Maryland Cancer Registry
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Use of High Tumescent Power Assisted Liposuction in the Treatment of Madelung’S Collar
Letter to the Editor The use of high tumescent power assisted liposuction in the treatment of Madelung’s collar Henryk Witmanowski1,2, Łukasz Banasiak1, Grzegorz Kierzynka1, Jarosław Markowicz1, Jerzy Kolasiński1, Katarzyna Błochowiak3, Paweł Szychta1,4 1Department of Plastic, Reconstructive and Aesthetic Surgery, Medical College in Bydgoszcz, Nicolaus Copernicus University in Torun, Poland 2Department of Physiology, Poznan University of Medical Sciences, Poznan, Poland 3Department of the Oral Surgery, Poznan University of Medical Sciences, Poznan, Poland 4Department of Oncological Surgery and Breast Diseases, Polish Mother’s Memorial Hospital-Research Institute, Lodz, Poland Adv Dermatol Allergol 2017; XXXIV (4): 366–371 DOI: https://doi.org/10.5114/ada.2017.69319 Mild symmetrical lipomatosis (plural symmetrical The disease most commonly takes a proximal form lipomatosis, multiple symmetric lipomatosis – MSL), which takes the following areas of the body with the fol- also known as Madelung’s disease or Launois-Bensaude lowing frequency: the genial area 92.3%, cervical region syndrome is a rare disease of unknown etiology, first de- 67.7%, shoulder region 54.8%, abdominal 45.2%, chest scribed by Brodie in 1846, Madelung in 1888, and Launois 41.9%, thigh and pelvic rim 32.3% [11, 12]. The periph- with Bensaude in 1898 [1–3]. eral type mainly locates on both sides at the level of the Madelung’s disease incidence is 1 : 250000 [4]. Mul- hands, feet and knees, this is definitely a rarer form of tiple symmetric lipomatosis occurs mainly in the inhabit- the disease. The mixed form is described very rarely. The ants of the Mediterranean area and Eastern Europe, in specified central type is also engaged primarily around males (male to female ratio is 20 : 1), aged 30–70 years, the lower torso, and intermediate parts of the legs. -
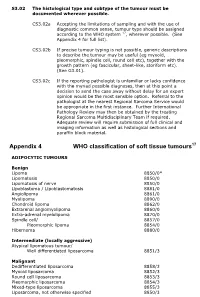
Appendix 4 WHO Classification of Soft Tissue Tumours17
S3.02 The histological type and subtype of the tumour must be documented wherever possible. CS3.02a Accepting the limitations of sampling and with the use of diagnostic common sense, tumour type should be assigned according to the WHO system 17, wherever possible. (See Appendix 4 for full list). CS3.02b If precise tumour typing is not possible, generic descriptions to describe the tumour may be useful (eg myxoid, pleomorphic, spindle cell, round cell etc), together with the growth pattern (eg fascicular, sheet-like, storiform etc). (See G3.01). CS3.02c If the reporting pathologist is unfamiliar or lacks confidence with the myriad possible diagnoses, then at this point a decision to send the case away without delay for an expert opinion would be the most sensible option. Referral to the pathologist at the nearest Regional Sarcoma Service would be appropriate in the first instance. Further International Pathology Review may then be obtained by the treating Regional Sarcoma Multidisciplinary Team if required. Adequate review will require submission of full clinical and imaging information as well as histological sections and paraffin block material. Appendix 4 WHO classification of soft tissue tumours17 ADIPOCYTIC TUMOURS Benign Lipoma 8850/0* Lipomatosis 8850/0 Lipomatosis of nerve 8850/0 Lipoblastoma / Lipoblastomatosis 8881/0 Angiolipoma 8861/0 Myolipoma 8890/0 Chondroid lipoma 8862/0 Extrarenal angiomyolipoma 8860/0 Extra-adrenal myelolipoma 8870/0 Spindle cell/ 8857/0 Pleomorphic lipoma 8854/0 Hibernoma 8880/0 Intermediate (locally -

Eyelid Conjunctival Tumors
EYELID &CONJUNCTIVAL TUMORS PHOTOGRAPHIC ATLAS Dr. Olivier Galatoire Dr. Christine Levy-Gabriel Dr. Mathieu Zmuda EYELID & CONJUNCTIVAL TUMORS 4 EYELID & CONJUNCTIVAL TUMORS Dear readers, All rights of translation, adaptation, or reproduction by any means are reserved in all countries. The reproduction or representation, in whole or in part and by any means, of any of the pages published in the present book without the prior written consent of the publisher, is prohibited and illegal and would constitute an infringement. Only reproductions strictly reserved for the private use of the copier and not intended for collective use, and short analyses and quotations justified by the illustrative or scientific nature of the work in which they are incorporated, are authorized (Law of March 11, 1957 art. 40 and 41 and Criminal Code art. 425). EYELID & CONJUNCTIVAL TUMORS EYELID & CONJUNCTIVAL TUMORS 5 6 EYELID & CONJUNCTIVAL TUMORS Foreword Dr. Serge Morax I am honored to introduce this Photographic Atlas of palpebral and conjunctival tumors,which is the culmination of the close collaboration between Drs. Olivier Galatoire and Mathieu Zmuda of the A. de Rothschild Ophthalmological Foundation and Dr. Christine Levy-Gabriel of the Curie Institute. The subject is now of unquestionable importance and evidently of great interest to Ophthalmologists, whether they are orbital- palpebral specialists or not. Indeed, errors or delays in the diagnosis of tumor pathologies are relatively common and the consequences can be serious in the case of malignant tumors, especially carcinomas. Swift diagnosis and anatomopathological confirmation will lead to a treatment, discussed in multidisciplinary team meetings, ranging from surgery to radiotherapy. -

Apocrine Hidrocystoma: a Slowly Growing Postauricular Translucent Nodule
Volume 27 Number 1| January 2021 Dermatology Online Journal || Photo Vignette 27(1):16 Apocrine hidrocystoma: a slowly growing postauricular translucent nodule Karan Pandher1 BS, Felipe B Cerci2,3 MD MSc, Stanislav N Tolkachjov4 MD Affiliations: 1Chicago Medical School, Rosalind Franklin University of Medicine and Science, North Chicago, Illinois, USA, 2Department of Dermatology. Hospital de Clínicas da Universidade Federal do Paraná, Curitiba, Brazil, 3Clínica Cepelle. Curitiba, Brazil, 4Epiphany Dermatology, Dallas, Texas, USA Corresponding Author: Stanislav N Tolkachjov MD, Epiphany Dermatology, 1640 FM 544, Suite 100, The Colony, TX 75056, Tel: 972-712- 3131, Email: [email protected] importance of histopathological examination of Abstract cystic tumors on the periauricular area. Apocrine hidrocystoma is a benign, cystic proliferation of the apocrine sweat gland that may present commonly on sun-exposed areas of the head Case Synopsis and neck. However, given its location and features, A middle-aged previously healthy woman presented apocrine hidrocystomas may often be confused with with an asymptomatic right postauricular lesion, that malignant tumors such as basal cell carcinomas or primary cutaneous mucinous carcinomas. Herein, we progressed to a nodule over 10 years (Figure 1A). present an unusual case of an apocrine hidrocystoma Physical examination demonstrated a translucent, presenting in the postauricular region and highlight blue-gray nodule with three rounded projections the importance of histopathological examination of and a fibroelastic consistency in the right cystic tumors on the periauricular area. postauricular region measuring 2.3×2cm in diameter. The well-defined nodule was not adherent to deep planes. A similar papule was present Keywords: apocrine hidrocystoma, dermatology, superiorly. -
Pathology and Genetics of Tumours of Soft Tissue and Bone
bb5_1.qxd 13.9.2006 14:05 Page 3 World Health Organization Classification of Tumours WHO OMS International Agency for Research on Cancer (IARC) Pathology and Genetics of Tumours of Soft Tissue and Bone Edited by Christopher D.M. Fletcher K. Krishnan Unni Fredrik Mertens IARCPress Lyon, 2002 bb5_1.qxd 13.9.2006 14:05 Page 4 World Health Organization Classification of Tumours Series Editors Paul Kleihues, M.D. Leslie H. Sobin, M.D. Pathology and Genetics of Tumours of Soft Tissue and Bone Editors Christopher D.M. Fletcher, M.D. K. Krishnan Unni, M.D. Fredrik Mertens, M.D. Coordinating Editor Wojciech Biernat, M.D. Layout Lauren A. Hunter Illustrations Lauren A. Hunter Georges Mollon Printed by LIPS 69009 Lyon, France Publisher IARCPress International Agency for Research on Cancer (IARC) 69008 Lyon, France bb5_1.qxd 13.9.2006 14:05 Page 5 This volume was produced in collaboration with the International Academy of Pathology (IAP) The WHO Classification of Tumours of Soft Tissue and Bone presented in this book reflects the views of a Working Group that convened for an Editorial and Consensus Conference in Lyon, France, April 24-28, 2002. Members of the Working Group are indicated in the List of Contributors on page 369. bb5_1.qxd 22.9.2006 9:03 Page 6 Published by IARC Press, International Agency for Research on Cancer, 150 cours Albert Thomas, F-69008 Lyon, France © International Agency for Research on Cancer, 2002, reprinted 2006 Publications of the World Health Organization enjoy copyright protection in accordance with the provisions of Protocol 2 of the Universal Copyright Convention. -

Treatment Strategies for Well-Differentiated Liposarcomas and Therapeutic Outcomes
ANTICANCER RESEARCH 32: 1821-1826 (2012) Treatment Strategies for Well-differentiated Liposarcomas and Therapeutic Outcomes NORIO YAMAMOTO1, KATSUHIRO HAYASHI1, YOSHIKAZU TANZAWA1, HIROAKI KIMURA1, AKIHIKO TAKEUCHI1, KENTARO IGARASHI1, HIROYUKI INATANI1, SHINGO SHIMOZAKI1, SEIKO KITAMURA2 and HIROYUKI TSUCHIYA1 1Department of Orthopedic Surgery, Graduate School of Medical Sciences, Kanazawa University, Kanazawa, Ishikawa, Japan; 2Department of Pathology, Kanazawa University Hospital, Kanazawa, Ishikawa, Japan Abstract. This study examined 45 patients with well- liposarcoma tends to be less than the one performed in differentiated liposarcoma who were surgically treated at our conventional extensive resection (7, 8). However, operative hospital (initial surgery in 41 patients and reoperation in 4). procedures from marginal resection to extensive resection Only one patient had recurrence among patients who vary among institutions. In this study, we examined the underwent initial surgery, and the recurrence was localised outcomes of well-differentiated liposarcomas treated at our in the retroperitoneal space. For patients who underwent hospital and we discuss future treatment strategies. reoperation, the mean time between the initial surgery and the recurrence was 16.5 years. None of the 45 patients Patients and Methods developed distant metastasis. It is important to preserve not only neurovascular bundles but also lower limb muscles in The subjects of this study were 45 patients with well-differentiated order to maintain ambulatory ability in the elderly patients. liposarcomas who were surgically treated in our hospital between For well-differentiated liposarcomas of the limbs, it is January 1989 and July 2010 and who were followed-up for at least 6 months. The study group consisted of 17 men and 28 women. -

Diagnostic Approach to Neuroendocrine Neoplasms of the Gastrointestinal Tract and Pancreas
Review doi: 10.5146/tjpath.2015.01319 Diagnostic Approach to Neuroendocrine Neoplasms of the Gastrointestinal Tract and Pancreas Silvia UCCELLA1, Fausto SESSA1, Stefano La ROSA2 1Department of Surgical and Morphological Sciences, University of Insubria, VARESE, ITALY, 2Department of Pathology, Ospedale di Circolo, VARESE, ITALY ABSTRACT The gastroenteropancreatic (GEP) system is the site of origin of about two thirds of all neuroendocrine neoplasms (NENs) of the human body. GEP-NENs encompass a wide spectrum of entities, from very indolent tumors to highly aggressive carcinomas. They represent a challenge for the oncologist and a correct diagnostic approach is crucial for the management of patients. The nomenclature and classification of these tumors have been a matter of debate for more than a century, since their first description by Siegfried Oberdorfer. The last WHO classification provided a robust and easy-to-use tool to prognostically stratify GEP-NENs, based on morphological aspects and on proliferation rate. This review examines current approaches to the diagnosis and prognostic classification of GEP-NENs, focusing on the critical use of morphological parameters and immunohistochemical stainings, including diagnostic, site-specific and prognostic markers. The key issues of the current classification are addressed, including the emerging topics about cases with discordant morphology and proliferative index. Finally, we attempted to highlight the diagnostic pitfalls and the caveats in the use of immunohistochemical stains. Key Words: Neuroendocrine tumors, Gastrointestinal tract, Pancreas, Diagnosis BACKGROUND finding, as only neoplasms widely metastatic to the liver are associated with this syndrome (3, 4). Neuroendocrine neoplasms (NENs) are a heterogeneous group of epithelial neoplastic proliferations arising in The high heterogeneity of the biological and clinical features a large number of body organs. -

Oculoplastic Aspects of Ocular Oncology
Eye (2013) 27, 199–207 & 2013 Macmillan Publishers Limited All rights reserved 0950-222X/13 www.nature.com/eye Oculoplastic aspects C Rene CAMBRIDGE OPHTHALMOLOGICAL SYMPOSIUM of ocular oncology Abstract represents a significant proportion of the oculoplastic surgeon’s workload. In this review, It is estimated that 5–10% of all cutaneous the features of periocular skin cancer are malignancies involve the periocular region presented together with a discussion of the and management of periocular skin cancers treatment modalities. account for a significant proportion of the oculoplastic surgeon’s workload. Epithelial tumours are most frequently encountered, Diagnosing malignant eyelid disease including basal cell carcinoma, squamous cell carcinoma, and sebaceous gland Although malignant eyelid disease is usually carcinoma, in decreasing order of frequency. easy to diagnose on the basis of the history and Non-epithelial tumours, such as cutaneous clinical signs identified on careful examination melanoma and Merkel cell carcinoma, rarely (Table 1), differentiating between benign and involve the ocular adnexae. Although malignant periocular skin lesions can be non-surgical treatments for periocular challenging because malignant lesions malignancies are gaining in popularity, occasionally masquerade as benign pathology. surgery remains the main treatment modality For instance, a cystic basal cell carcinoma (BCC) 4,5 and has as its main aims tumour clearance, can resemble a hidrocystoma or sebaceous restoration of the eyelid function, protection gland carcinoma (SGC) classically mimics a 6,7 of the ocular surface, and achieving a good chalazion. Conversely, a benign lesion such as cosmetic outcome. The purpose of this article a pigmented hidrocystoma may be mistaken for 8 is to review the management of malignant a malignant melanoma. -

The 2020 WHO Classification of Soft Tissue Tumours: News and Perspectives
PATHOLOGICA 2021;113:70-84; DOI: 10.32074/1591-951X-213 Review The 2020 WHO Classification of Soft Tissue Tumours: news and perspectives Marta Sbaraglia1, Elena Bellan1, Angelo P. Dei Tos1,2 1 Department of Pathology, Azienda Ospedale Università Padova, Padova, Italy; 2 Department of Medicine, University of Padua School of Medicine, Padua, Italy Summary Mesenchymal tumours represent one of the most challenging field of diagnostic pathol- ogy and refinement of classification schemes plays a key role in improving the quality of pathologic diagnosis and, as a consequence, of therapeutic options. The recent publica- tion of the new WHO classification of Soft Tissue Tumours and Bone represents a major step toward improved standardization of diagnosis. Importantly, the 2020 WHO classi- fication has been opened to expert clinicians that have further contributed to underline the key value of pathologic diagnosis as a rationale for proper treatment. Several rel- evant advances have been introduced. In the attempt to improve the prediction of clinical behaviour of solitary fibrous tumour, a risk assessment scheme has been implemented. NTRK-rearranged soft tissue tumours are now listed as an “emerging entity” also in con- sideration of the recent therapeutic developments in terms of NTRK inhibition. This deci- sion has been source of a passionate debate regarding the definition of “tumour entity” as well as the consequences of a “pathology agnostic” approach to precision oncology. In consideration of their distinct clinicopathologic features, undifferentiated round cell sarcomas are now kept separate from Ewing sarcoma and subclassified, according to the underlying gene rearrangements, into three main subgroups (CIC, BCLR and not Received: October 14, 2020 ETS fused sarcomas) Importantly, In order to avoid potential confusion, tumour entities Accepted: October 19, 2020 such as gastrointestinal stroma tumours are addressed homogenously across the dif- Published online: November 3, 2020 ferent WHO fascicles. -

2016 Essentials of Dermatopathology Slide Library Handout Book
2016 Essentials of Dermatopathology Slide Library Handout Book April 8-10, 2016 JW Marriott Houston Downtown Houston, TX USA CASE #01 -- SLIDE #01 Diagnosis: Nodular fasciitis Case Summary: 12 year old male with a rapidly growing temple mass. Present for 4 weeks. Nodular fasciitis is a self-limited pseudosarcomatous proliferation that may cause clinical alarm due to its rapid growth. It is most common in young adults but occurs across a wide age range. This lesion is typically 3-5 cm and composed of bland fibroblasts and myofibroblasts without significant cytologic atypia arranged in a loose storiform pattern with areas of extravasated red blood cells. Mitoses may be numerous, but atypical mitotic figures are absent. Nodular fasciitis is a benign process, and recurrence is very rare (1%). Recent work has shown that the MYH9-USP6 gene fusion is present in approximately 90% of cases, and molecular techniques to show USP6 gene rearrangement may be a helpful ancillary tool in difficult cases or on small biopsy samples. Weiss SW, Goldblum JR. Enzinger and Weiss’s Soft Tissue Tumors, 5th edition. Mosby Elsevier. 2008. Erickson-Johnson MR, Chou MM, Evers BR, Roth CW, Seys AR, Jin L, Ye Y, Lau AW, Wang X, Oliveira AM. Nodular fasciitis: a novel model of transient neoplasia induced by MYH9-USP6 gene fusion. Lab Invest. 2011 Oct;91(10):1427-33. Amary MF, Ye H, Berisha F, Tirabosco R, Presneau N, Flanagan AM. Detection of USP6 gene rearrangement in nodular fasciitis: an important diagnostic tool. Virchows Arch. 2013 Jul;463(1):97-8. CONTRIBUTED BY KAREN FRITCHIE, MD 1 CASE #02 -- SLIDE #02 Diagnosis: Cellular fibrous histiocytoma Case Summary: 12 year old female with wrist mass. -

Rotana Alsaggaf, MS
Neoplasms and Factors Associated with Their Development in Patients Diagnosed with Myotonic Dystrophy Type I Item Type dissertation Authors Alsaggaf, Rotana Publication Date 2018 Abstract Background. Recent epidemiological studies have provided evidence that myotonic dystrophy type I (DM1) patients are at excess risk of cancer, but inconsistencies in reported cancer sites exist. The risk of benign tumors and contributing factors to tu... Keywords Cancer; Tumors; Cataract; Comorbidity; Diabetes Mellitus; Myotonic Dystrophy; Neoplasms; Thyroid Diseases Download date 07/10/2021 07:06:48 Link to Item http://hdl.handle.net/10713/7926 Rotana Alsaggaf, M.S. Pre-doctoral Fellow - Clinical Genetics Branch, Division of Cancer Epidemiology & Genetics, National Cancer Institute, NIH PhD Candidate – Department of Epidemiology & Public Health, University of Maryland, Baltimore Contact Information Business Address 9609 Medical Center Drive, 6E530 Rockville, MD 20850 Business Phone 240-276-6402 Emails [email protected] [email protected] Education University of Maryland – Baltimore, Baltimore, MD Ongoing Ph.D. Epidemiology Expected graduation: May 2018 2015 M.S. Epidemiology & Preventive Medicine Concentration: Human Genetics 2014 GradCert. Research Ethics Colorado State University, Fort Collins, CO 2009 B.S. Biological Science Minor: Biomedical Sciences 2009 Cert. Biomedical Engineering Interdisciplinary studies program Professional Experience Research Experience 2016 – present Pre-doctoral Fellow National Cancer Institute, National Institutes -

Case Report Perineal Lipoblastoma: a Case Report and Review of Literature
Int J Clin Exp Pathol 2014;7(6):3370-3374 www.ijcep.com /ISSN:1936-2625/IJCEP0000325 Case Report Perineal lipoblastoma: a case report and review of literature Qiang Liu1*, Zheng Xu1*, Shunbao Mao1, Rongyao Zeng1, Wenyou Chen1, Qiang Lu1, Yihe Guo2, Jing Liu1* 1Department of General Surgery, 175 Hospital of PLA (Affiliated Dongnan Hospital of Xiamen University), 269 Zhanghua Middle Road, Zhangzhou 363000, Fujian Province, China; 2Department of Pathology, 175 Hospital of PLA, 269 Zhanghua Middle Road, Zhangzhou 363000, Fujian Province, China. *Equal contributors. Received March 25, 2014; Accepted May 23, 2014; Epub May 15, 2014; Published June 1, 2014 Abstract: Lipoblastoma is a rare benign mesenchymal tumor that composes of embryonal white fat tissue and typi- cally occurs in infants or young children under 3 years of age. It usually affects the extremities, trunk, head, and neck. The perineum is a rare location with only 7 cases reported in the literature. We describe a case of 3-year-old girl with a lipoblastoma arising from perineum. An approximately 4.5 cm × 3.5 cm × 2.5 cm nodule was resected in left perineum with satisfied results. Pathological examination showed that it was composed of small lobules of mature and immature fat cells, separated by fibrous septa containing small dilated blood vessels. The left perineal lipoblastoma, although rare, should be differentiated from some other mesenchymal tumors with similar histologic and cytological features. Keywords: Perineum, lipoblastoma, myxoid liposarcoma, childhood, pathology Introduction Case report Lipoblastoma was first described by Jaffe in A 3-year-old girl was admitted to the Department 1926 [1].