Georgia's Newborn Screening Panel (Disorders)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ovulation-Selective Genes: the Generation and Characterization of an Ovulatory-Selective Cdna Library
531 Ovulation-selective genes: the generation and characterization of an ovulatory-selective cDNA library A Hourvitz1,2*, E Gershon2*, J D Hennebold1, S Elizur2, E Maman2, C Brendle1, E Y Adashi1 and N Dekel2 1Division of Reproductive Sciences, Department of Obstetrics and Gynecology, University of Utah Health Sciences Center, Salt Lake City, Utah 84132, USA 2Department of Biological Regulation, Weizmann Institute of Science, Rehovot, Israel (Requests for offprints should be addressed to N Dekel; Email: [email protected]) *(A Hourvitz and E Gershon contributed equally to this paper) (J D Hennebold is now at Division of Reproductive Sciences, Oregon National Primate Research Center, Oregon Health and Science University, Beaverton, Oregon 97006, USA) Abstract Ovulation-selective/specific genes, that is, genes prefer- (FAE-1) homolog, found to be localized to the inner entially or exclusively expressed during the ovulatory periantral granulosa and to the cumulus granulosa cells of process, have been the subject of growing interest. We antral follicles. The FAE-1 gene is a -ketoacyl-CoA report herein studies on the use of suppression subtractive synthase belonging to the fatty acid elongase (ELO) hybridization (SSH) to construct a ‘forward’ ovulation- family, which catalyzes the initial step of very long-chain selective/specific cDNA library. In toto, 485 clones were fatty acid synthesis. All in all, the present study accom- sequenced and analyzed for homology to known genes plished systematic identification of those hormonally with the basic local alignment tool (BLAST). Of those, regulated genes that are expressed in the ovary in an 252 were determined to be nonredundant. -

Mapping Influenza-Induced Posttranslational Modifications On
viruses Article Mapping Influenza-Induced Posttranslational Modifications on Histones from CD8+ T Cells Svetlana Rezinciuc 1, Zhixin Tian 2, Si Wu 2, Shawna Hengel 2, Ljiljana Pasa-Tolic 2 and Heather S. Smallwood 1,3,* 1 Department of Pediatrics, University of Tennessee Health Science Center, Memphis, TN 38163, USA; [email protected] 2 Environmental Molecular Sciences Laboratory, Pacific Northwest National Laboratory, Richland, WA 99354, USA; [email protected] (Z.T.); [email protected] (S.W.); [email protected] (S.H.); [email protected] (L.P.-T.) 3 Children’s Foundation Research Institute, Memphis, TN 38105, USA * Correspondence: [email protected]; Tel.: +1-(901)-448–3068 Academic Editor: Italo Tempera Received: 10 October 2020; Accepted: 2 December 2020; Published: 8 December 2020 Abstract: T cell function is determined by transcriptional networks that are regulated by epigenetic programming via posttranslational modifications (PTMs) to histone proteins and DNA. Bottom-up mass spectrometry (MS) can identify histone PTMs, whereas intact protein analysis by MS can detect species missed by bottom-up approaches. We used a novel approach of online two-dimensional liquid chromatography-tandem MS with high-resolution reversed-phase liquid chromatography (RPLC), alternating electron transfer dissociation (ETD) and collision-induced dissociation (CID) on precursor ions to maximize fragmentation of uniquely modified species. The first online RPLC separation sorted histone families, then RPLC or weak cation exchange hydrophilic interaction liquid chromatography (WCX-HILIC) separated species heavily clad in PTMs. Tentative identifications were assigned by matching proteoform masses to predicted theoretical masses that were verified with tandem MS. We used this innovative approach for histone-intact protein PTM mapping (HiPTMap) to identify and quantify proteoforms purified from CD8 T cells after in vivo influenza infection. -

Supplement 1 Overview of Dystonia Genes
Supplement 1 Overview of genes that may cause dystonia in children and adolescents Gene (OMIM) Disease name/phenotype Mode of inheritance 1: (Formerly called) Primary dystonias (DYTs): TOR1A (605204) DYT1: Early-onset generalized AD primary torsion dystonia (PTD) TUBB4A (602662) DYT4: Whispering dystonia AD GCH1 (600225) DYT5: GTP-cyclohydrolase 1 AD deficiency THAP1 (609520) DYT6: Adolescent onset torsion AD dystonia, mixed type PNKD/MR1 (609023) DYT8: Paroxysmal non- AD kinesigenic dyskinesia SLC2A1 (138140) DYT9/18: Paroxysmal choreoathetosis with episodic AD ataxia and spasticity/GLUT1 deficiency syndrome-1 PRRT2 (614386) DYT10: Paroxysmal kinesigenic AD dyskinesia SGCE (604149) DYT11: Myoclonus-dystonia AD ATP1A3 (182350) DYT12: Rapid-onset dystonia AD parkinsonism PRKRA (603424) DYT16: Young-onset dystonia AR parkinsonism ANO3 (610110) DYT24: Primary focal dystonia AD GNAL (139312) DYT25: Primary torsion dystonia AD 2: Inborn errors of metabolism: GCDH (608801) Glutaric aciduria type 1 AR PCCA (232000) Propionic aciduria AR PCCB (232050) Propionic aciduria AR MUT (609058) Methylmalonic aciduria AR MMAA (607481) Cobalamin A deficiency AR MMAB (607568) Cobalamin B deficiency AR MMACHC (609831) Cobalamin C deficiency AR C2orf25 (611935) Cobalamin D deficiency AR MTRR (602568) Cobalamin E deficiency AR LMBRD1 (612625) Cobalamin F deficiency AR MTR (156570) Cobalamin G deficiency AR CBS (613381) Homocysteinuria AR PCBD (126090) Hyperphelaninemia variant D AR TH (191290) Tyrosine hydroxylase deficiency AR SPR (182125) Sepiaterine reductase -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -

Biotin Rescues Mitochondrial Dysfunction and Neurotoxicity in a Tauopathy Model
Biotin rescues mitochondrial dysfunction and neurotoxicity in a tauopathy model Kelly M. Lohra,b, Bess Frostc, Clemens Scherzerd, and Mel B. Feanya,1 aDepartment of Pathology, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA 02115; bDepartment of Biology, Washington & Jefferson College, Washington, PA 15301; cDepartment of Cell Systems and Anatomy, University of Texas Health Science Center at San Antonio, San Antonio, TX 78229; and dNeurogenomics Laboratory, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA 02115 Edited by Solomon H. Snyder, Johns Hopkins University School of Medicine, Baltimore, MD, and approved September 17, 2020 (received for review December 21, 2019) Mitochondrial and metabolic dysfunction are often implicated in We combined Drosophila genetics with a variety of molecular neurological disease, but effective mechanism-based therapies re- and cellular approaches to explore the role of mitochondrial and main elusive. We performed a genome-scale forward genetic metabolic pathways in tauopathy and neuronal survival. We screen in a Drosophila model of tauopathy, a class of neurodegen- identified dysfunction within the biotin pathway in tauopathy and erative disorders characterized by the accumulation of the protein showed that biotin supplementation both rescues mitochondrial tau, and identified manipulation of the B-vitamin biotin as a po- deficits and improves neuronal health in vivo. Furthermore, we tential therapeutic approach in tauopathy. We show that tau demonstrate parallel mechanisms in human Alzheimer’s disease transgenic flies have an innate biotin deficiency due to tau-medi- brain. Together, these findings emphasize the importance of ated relaxation of chromatin and consequent aberrant expression biotin handling in mitochondrial and metabolic processes in of multiple biotin-related genes, disrupting both carboxylase and neurons, suggesting a key role for biotin in both the healthy and mitochondrial function. -

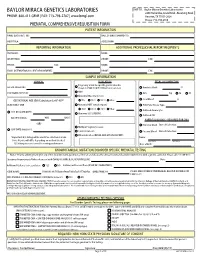
Molecular Diagnostic Requisition
BAYLOR MIRACA GENETICS LABORATORIES SHIP TO: Baylor Miraca Genetics Laboratories 2450 Holcombe, Grand Blvd. -Receiving Dock PHONE: 800-411-GENE | FAX: 713-798-2787 | www.bmgl.com Houston, TX 77021-2024 Phone: 713-798-6555 MOLECULAR DIAGNOSTIC REQUISITION PATIENT INFORMATION SAMPLE INFORMATION NAME: DATE OF COLLECTION: / / LAST NAME FIRST NAME MI MM DD YY HOSPITAL#: ACCESSION#: DATE OF BIRTH: / / GENDER (Please select one): FEMALE MALE MM DD YY SAMPLE TYPE (Please select one): ETHNIC BACKGROUND (Select all that apply): UNKNOWN BLOOD AFRICAN AMERICAN CORD BLOOD ASIAN SKELETAL MUSCLE ASHKENAZIC JEWISH MUSCLE EUROPEAN CAUCASIAN -OR- DNA (Specify Source): HISPANIC NATIVE AMERICAN INDIAN PLACE PATIENT STICKER HERE OTHER JEWISH OTHER (Specify): OTHER (Please specify): REPORTING INFORMATION ADDITIONAL PROFESSIONAL REPORT RECIPIENTS PHYSICIAN: NAME: INSTITUTION: PHONE: FAX: PHONE: FAX: NAME: EMAIL (INTERNATIONAL CLIENT REQUIREMENT): PHONE: FAX: INDICATION FOR STUDY SYMPTOMATIC (Summarize below.): *FAMILIAL MUTATION/VARIANT ANALYSIS: COMPLETE ALL FIELDS BELOW AND ATTACH THE PROBAND'S REPORT. GENE NAME: ASYMPTOMATIC/POSITIVE FAMILY HISTORY: (ATTACH FAMILY HISTORY) MUTATION/UNCLASSIFIED VARIANT: RELATIONSHIP TO PROBAND: THIS INDIVIDUAL IS CURRENTLY: SYMPTOMATIC ASYMPTOMATIC *If family mutation is known, complete the FAMILIAL MUTATION/ VARIANT ANALYSIS section. NAME OF PROBAND: ASYMPTOMATIC/POPULATION SCREENING RELATIONSHIP TO PROBAND: OTHER (Specify clinical findings below): BMGL LAB#: A COPY OF ORIGINAL RESULTS ATTACHED IF PROBAND TESTING WAS PERFORMED AT ANOTHER LAB, CALL TO DISCUSS PRIOR TO SENDING SAMPLE. A POSITIVE CONTROL MAY BE REQUIRED IN SOME CASES. REQUIRED: NEW YORK STATE PHYSICIAN SIGNATURE OF CONSENT I certify that the patient specified above and/or their legal guardian has been informed of the benefits, risks, and limitations of the laboratory test(s) requested. -

Neonatal Screening in Sweden and Disease-Causing Variants in Phenylketonuria, Galactosaemia and Biotinidase Deficiency
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Publications from Karolinska Institutet From the DEPARTMENT OF MEDICAL BIOCHEMISTRY AND BIOPHYSICS Karolinska Institutet, Stockholm, Sweden NEONATAL SCREENING IN SWEDEN AND DISEASE-CAUSING VARIANTS IN PHENYLKETONURIA, GALACTOSAEMIA AND BIOTINIDASE DEFICIENCY Annika Ohlsson Stockholm 2016 All previously published papers were reproduced with the permission of the publisher. Published by Karolinska Institutet. Printed by E-print AB 2016 © Annika Ohlsson, 2016 ISBN 978-91-7676-459-6 NEONATAL SCREENING IN SWEDEN AND DISEASE-CAUSING VARIANTS IN PHENYLKETONURIA, GALACTOSAEMIA AND BIOTINIDASE DEFICIENCY THESIS FOR DOCTORAL DEGREE (Ph.D.) By Annika Ohlsson Principal Supervisor: Opponent: Associate Professor Ulrika von Döbeln Professor Ola Hjalmarsson Karolinska Institute University of Gothenburg Department of Medical Biochemistry and Sahlgrenska Academy Biophysics Department of Pediatrics Division of Molecular Metabolism Examination Board: Co-supervisor: Professor Olle Söder Professor Anna Wedell Karolinska Institute Karolinska Institute Department of Women´s and Children´s Health Department of Molecular Medicine and Surgery Division of Pediatric Endocrinology Division of Inborn Errors of Endocrinology and Metabolism Associate Professor Cecilia Gunnarsson University of Linköping Department of Clinical and Experimental Medicine Division of Cell Biology Professor Lena Hjelte Karolinska Institute Department of Clinical Science, Intervention and Technology Division of Pediatrics To Urban, Sofie and Mathias ‘Success is not the key to happiness. Happiness is the key to success. If you love what you are doing, you will be successful.’ Herman Cain ABSTRACT Sweden celebrated 50 years of newborn screening (NBS) in 2015 and more than 2000 infants have benefitted from the programme. -
Prenatal Testing Requisition Form
BAYLOR MIRACA GENETICS LABORATORIES SHIP TO: Baylor Miraca Genetics Laboratories 2450 Holcombe, Grand Blvd. -Receiving Dock PHONE: 800-411-GENE | FAX: 713-798-2787 | www.bmgl.com Houston, TX 77021-2024 Phone: 713-798-6555 PRENATAL COMPREHENSIVE REQUISITION FORM PATIENT INFORMATION NAME (LAST,FIRST, MI): DATE OF BIRTH (MM/DD/YY): HOSPITAL#: ACCESSION#: REPORTING INFORMATION ADDITIONAL PROFESSIONAL REPORT RECIPIENTS PHYSICIAN: NAME: INSTITUTION: PHONE: FAX: PHONE: FAX: NAME: EMAIL (INTERNATIONAL CLIENT REQUIREMENT): PHONE: FAX: SAMPLE INFORMATION CLINICAL INDICATION FETAL SPECIMEN TYPE Pregnancy at risk for specific genetic disorder DATE OF COLLECTION: (Complete FAMILIAL MUTATION information below) Amniotic Fluid: cc AMA PERFORMING PHYSICIAN: CVS: mg TA TC Abnormal Maternal Screen: Fetal Blood: cc GESTATIONAL AGE (GA) Calculation for AF-AFP* NTD TRI 21 TRI 18 Other: SELECT ONLY ONE: Abnormal NIPT (attach report): POC/Fetal Tissue, Type: TRI 21 TRI 13 TRI 18 Other: Cultured Amniocytes U/S DATE (MM/DD/YY): Abnormal U/S (SPECIFY): Cultured CVS GA ON U/S DATE: WKS DAYS PARENTAL BLOODS - REQUIRED FOR CMA -OR- Maternal Blood Date of Collection: Multiple Pregnancy Losses LMP DATE (MM/DD/YY): Parental Concern Paternal Blood Date of Collection: Other Indication (DETAIL AND ATTACH REPORT): *Important: U/S dating will be used if no selection is made. Name: Note: Results will differ depending on method checked. Last Name First Name U/S dating increases overall screening performance. Date of Birth: KNOWN FAMILIAL MUTATION/DISORDER SPECIFIC PRENATAL TESTING Notice: Prior to ordering testing for any of the disorders listed, you must call the lab and discuss the clinical history and sample requirements with a genetic counselor. -

Downloaded from the App Store and Nucleobase, Nucleotide and Nucleic Acid Metabolism 7 Google Play
Hoytema van Konijnenburg et al. Orphanet J Rare Dis (2021) 16:170 https://doi.org/10.1186/s13023-021-01727-2 REVIEW Open Access Treatable inherited metabolic disorders causing intellectual disability: 2021 review and digital app Eva M. M. Hoytema van Konijnenburg1†, Saskia B. Wortmann2,3,4†, Marina J. Koelewijn2, Laura A. Tseng1,4, Roderick Houben6, Sylvia Stöckler‑Ipsiroglu5, Carlos R. Ferreira7 and Clara D. M. van Karnebeek1,2,4,8* Abstract Background: The Treatable ID App was created in 2012 as digital tool to improve early recognition and intervention for treatable inherited metabolic disorders (IMDs) presenting with global developmental delay and intellectual disabil‑ ity (collectively ‘treatable IDs’). Our aim is to update the 2012 review on treatable IDs and App to capture the advances made in the identifcation of new IMDs along with increased pathophysiological insights catalyzing therapeutic development and implementation. Methods: Two independent reviewers queried PubMed, OMIM and Orphanet databases to reassess all previously included disorders and therapies and to identify all reports on Treatable IDs published between 2012 and 2021. These were included if listed in the International Classifcation of IMDs (ICIMD) and presenting with ID as a major feature, and if published evidence for a therapeutic intervention improving ID primary and/or secondary outcomes is avail‑ able. Data on clinical symptoms, diagnostic testing, treatment strategies, efects on outcomes, and evidence levels were extracted and evaluated by the reviewers and external experts. The generated knowledge was translated into a diagnostic algorithm and updated version of the App with novel features. Results: Our review identifed 116 treatable IDs (139 genes), of which 44 newly identifed, belonging to 17 ICIMD categories. -

Disorders Alphabetical by Disease Updated 1/2020
Disorders Alphabetical by Disease updated 1/2020 Disorders Abbreviation Classification Recommended Uniform Screening Panel (RUSP) Classification 2,4 Dienoyl CoA Reductase Deficiency DE RED Fatty Acid Oxidation Disorder Secondary Condition 2-Methyl 3 Hydroxy Butyric Aciduria 2M3HBA Organic Acid Disorder Secondary Condition 2-Methyl Butyryl-CoA Dehydrogenase Deficiency 2MBG Organic Acid Disorder Secondary Condition (called 2-Methylbutyrylglycinuria on RUSP) 3-Hydroxy-3-Methylglutaryl CoA Lyase Deficiency HMG Organic Acid Disorder Core Condition 3-Methylcrotonyl CoA Carboxylase Deficiency 3MCC Organic Acid Disorder Core Condition 3-Methylglutaconic Aciduria 3MGA Organic Acid Disorder Secondary Condition Alpha-Thalassemia (Bart's Hb) Hemoglobin Bart's Hemoglobin Disorder Secondary Conditoin Argininemia, Arginase Deficiency ARG Amino Acid Disorder Secondary Condition Arginosuccinic Aciduria ASA Amino Acid Disorder Core Condition Benign Hyperphenylalaninemia PHE Amino Acid Disorder Secondary Condition Beta-Ketothiolase Deficiency BKT Organic Acid Disorder Core Condition Biopterin Defect in Cofactor Biosynthesis BIOPT (BS) Amino Acid Disorder Secondary Condition Biopterin Defect in Cofactor Regeneration BIOPT (Reg) Amino Acid Disorder Secondary Condition Biotinidase Deficiency BIO Metabolic Disorder of Biotin Recycling Core Condition Carbamoyltransferase Deficiency, Carbamoyl Phosphate Synthetase I Deficiency CPS Amino Acid Disorder Not on RUSP Carnitine Palmitoyl Transferase Deficiency Type 1 CPT I Fatty Acid Oxidation Disorder Secondary Condition -

Inborn Errors of Metabolism Collaborative: Large-Scale Collection of Data on Long-Term Follow-Up for Newborn-Screened Conditions
ORIGINAL RESEARCH ARTICLE © American College of Medical Genetics and Genomics Inborn Errors of Metabolism Collaborative: large-scale collection of data on long-term follow-up for newborn-screened conditions Susan A. Berry, MD1, Nancy D. Leslie, MD2, Mathew J. Edick, PhD3, Sally Hiner3, Kaitlin Justice3 and Cynthia Cameron, PhD3; for the Inborn Errors of Metabolism Collaborative Purpose: The Inborn Errors of Metabolism Information System on the recommended uniform screening panel; 4 conditions have (IBEM-IS) collects data on the clinical history of inborn errors of more than 100 subjects enrolled. Median follow-up time for subjects metabolism (IBEMs). The IBEM-IS is accessible to metabolic clinics with more than one visit (n = 898) is 1.5 years (interquartile range = nationwide and seeks to (i) influence clinical management of affected 2.2 years). Subjects with critical conditions are more likely to have individuals and (ii) provide information to support public health emergency letters and sick-day plans. Mortality was exclusive to chil- decision making. dren with critical conditions. Methods: Thirty centers in 21 states are enrolling persons with Conclusion: Large-scale prospective data can be collected for indi- newborn-screened conditions, collecting information on diagnosis viduals with rare conditions, permitting enhanced decision making and treatment at the time of enrollment and all subsequent visits. for clinical management and supporting decision making in public Prospective data are collected using electronic capture forms allow- health newborn screening programs. ing aggregation of information regarding outcomes for individuals affected with IBEMs. Genet Med advance online publication 19 May 2016 Results: A total of 1,893 subjects have been enrolled in the IBEM-IS, Key Words: inborn errors of metabolism; natural history; newborn and more than 540,000 individual data points have been collected. -

Movement Disorders and Neurometabolic Diseases
Movement Disorders and Neurometabolic Diseases. Celanie K. Christensen, MS MD1, 2, Laurence Walsh, MD1, 2, 3 1Department of Neurology, Section of Child Neurology, Indiana University School of Medicine, Indianapolis, IN 2Department of Pediatrics, Section of Developmental Pediatrics, Indiana University School of Medicine, Indianapolis, IN 3Department of Medical and Molecular Genetics, Indiana University School of Medicine, Indianapolis, IN From: Riley Hospital for Children at Indiana University Health and Indiana University School of Medicine Address reprint requests to: Celanie K. Christensen, MS MD Section of Developmental Pediatrics RI1601 705 Riley Hospital Drive Indianapolis, IN 46202 ___________________________________________________________________ This is the author's manuscript of the article published in final edited form as: Christensen, C. K., & Walsh, L. (2018). Movement Disorders and Neurometabolic Diseases. Seminars in Pediatric Neurology. https://doi.org/10.1016/j.spen.2018.02.003 Abstract Many inherited metabolic disorders cause movement disorders in children. This review focuses on chorea, dystonia, myoclonus, tremor, and parkinsonism. Broad categories commonly responsible for pediatric movement disorders include mitochondrial disorders, organic acidemias, mineral metabolism and transport disorders, neurotransmitter diseases, purine metabolism disorders, lipid storage disorders, and disorders of creatine metabolism. Each movement disorder can be caused by many different inherited metabolic disorders and several of the inherited metabolic disorders can cause multiple movement abnormalities. Dietary modifications, medications, and increasingly specific therapy can improve outcomes in children with movement disorders caused by metabolic disorders. Recognition and characterization of secondary movement disorders in children facilitate management of the abnormal movements and diagnosis, and possible treatment, of an underlying metabolic disorder. Introduction Many inborn errors of metabolism (IEM) cause movement disorders in children.