trust Accounts (IOLTA) In a historic move, the Texas Legislature funds, a primary source of funding for legal issued a joint resolution in June commending aid. IOLTA funding has declined more than the Supreme Court for its efforts to preserve 71 percent since 2007. access to justice for all Texans. “All Texans should be grateful for the actions of the Texas House and Senate in Press Conference Highlights Needs these efforts to provide access to justice Before the approval of legal aid funding for Texans who could otherwise not afford in the special session, several groups and it,” Texas Supreme Court Justice Nathan L. -

2007 Legislative Report.Indd
TEXAS LAND TITLE ASSOCIATION LEGISLATIVE2007 REPORT by Mindy Carr, TLTA Director of Government Affairs or the fi rst time in several years, the Texas Legislature convened SESSION FACTS the session without any emergency issues on the table. In 2003, TLTA tracked 667 bills F they dealt with the controversial congressional redistricting issue and in 2005, revision of the school fi nance system and property tax relief were top priorities. However, within the fi rst several weeks, Of more than 6,300 bills filed, approximately 24% a number of big issues arose causing the Legislature to spend most of them were passed of the year in response mode. From moving to block the Governor’s into law controversial order of the HPV vaccine to overhauling the troubled Texas Youth Commission, members of the Legislature were forced to deal with 49 bills were vetoed by emotionally charged issues that greatly impacted their constituents. As Governor Perry the session continued, Legislators’ personal agendas, such as a statewide smoking ban, the death penalty for sexual predators, toll roads and Number of days in the regular water reservoirs, gradually became top priority. session – 140 In turn, the title insurance industry also fell into response mode. In There are 31 members in the February, the Attorney General released an opinion stating that social Senate and 150 members in the House security numbers (SSNs) were confi dential and county clerks would be held criminally responsible if the numbers were released. This caused the State senators are elected for majority of the 254 county courthouses to either shut down or limit the four-year terms (Staggered) real estate industry’s access to offi cial public records. -

83Rd Legislative Session Building on Success
TEXAS DEPARTMENT OF TRANSPORTATION 83RD LEGISLATIVE SESSION BUILDING ON SUCCESS TABle OF Contents INTRODUCTION ...................................................................................................................... 1 TXDOT MISSION, GOALS AND PRIORITIES ......................................................................... 2 A MESSagE FROM TXDOT EXECUTIVE DiRECTOR PHil WilSON .................................................................................. 3 2013 LEGISlaTIVE SESSION OVERVIEW ............................................................................ 4 Regular Session ..................................................4 Called Sessions ..................................................7 FEATURED LEGISlaTION AND EVENTS ............................................................................... 9 8th Annual Texas Transportation Forum.................9 Funding Repairs to Roads Damaged Comprehensive Development by Energy Development Activities Agreements (SB 1730) .........................................10 (HB 1025 and SB 1747) ......................................14 TxDOT Podcast ....................................................11 Increasing Enforcement for Nonpayment of Tolls (SB 1792) ........................17 Streamlining the Environmental Review Process (SB 466) ....................................12 Expanding Move Over/Slow Down Coverage to TxDOT (SB 510) .................................18 83RD TEXAS LEGISlaTURE - BillS ENACTED .................................................................. -

PARTNERS in MOBILITY a Coalition of Dallas-Fort Worth Area Public and Private Transportation Interest Groups
DRAFT MINUTE ORDERS ARE SUBJECT TO CHANGE PRIOR TO COMMISSION APPROVAL PARTNERS IN MOBILITY A Coalition of Dallas-Fort Worth Area Public and Private Transportation Interest Groups January 15, 2009 Mr. William L. Hale, P.E. TxDOT District Engineer P. O. Box 133067 Dallas, Texas 75313-3067 Dear Mr. Hale: Annually since 1995 the Partners in Mobility coalition has taken a delegation of public and private leaders from the Dallas/Fort Worth metropolitan area to Austin to inform the Texas Transportation Commission of our region’s progress and challenges in moving people and goods within and through the re gion. The District has always provided cooperation and assistance in processing the delegation petition, for which we are most appreciative. We would like to appear before the Commission March 26, 2009. We will identify several presenters representative of the North Texas local government and business communities to deliver our coalition’s 20-minute presentation to the Commission and will advise you of their names and affiliations as soon as we have commitments from them. As always, we will coordinate and communicate with you in the development of the presentation contents. Enclosed is a draft delegation petition. Please let us know if you would like any changes in the petition or if you have any questions or need additional information at this time. Thank you very much. Sincerely, Vic Suhm cc. Maribel Chavez Steve Simmons North Texas Commission P.O. Box 610246 DFW Airport, Texas 75261 972-621-0400 Founded in 1995, the Partners In Mobility is a broad based public-private sector coalition of the Dallas Regional Mobility Coalition, the Fort Worth Chamber of Commerce, the Greater Dallas Chamber, the North Central Texas Council of Governments/Regional Transportation Council, the North Texas Commission, and the Tarrant Regional Transportation Coalition. -

INSIDE INTELLIGENCE: the Texas Weekly/Texas Tribune Insider's Poll for 4 April 2011
The insider's poll for the week of April 4. INSIDE INTELLIGENCE: The Texas Weekly/Texas Tribune insider's poll for 4 April 2011 We're past the halfway point of this session. What's your take on the top leaders — Gov. Rick Perry, Lt. Gov. David Dewhurst, and House Speaker Joe Straus? • "Too early to tell." • "Perry is thinking 2 much abt a national seat and its effing up our session. Dewhurst and • "Perry is looking at a national office, so he's Straus seem to be more grounded in reality." posturing to the right. Dewhurst is looking at the U.S. Senate, so he's doing the same thing. • "Dewhurst and Straus are doing the best Straus seems to be keeping a low profile right they can with Perry's mess" now--he's either indecisive or waiting for a time to make his impression felt." • "Straus and Dewhurst have some inkling of actually trying to do their jobs well, Perry • "Things are moving very slow, but that is a does not." good thing. Legislative Redistricting will be done by the LRB so that is not an issue. The • "Lt. Gov. Dewhurst is beginning to pull his budget, if it gets passed, will be the only other weight; the others haven't shown up much." issue. Who cares if anything else gets done? Adjourn and come back later in the year to finish Congressional redistricting." • "Has Perry done anything that he wasn't expected to do? Other than give up a little bit more than $3 billion from the Rainy Day • "Straus - A+..