Understanding Healthcare Self-Referral in Nigeria from The
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sustainability of the Niger State CDTI Project, Nigeria
l- World Health Organization African Programme for Onchocerciasis Control FINAL RËPOftî ,i ={ Evaluation of the Sustainability of the Niger State CDTI Project, Nigeria N ove m ber- Decem ber 2004 Elizabeth Elhassan (Team Leader) Uwem Ekpo Paul Kolo William Kisoka Abraraw Tefaye Hilary Adie f'Ï 'rt\ t- I I I TABLE OF CONTENTS I Table of contents............. ..........2 Abbreviations/Acronyms ................ ........ 3 Acknowledgements .................4 Executive Summary .................5 *? 1. lntroduction ...........8 2. Methodology .........9 2.1 Sampling ......9 2.2 Levels and lnstruments ..............10 2.3 Protocol ......10 2.4 Team Composition ........... ..........11 2.5 Advocacy Visits and 'Feedback/Planning' Meetings........ ..........12 2.6 Limitations ..................12 3. Major Findings And Recommendations ........ .................. 13 3.1 State Level .....13 3.2 Local Government Area Level ........21 3.3 Front Line Health Facility Level ......27 3.4 Community Level .............. .............32 4. Conclusions ..........36 4.1 Grading the Overall Sustainability of the Niger State CDTI project.................36 4.2 Grading the Project as a whole .......39 ANNEXES .................40 lnterviews ..............40 Schedule for the Evaluation and Advocacy.......... .................42 Feedback and Planning Meetings, Agenda.............. .............44 Report of the Feedbacl</Planning Meetings ..........48 Strengths And Weaknesses Of The Niger State Cdti Project .. .. ..... 52 Participants Attendance List .......57 Abbrevi -

Success Stories Nigeria Kaduna and Niger State
Success Stories - Nigeria 2019 SUCCESS STORIES NIGERIA KADUNA AND NIGER STATE 1 Success Stories - Nigeria 2019 Story 1: PASSAGE AND ASSENT OF THE NIGERIAN AGRICULTURAL SEEDS COUNCIL BILL eed system security is one the top priorities of AGRA as an organization that drives agricultural productivity in Africa. Following the declined assent of the Nigerian Agricultural Seeds Council Bill by President Muhammadu Buhari; AGRA approached SNESG and formed a partnership with a focus on systems approach to advocate for the passage and assent of three critical Bills to create an enabling business environment 2018 NG 001: within the agriculture sector. To drive the advocacy pro- cess, economic impact analysis/ impact assessment of Advocacy for the the three Bills was conducted which shaped the evi- passage of the dence-based policy briefs and other digital and traditional fertilizer quality control advocacy assets utilized. A mapping of Stakeholders was bill, Nigerian independent done to differentiate the policy cluster, operational clus- ter/implementers and beneficiaries who had power to in- warehouse receipt system bill fluence the passage and assent of the three Bills. and the presidential assent of the National Agricultural Seed Sensitization was conveyed across 5 geo-political zones Council bill. in Nigeria to sensitize smallholder farmers on the impera- tives & impact of the Bills. Support and buy-in was garnered from players across different sectors, agro-allied companies and private & public development organizations with interest in the Bills. Traditional and social media campaigns on the three Bills commenced in November, 2018 and the momentum is currently sustained. To further deepen engagement with the Legislature and the Executive; one-on-one consultative ad- vocacy meetings was held between the NESG-National Assembly Business Environment Roundtable (NASSBER) and the Clerks of the Committees that presided over the Bills. -

Socio-Economic Survey, 2014
NIGER STATE BUREAU OF STATISTICS (WITH TECHNICAL SUPPORT OF THE NATIONAL BUREAU OF STATISTICS) SOCIO-ECONOMIC SURVEY, 2014 Niger State Bureau of Statistics (NSBS) www.nigerstats.ni.gov.ng E-mail: [email protected] SOCIO-ECONOMIC SURVEY, 2014 NIGER STATE BUREAU OF STATISTICS ii SOCIO-ECONOMIC SURVEY, 2014 Table of Contents VISION AND MISSION STATEMENTS OF NIGER STATE BUREAU OF 1.16 Data Processing and Analysis ........................................ 4 STATISTICS (NSBS) ...............................................................................viii 1.17 Tabulation Plan ...............................................................4 Vision .......................................................................................................viii 1.18 Report Writing .................................................................4 Mission ....................................................................................................viii FOREWORD ............................................................................................. ix CHAPTER TWO .........................................................................................5 ACKNOWLEDGEMENT ............................................................................ x HOUSEHOLD CHARACTERISTICS ..........................................................5 BRIEF NOTE ON NIGER STATE .............................................................. xi 2.1 Average Household Size ................................................5 CHAPTER ONE .........................................................................................1 -

LGA Agale Agwara Bida Borgu Bosso Chanchaga Edati Gbako Gurara
LGA Agale Agwara Bida Borgu Bosso Chanchaga Edati Gbako Gurara Katcha Kontagora Lapai Lavun Magama Mariga Mashegu Mokwa Munya Paikoro Rafi Rijau Shiroro Suleja Tafa Wushishi PVC PICKUP ADDRESS Santali Road, After Lga Secretariat, Agaie Opposite Police Station, Along Agwara-Borgu Road, Agwara Lga Umaru Magajib Ward, Yahayas, Dangana Way, Bida Lga Borgu Lga New Bussa, Niger Along Leg Road, Opp. Baband Abo Primary/Junior Secondary Schoo, Near Divisional Police Station, Maikunkele, Bosso Lga Along Niger State Houseso Assembly Quarters, Western Byepass, Minna Opposite Local Govt. Secretariat Road Edati Lga, Edati Along Bida-Zungeru Road, Gbako Lga, Lemu Gwadene Primary School, Gawu Babangida Gangiarea, Along Loga Secretariat, Katcha Katcha Lga Near Hamdala Motors, Along Kontagora-Yauri Road, Kontagoa Along Minna Road, Beside Pension Office, Lapai Opposite Plice Station, Along Bida-Mokwa Road, Lavun Off Lga Secretariat Road, Magama Lga, Nasko Unguwan Sarki, Opposite Central Mosque Bangi Adogu, Near Adogu Primary School, Mashegu Off Agric Road, Mokwa Lga Munya Lga, Sabon Bari Sarkin Pawa Along Old Abuja Road, Adjacent Uk Bello Primary School, Paikoro Behind Police Barracks, Along Lagos-Kaduna Road, Rafi Lga, Kagara Dirin-Daji/Tungan Magajiya Road, Junction, Rijau Anguwan Chika- Kuta, Near Lag Secretariat, Gussoroo Road, Kuta Along Suleja Minna Road, Opp. Suleman Barau Technical Collage, Kwamba Beside The Div. Off. Station, Along Kaduna-Abuja Express Road, Sabo-Wuse, Tafa Lga Women Centre, Behind Magistration Court, Along Lemu-Gida Road, Wushishi. Along Leg Road, Opp. Baband Abo Primary/Junior Secondary Schoo, Near Divisional Police Station, Maikunkele, Bosso Lga. -

Evaluation of the Effect of Flooding on Danchitagi Community of Lavun Local Government Area, Niger State, Nigeria
Hummingbird Publications © December, HP Journal of Env. Design & Constructions Mgt. 2019 www.hummingpubng.com Vol. 19 No. 4 JECM 2019 Evaluation of the Effect of Flooding on Danchitagi Community of Lavun Local Government Area, Niger State, Nigeria M. A. Emigilati 1 Abdulkadir Nasiru 2 Department of Geography, Federal University of Technology, Minna – Niger State, Nigeria. Keyword: Abstract Niger State and precisely Danchitagi community in Danchitagi Lavun Local Government Area will continue to labour community, under the pains of flood disaster unless there is a Flooding, radical approach to avert the disaster. The aim of this farmland and study was to evaluate the effects of flooding on Lavun Danchitagi community in Lavun Local Government Area of Niger State, Nigeria. The researcher randomly distributed 355 household questionnaires while the instrument of in-depth interviews schedule was administered to the respondents. Frequency percentage statistics was utilized for data analysis and presentation. The finding shows that 193 (54.4%) of the respondents believed that the main cause of flood in the study area is from heavy rainfall, 148 (41.7%) of the respondents agreed that the main cause of flooding is due to flood plain development, poor drainage system ranked third with 13 (3.7%) of the respondents and blockage in the drainage ranked the least with one respondent. The results also shows that about 341 (96.1%) of the respondents said that their farmlands were being affected by flood while 14 (3.9%) said their farmlands were not being affected by flood since their farmlands were located far away from flood plain. Loss Page 103 of 322 JECM Vol. -

Nigeria's Constitution of 1999
PDF generated: 26 Aug 2021, 16:42 constituteproject.org Nigeria's Constitution of 1999 This complete constitution has been generated from excerpts of texts from the repository of the Comparative Constitutions Project, and distributed on constituteproject.org. constituteproject.org PDF generated: 26 Aug 2021, 16:42 Table of contents Preamble . 5 Chapter I: General Provisions . 5 Part I: Federal Republic of Nigeria . 5 Part II: Powers of the Federal Republic of Nigeria . 6 Chapter II: Fundamental Objectives and Directive Principles of State Policy . 13 Chapter III: Citizenship . 17 Chapter IV: Fundamental Rights . 20 Chapter V: The Legislature . 28 Part I: National Assembly . 28 A. Composition and Staff of National Assembly . 28 B. Procedure for Summoning and Dissolution of National Assembly . 29 C. Qualifications for Membership of National Assembly and Right of Attendance . 32 D. Elections to National Assembly . 35 E. Powers and Control over Public Funds . 36 Part II: House of Assembly of a State . 40 A. Composition and Staff of House of Assembly . 40 B. Procedure for Summoning and Dissolution of House of Assembly . 41 C. Qualification for Membership of House of Assembly and Right of Attendance . 43 D. Elections to a House of Assembly . 45 E. Powers and Control over Public Funds . 47 Chapter VI: The Executive . 50 Part I: Federal Executive . 50 A. The President of the Federation . 50 B. Establishment of Certain Federal Executive Bodies . 58 C. Public Revenue . 61 D. The Public Service of the Federation . 63 Part II: State Executive . 65 A. Governor of a State . 65 B. Establishment of Certain State Executive Bodies . -

Focus on Niger State Housing Corportation – Being an Article for Journal Publication In
Housing Today: The Journal of the Association of Housing Corporations of Nigeria, Volume 8, No. 3, November 1992, Pp. 62-70 FOCUS ON NIGER STATE HOUSING CORPORATION (N.S.H.C.) Mohammed, A.; Bobi, M.T.; Minin, U.; Babalola, O.; Shaaba, A.P.; Namagana, N.M.; Olukade, I.J. and Bako, M.D. @Niger State Housing Corporation, P.M.B 105 Minna, Niger State, Nigeria Abstract: Established in 1979, Niger State Housing Corporation (NSHC)had the primary responsibility to address qualitative and quantitative housing inadequacy in Niger State, thereby enhancing the standard of living of her citizens, this article with the aim of elucidating the activities of the Corporation for performance rating , has the objectives to examine its consultancy and contracting services, and to assess its home ownership and other programmes. The methodology adopted for the study was the qualitative research design method which provides description of case studies with purposive sampling, hence the analyses also. The results of the study concluded that the NSHC’s performance from inception to date has been very satisfactory, and recommended that the Corporation enhances its programmes and continue to discharge its responsibilities to Nigerian citizens in the State with more enlightenment about its activities. Keywords: Consultancy, contracting, direct-labor, housing, tenure. ARTICLE OUTLINE Alhaji Isa Mohammed Kagara was 1.0 Introduction appointed secretary. They were replaced in 2.0 Relevant Review Works November, 1984, by Arc. Mustapha 3.0 Research Methodology Zubairu and Alhaji Mohammed Isa Ekkan 4.0 Data Presentation, Analyses and Discussion respectively, in September 1990 Mallam 5.0 Conclusion Mohammed Tukur Bobi was appointed the References new Secretary of the Corporation. -

Impact of Tungan-Kawo Irrigation Scheme on Rice Production in Wushishi Local Government Area, Niger State, Nigeria Ibrahim Jalal
African Scholar VOL. 17 NO. 1 Publications & ISSN: 2877-1990 Research MARCH, 2020 International African Scholar Journal of Agriculture and Agricultural Tech. (JAAT-1) Impact of Tungan-Kawo Irrigation Scheme on Rice Production in Wushishi Local Government Area, Niger State, Nigeria Ibrahim Jalaludeen S., M. B. Yunusa PhD & M.A. Emigilati PhD Department of Geography Federal University of Technology Minna, Nigeria Abstract This study seek to examine the impact of Tungan-kawo irrigation scheme on rice production in Wushishi Local Government Area, Niger state, Nigeria. Tara Yamane’s sampling technique was used to derive 400 farmers/respondents from the population of the study. Data was collected through the use of structured questionnaires which was subjected to analysis using frequencies, percentages and Pearson’s product-moment correlation coefficient of multiple regression analysis. From a response rate of 91.75% deduced, about 66.8% of the farmers were between the age of 18 to 38 years. This portends an indication that there is opportunity for more active years in agricultural activities. The study revealed that 93% of respondents were male. The marital status of farmers involved in the study indicated that 92.1% were married. The level of educational qualification of respondents was highly appreciated as a substantial number of them had formal education, where 52.9% had tertiary education. 87.5% of the respondents embrace farming as a major occupation. Within the demographic characteristics of the farmers, 70.0% of respondents had household size of 6 to 10. Farmers average experience in paddy production was recorded to be 11-20 years while findings showed that ownership type of land cultivated was majorly through inheritance and rentage with an average farm size of 5 acres. -
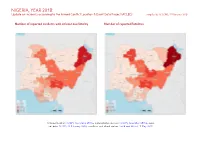
NIGERIA, YEAR 2018: Update on Incidents According to the Armed Conflict Location & Event Data Project (ACLED) Compiled by ACCORD, 25 February 2020
NIGERIA, YEAR 2018: Update on incidents according to the Armed Conflict Location & Event Data Project (ACLED) compiled by ACCORD, 25 February 2020 Number of reported incidents with at least one fatality Number of reported fatalities National borders: GADM, November 2015a; administrative divisions: GADM, November 2015b; incid- ent data: ACLED, 22 February 2020; coastlines and inland waters: Smith and Wessel, 1 May 2015 NIGERIA, YEAR 2018: UPDATE ON INCIDENTS ACCORDING TO THE ARMED CONFLICT LOCATION & EVENT DATA PROJECT (ACLED) COMPILED BY ACCORD, 25 FEBRUARY 2020 Contents Conflict incidents by category Number of Number of reported fatalities 1 Number of Number of Category incidents with at incidents fatalities Number of reported incidents with at least one fatality 1 least one fatality Violence against civilians 705 566 2853 Conflict incidents by category 2 Battles 474 373 2470 Development of conflict incidents from 2009 to 2018 2 Protests 427 3 3 Riots 213 61 154 Methodology 3 Strategic developments 117 3 4 Conflict incidents per province 4 Explosions / Remote 100 84 759 violence Localization of conflict incidents 4 Total 2036 1090 6243 Disclaimer 8 This table is based on data from ACLED (datasets used: ACLED, 22 February 2020). Development of conflict incidents from 2009 to 2018 This graph is based on data from ACLED (datasets used: ACLED, 22 February 2020). 2 NIGERIA, YEAR 2018: UPDATE ON INCIDENTS ACCORDING TO THE ARMED CONFLICT LOCATION & EVENT DATA PROJECT (ACLED) COMPILED BY ACCORD, 25 FEBRUARY 2020 Methodology on what level of detail is reported. Thus, towns may represent the wider region in which an incident occured, or the provincial capital may be used if only the province The data used in this report was collected by the Armed Conflict Location & Event is known. -

International Journal of Language, Literature and Gender Studies (LALIGENS), Bahir Dar- Ethiopia Vol
1 LALIGENS, VOL. 8(2), S/N 18, AUGUST/SEPT., 2019 International Journal of Language, Literature and Gender Studies (LALIGENS), Bahir Dar- Ethiopia Vol. 8 (2), Serial No 18, August/Sept., 2019:1-12 ISSN: 2225-8604(Print) ISSN 2227-5460 (Online) DOI: http://dx.doi.org/10.4314/laligens.v8i2.1 BABEL OF NIGER STATE 1IHENACHO, A. A., JAMIU, A. M., AGU, M. N., EBINE, S. A., ADELABU, S. & OBI, E. F. Faculty of Languages and Communication Studies IBB University, Lapai, Niger State, Nigeria 1+2348127189382 [email protected] Abstract This paper is a preliminary report on an ongoing research being carried out in the Faculty of Languages and Communication Studies of Ibrahim Badamasi Babangida University, Lapai, Niger State, Nigeria. The research is on ‘Language education and translation in Niger State’. The languages involved in the research are: Arabic, English, French, Gbagyi, Hausa and Nupe. The aim of this research which is funded by the Nigerian Tertiary Education Trust Fund (TETFund) is ‘to help improve the outcome of language education and translation in Niger State in both quality and quantity’ As a preliminary inquiry, the research team visited 78 institutions of learning at all levels (primary, secondary and tertiary) in all the three geopolitical zones of Niger State, as well as media houses located in the capital, Minna, and obtained responses to the questionnaires they took to the institutions. While pursuing the aim and objectives of their main research, the team deemed it necessary to consider the position (and the plight) of the multiplicity of other languages of Niger State (than the three major ones – Gbagyi, Hausa and Nupe) in relation to Nigeria’s language policy in education. -
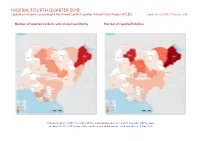
NIGERIA, FOURTH QUARTER 2018: Update on Incidents According to the Armed Conflict Location & Event Data Project (ACLED) Compiled by ACCORD, 25 February 2020
NIGERIA, FOURTH QUARTER 2018: Update on incidents according to the Armed Conflict Location & Event Data Project (ACLED) compiled by ACCORD, 25 February 2020 Number of reported incidents with at least one fatality Number of reported fatalities National borders: GADM, November 2015a; administrative divisions: GADM, November 2015b; incid- ent data: ACLED, 22 February 2020; coastlines and inland waters: Smith and Wessel, 1 May 2015 NIGERIA, FOURTH QUARTER 2018: UPDATE ON INCIDENTS ACCORDING TO THE ARMED CONFLICT LOCATION & EVENT DATA PROJECT (ACLED) COMPILED BY ACCORD, 25 FEBRUARY 2020 Contents Conflict incidents by category Number of Number of reported fatalities 1 Number of Number of Category incidents with at incidents fatalities Number of reported incidents with at least one fatality 1 least one fatality Battles 124 82 753 Conflict incidents by category 2 Violence against civilians 113 65 276 Development of conflict incidents from December 2016 to December 2018 2 Protests 79 0 0 Riots 50 8 58 Methodology 3 Strategic developments 34 0 0 Conflict incidents per province 4 Explosions / Remote 18 16 107 violence Localization of conflict incidents 4 Total 418 171 1194 Disclaimer 7 This table is based on data from ACLED (datasets used: ACLED, 22 February 2020). Development of conflict incidents from December 2016 to December 2018 This graph is based on data from ACLED (datasets used: ACLED, 22 February 2020). 2 NIGERIA, FOURTH QUARTER 2018: UPDATE ON INCIDENTS ACCORDING TO THE ARMED CONFLICT LOCATION & EVENT DATA PROJECT (ACLED) COMPILED BY ACCORD, 25 FEBRUARY 2020 Methodology on what level of detail is reported. Thus, towns may represent the wider region in which an incident occured, or the provincial capital may be used if only the province The data used in this report was collected by the Armed Conflict Location & Event is known. -

Oral Literature Genres of the Nupe of Central Nigeria
Oral literature genres of the Nupe of Central Nigeria [DRAFT CIRCULATED FOR COMMENT] Roger Blench Kay Williamson Educational Foundation 8, Guest Road Cambridge CB1 2AL United Kingdom Voice/Ans 0044-(0)1223-560687 Mobile worldwide (00-44)-(0)7967-696804 E-mail [email protected] http://www.rogerblench.info/RBOP.htm This printout: July 16, 2010 Roger Blench Nupe oral literature genres Circulated for comment TABLE OF CONTENTS 1. INTRODUCTION: BACKGROUND TO NIGERIA.............................................................................. 1 2. THE NUPE PEOPLE ................................................................................................................................. 2 3. THE NUPE LANGUAGE .......................................................................................................................... 3 4. WRITTEN FORMS OF NUPE LITERATURE GENRES..................................................................... 5 4.1 Arabic script literature..........................................................................................................................................5 4.2 Roman script literature .........................................................................................................................................6 5. NUPE ORAL LITERATURE GENRES................................................................................................... 8 5.1 General....................................................................................................................................................................8