Hello My Name Is and I Have Parkinson's Disease
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Parkinson's Disease Fact Sheet
Parkinson’s Disease Fact Sheet About Parkinson’s Disease Parkinson’s disease is a progressive, incurable neurological disorder associated with a loss of dopamine-generating cells in the brain. It is primarily associated with progressive loss of motor control, but it results in a complex array of symptoms, including many non-motor symptoms. Parkinson’s impacts an estimated one million people in the United States. Critical Clinical Care Considerations • To avoid serious side effects, Parkinson’s patients need their medications on time, every time — do not skip or postpone doses. • Write down the exact times of day medications are to be administered so that doses are given on the same schedule the patient follows at home. • Do not substitute Parkinson’s medications or stop levodopa therapy abruptly. • Resume medications immediately following procedures, unless vomiting or severely incapacitated. • If an antipsychotic is necessary, use pimavanserin (Nuplazid), quetiapine (Seroquel) or clozapine (Clozaril). • Be alert for symptoms of dysphagia (trouble swallowing) and risk of pneumonia. • Ambulate as soon as medically safe. Patients may require assistance. Common Symptoms of Parkinson’s Disease Motor Non-Motor • Shaking or tremor at rest • Depression • Bradykinesia or freezing (being stuck • Anxiety in place when attempting to walk) • Constipation • Low voice volume or muffled speech • Cognitive decline and dementia • Lack of facial expression • Impulse control disorders • Stiffness or rigidity of the arms, legs • Orthostatic hypotension or -

Together with CCHP's Medication List Prior Authorization Is Required If Indicated by X(PA)
Together with CCHP's Medication List Prior authorization is required if indicated by X(PA). Pharmacy Benefit: Submit authorizations through Together with CCHP's Pharmacy Services. Medical Benefit: Submit authorizations through CareWeb Qi Authorization tool. Jcode Brand Name Description Pharmacy Medical Notes J3365 Abbokinase INJECTION, UROKINASE, 250,000 IU X J0287 Abelcet INJECTION, AMPHOTERICIN B LIPID X COMPLEX, 10 MG J0401 Abilify Maintena INJECTION, ARIPIPRAZOLE, EXTENDED X X May bIll eIther RELEASE, 1 MG (PA < 12 YEARS OF benefIt, PA AGE) reQuIred when bIllIng through pharmacy INJECTION, PACLITAXEL PROTEIN- J9264 Abraxane BOUND PARTICLES, 1 MG X J7613 Accuneb ALBUTEROL, INHALATION SOLUTION, X FDA- APPROVED FINAL PRODUCT, NONCOMPOUNDED, ADMINISTERED THROUGH DME, UNIT DOSE, 1 MG J0132 Acetadote INJECTION, ACETYLCYSTEINE, 100 MG X J7608 Acetylcysteine ACETYLCYSTEINE, INHALATION X SOLUTION, FDA- APPROVED FINAL PRODUCT, NONCOMPOUNDED, ADMINISTERED THROUGH DME, UNIT DOSE FORM, PER G J3262 Actemra INJECTION, TOCILIZUMAB, 1 MG X (PA) J0800 Acthar Gel INJECTION, CORTICOTROPIN, UP TO 40 X (PA) UNITS J0795 Acthrel INJECTION, CORTICORELIN OVINE X TRIFLUTATE, 1 MCG J9216 Actimmune INTERFERON GAMMAM 1-B X (PA) J2997 Activase INJECTION, ALTEPLASE RECOMBINANT, X 1 MG J2504 Adagen PEGADEMASE BOVINE 25 IU X (PA) J2062 Adasuve LoxapIne, InhalatIon powder, 10 mg X INJECTION, BRENTUXIMAB VEDOTIN, 1 J9042 Adcetris X MG 1 Together with CCHP's Medication List Prior authorization is required if indicated by X(PA). Pharmacy Benefit: Submit authorizations -

Neuroleptic Malignant Syndrome in the Acquired Immunodeficiency Syndrome
Postgrad Med J 1997; 73: 779-784 (© The Fellowship of Postgraduate Medicine, 1997 HIV medicine Postgrad Med J: first published as 10.1136/pgmj.73.866.779 on 1 December 1997. Downloaded from Neuroleptic malignant syndrome in the acquired immunodeficiency syndrome Jose L Hemaindez, Luis Palacios-Araus, Santiago Echevarria, Andres Herran, Juan F Campo, Jose A Riancho Summary The neuroleptic malignant syndrome (NMS) is a life-threatening process, Patients infected by the human typically, but not exclusively, induced by drugs of the neuroleptic group. Its immunodeficiency virus are pre- main clinical manifestations include fever, rigidity of skeletal muscles, disposed to many infectious and fluctuating consciousness and autonomic disturbances.' Since first described noninfectious complications and by Delay and Deniker in 1968,2 the syndrome has received increasing attention often receive a variety of drugs. and more than 1600 cases have been reported to date, including a few cases in Furthermore, they seem to have a patients with the acquired immunodeficiency syndrome (AIDS).3-8 Never- particular susceptibility to idio- theless, outside psychiatry, the syndrome probably remains underdiagnosed, as syncratic adverse drug reactions. its manifestations may be also caused by other processes such as infections and It is therefore surprising that only neoplasms. Thus, a high index of suspicion is needed to not miss the diagnosis a few cases of the neuroleptic in medical patients. This is particularly important in patients infected by the malignant syndrome have been human immunodeficiency virus (HIV), who commonly suffer infectious described in patients with the complications but also often receive psychoactive drugs. This article reviews acquired immunodeficiency syn- the main features of NMS in AIDS patients. -

One Step Multi-Drug Screen Test Cup Package Insert
Fentanyl (FEN) Fentanyl 300 the treatment of seizure disorders and alcohol withdrawal. Risk of physical dependence increases if One Step Multi-Drug Screen Test Cup Benzodiazepines are taken regularly (e.g., daily) for more than a few months, especially at higher Fentanyl (FEN) Fentanyl 200 than normal doses. Stopping abruptly can bring on such symptoms as trouble sleeping, Package Insert Fentanyl (FEN) Fentanyl 100 gastrointestinal upset, feeling unwell, loss of appetite, sweating, trembling, weakness, anxiety and changes in perception. Only trace amounts (less than 1%) of most Benzodiazepines are excreted Cotinine (COT) Cotinine 200 Package insert for testing of any combination of the following drugs: Methamphetamine, unaltered in the urine; most of the concentration in urine is conjugated drug. The detection period Amphetamine, Cocaine, Morphine, Ecstasy, EDDP (Methadone Metabolites), Tricyclic 6-Monoacetylmorphine (6-MAM) 6-Monoacetylmorphine 10 for the Benzodiazepines in the urine is 3-7 days. Antidepressants, Oxycodone, Barbiturates, Buprenorphine, Phencyclidine, K2 (Synthetic Methaqualone (MQL) Methaqualone 300 Cannabinoid), Ketamine, Methaqualone, Methadone, Fentanyl, Tramadol, Ethyl Glucuronide, OXYCODONE (OXY) Cotinine, 6-Monoacetylmorphine, Methylenedioxypyrovalerone, Lysergic acid diethylamide, Ketamine (KET) Ketamine 1,000 Oxycodone, [4,5-epoxy-14-hydroxy-3-methoxy-17-methyl-morphinan-6-one, Marijuana and Benzodiazepines. Ketamine (KET) Ketamine 100 dihydrohydroxycodeinone] is a semi-synthetic opioid agonist derived from thebaine, -

The Action of Thiethylperazihe Torecan®), a New Anti-Emetic, Compared
TH,'E ACTION OFf THIETHYLPERAZI!~Ei: ~ITO!~ECANr A NE'~( ANTI''-- EMETIC, COMPARED,' WITH:". PER[P:NHE' i ' q[AZINE ' ( TRILAFON|:'1 L TR~METHOBENZAMIDE (TIGAN| AND[A PI.ACE~O IN THE" suPPRESSION OF POSTANAESTHETI~NAIUSEN AND V()MITING IAN E. PtrnICIS, M.B., B.S., ~.F.A..I~.C.S.O POSTa_Na_ESTH~TIC VOMITING has been ~shown ~0 b(l" i~ffffeneed ]~y a varie]ty of factors, and it is therefore unlikely that any a~i-ergetie drug will be completely effective and without side-effects in all patients. In[the absence of any ele~r-eut superiority of one drug over another,-the physi4ian naust exercise a choicK selecting a drug with minimum side-effects but maximum anti-emetic effect. This choice can only be made on the basis of ieontrolled studies of effectir and side-effects, since clinical impressions can be nlost misleading.~ Malay ~igents can be shown to have an anti-emetic effect wl~n e0mpared I with a placebo (e.g., atropine) 1 but they may not be clinically us,~fuI as anfi-erneties. If new drug can be shown to have an effect equal to ~or better than a drug whi, .a has proven highly effective against a strong clinica,l challenge, then it is likeb that the new agent will be clinically useful. Thiethylperazine (Toreean| is a phenothiazin Which possesses to a very marked degree the anti-emetic activity common to all drugs, of this group, while the other group activities of lowering bk od pressure,~=.potentiatign of narcotics and barbil~urates, and extrapyramidal et feets, are minimized. -
Procedure Codes, Section 3
NEW YORK STATE MEDICAID PROGRAM PHYSICIAN – PROCEDURE CODES SECTION 3 - DRUGS and DRUG ADMINISTRATION Physician – Procedure Codes , Section 3- Drugs and Drug Administration _____________________________________________________________________________ Table of Contents GENERAL RULES AND INFORMATION ............................................................2 MMIS DRUG MODIFIERS ....................................................................................4 DRUGS.................................................................................................................5 IMMUNE GLOBULINS...................................................................................................5 VACCINES, TOXOIDS ..................................................................................................5 HYDRATION, THERAPEUTIC, PROPHYLACTIC AND DIAGNOSTIC INJECTIONS AND INFUSIONS (EXCLUDES CHEMOTHERAPY) .....................................................8 DRUGS ADMINISTERED OTHER THAN ORAL METHOD.........................................10 CHEMOTHERAPY ADMINISTRATION.......................................................................19 CHEMOTHERAPY DRUGS.........................................................................................21 Version 2008 – 1 (5/15/2008) Page 1 of 23 Physician – Procedure Codes , Section 3- Drugs and Drug Administration _____________________________________________________________________________ GENERAL RULES AND INFORMATION 1. BY REPORT: A service that is rarely provided, unusual, variable, -

High-Risk Medications in the Elderly
High-Risk Medications in the Elderly The Centers for Medicare & Medicaid Services (CMS) contracted with the National Committee for Quality Assurance (NCQA) to develop clinical strategies to monitor and evaluate the quality of care provided to Medicare beneficiaries. The NCQA’s Geriatric Measurement Advisory Panel identified several categories of medications that have an increased risk of adverse effects to elderly patients. The enclosed chart identifies several key medication categories that CMS and NCQA are monitoring. In an effort to ensure patients’ safety, many of our clients have established pre-authorization protocols for those prescriptions for high risk medications in patients older than 65 years of age. Since pharmacists have a very important role in patient care, we want you to be part of this safety initiative. We strongly encourage that you contact the prescriber when your elderly patient is requesting a new or refilled prescription of a high-risk medication listed on the below chart. Category High Risk Medications Alternatives Analgesics butalbital/APAP Mild Pain: butalbital/APAP/caffeine (ESGIC, FIORICET) acetaminophen, codeine, short-term NSAIDs butalbital /APAP/caffeine/codeine Moderate/Severe Pain: butalbital/ASA/caffeine (FIORINAL) tramadol (ULTRAM), tramadol/APAP* (ULTRACET), butalbital/ASA/caffeine/codeine morphine sulfate (MS CONTIN), ketorolac (TORADOL) hydrocodone/APAP (VICODIN, etc.), oxycodone indomethacin (INDOCIN) (OXYIR), oxycodone/APAP (PERCOCET), fentanyl meperidina (DEMEROL) patch (DURAGESIC), OXYCONTIN -
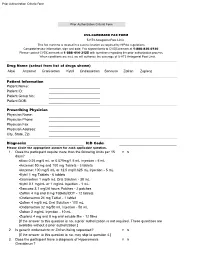
Prior Authorization Criteria Form
Prior Authorization Criteria Form Prior Authorization Criteria Form CVS-CAREMARK FAX FORM 5-HT3 Antagonist Post Limit This fax machine is located in a secure location as required by HIPAA regulations. Complete/review information, sign and date. Fax signed forms to CVS|Caremark at 1-888-836-0730. Please contact CVS|Caremark at 1-888-414-3125 with questions regarding the prior authorization process. When conditions are met, we will authorize the coverage of 5-HT3 Antagonist Post Limit. Drug Name (select from list of drugs shown) Aloxi Anzemet Granisetron Kytril Ondansetron Sancuso Zofran Zuplenz Patient Information Patient Name: Patient ID: Patient Group No.: Patient DOB: Prescribing Physician Physician Name: Physician Phone: Physician Fax: Physician Address: City, State, Zip: Diagnosis: ICD Code: Please circle the appropriate answer for each applicable question. 1. Does the participant require more than the following limits per 15 Y N days? ▪Aloxi 0.25 mg/5 mL or 0.075mg/1.5 mL Injection - 5 mL ▪Anzemet 50 mg and 100 mg Tablets - 3 tablets ▪Anzemet 100 mg/5 mL or 12.5 mg/0.625 mL Injection - 5 mL ▪Kytril 1 mg Tablets - 6 tablets ▪Granisetron 1 mg/5 mL Oral Solution - 30 mL ▪Kytril 0.1 mg/mL or 1 mg/mL Injection - 1 mL ▪Sancuso 3.1 mg/24 hours Patches - 2 patches ▪Zofran 4 mg and 8 mg Tablets/ODT - 12 tablets ▪Ondansetron 24 mg Tablet - 1 tablet ▪Zofran 4 mg/5 mL Oral Solution - 100 mL ▪Ondansetron 32 mg/50 mL Injection - 50 mL ▪Zofran 2 mg/mL Injection - 10 mL ▪Zuplenz 4 mg and 8 mg oral soluble film - 12 films [If the answer to this question is no, a prior authorization is not required. -

Table III 2021 Medicare National Drug Fee Schedule
Table III: 2021 Medicare Drug Fee Schedule* CY 2021 3rd Quarter Average Sales Price (ASP) Data Plus 6 Percent *The Medicare payments allowance limits are effective July 1 - September 30, 2021 CY 2021 CY 2021 CY 2021 Effective Jan. 1 Effective Apr. 1 Effective July 1 Through Mar. 31 Through June 30 Through Sep. 30 Code Description Code Dosage ASP plus 6 percent ASP plus 6 percent ASP plus 6 percent J0129 Abatacept 10mg $56.87 $57.83 $45.32 J0133 Acyclovir, 5 mg 5mg $0.04 $0.03 $0.04 J0171 Adrenalin epinephrin inject 0.1mg $0.85 $0.84 $0.80 J0207 Amifostine 500mg $1,135.69 $1,135.69 $1,135.69 J0256 Alpha 1 proteinase inhibitor 10mg $4.52 $4.51 $4.56 J0280 Aminophyllin 250 MG inj 250mg $10.34 $9.50 $6.11 J0289 Amphotericin b liposome inj 10mg $27.24 $27.07 $28.33 J0295 Ampicillin sodium per 1.5 gm 1.5gm $2.46 $2.75 $2.79 J0360 Hydralazine hcl injection 20mg $2.94 $4.87 $5.69 J0456 Azithromycin 500mg $3.30 $4.58 $3.88 J0461 Atropine sulfate injection 0.01mg $0.08 $0.09 $0.10 J0475 Baclofen 10 MG injection 10mg $172.78 $179.01 $179.42 J0476 Baclofen intrathecal trial 50mcg $56.66 $57.06 $58.45 J0480 Basiliximab 20mg $4,019.07 $4,016.20 $4,029.23 J0490 Belimumab 10mg $46.84 $46.87 $47.58 J0500 Dicyclomine injection 20mg $34.64 $33.85 $29.12 J0515 Inj benztropine mesylate 1mg $17.16 $17.41 $17.33 J0570 Buprenorphine implant 74.2mg $1,204.99 $1,285.78 $1,311.75 J0583 Bivalirudin 1mg $0.45 $0.60 $0.34 J0585 Botulinum toxin a per unit 1unit $6.06 $6.06 $6.08 J0587 Botulinum toxin type B 100units $11.97 $11.97 $11.57 J0592 Buprenorphine hydrochloride -

Virginia's Department of Medical Assistance Services Pharmacy and Therapeutics Committee Meeting
Virginia’s Department of Medical Assistance Services Pharmacy and Therapeutics Committee Meeting Thursday, September 17, 2020 - 10:00 a.m. Please click on this link to join the WebEx Audio Access: 866-692-4530; Pin 161 535 7780 This is an electronic public meeting held pursuant to Items 4-0.01(g) in House Bill 29 and House Bill 30. The FOIA Councils “Electronic Meetings Public Comment” form for submitting feedback on this electronic meeting may be accessed at http://foiacouncil.dls.virginia.gov/sample%20letters/welcome.htm Welcome and Comments from DMAS’ Director Karen Kimsey Virginia’s Secretary of Health & Human Resources Daniel Carey, MD, MHCM Call to Order Chethan Bachireddy, MD, CMO, Chair Approval of Minutes from April 20, 2020 Meeting P&T Committee Members Drug Utilization Review (DUR) Board Update Rachel Cain, PharmD PDL Management P&T Committee Members PDL Phase II – New Drug Review (Therapeutic Class) Brand Drugs Arazlo® (Acne Agents, Topical) AvsolaTM (Cytokine & Cam Antagonists) (Closed class) Licart Patch (topical NSAIDS) LyumjevTM (Hypoglycemics, Insulin & Related Agents) Nurtec® ODT (Antimigraine Agents, Other) Trijardy® XR (Hypoglycemics, SGLT2) (Closed class) Zeposia® (Multiple Sclerosis Agents) ZilxiTM Foam (Rosacea Agents, Topical) Generics Drugs and New Dosage Forms (additional information on P&T Committee web site) Antipsoriatic, Topical TCR calcipotriene 0.005% foam & calcipotriene/betamethasone suspension new generic for Sorilux and Taclonex susp Hypoglycemics, Metformin new generic for Riomet Solution NSAIDS TCR: -

Trimeprazine Tartrate (Panectyl| Diphenhy- Dramine Hce (Benadryl| Dimenhydrinate (Gravol| Dramam I Ne| and Cyiclizine Lactate (Marzine| Marazi Ne|
THE ANTISIALOGOGUE EFFECT OF TRIMETHOBENZAMIDE HCL (TIGAN| TRIMEPRAZINE TARTRATE (PANECTYL| DIPHENHY- DRAMINE HCE (BENADRYL| DIMENHYDRINATE (GRAVOL| DRAMAM I NE| AND CYICLIZINE LACTATE (MARZINE| MARAZI NE| ALLEN B. DOBKINI~ and V. GuY CRISWICK~ IT IS DIFFICULT tO tell clinically whether an ancillary drug, which is useful in association with anaesthesia, has useful physiological eh%cts other tha.n those of its primary action unless they are studied specifically. The a ntisialogogue effects of the following drags which are used primarily ~as antihistaminics and anti-emetics are reported here. Trimethobenzctmide HCL (Tigan| is la substituted benzamide which con- tains the active substance 4-(2-dimetliylaminoethoxy)-N-(3,4,5-trimethoxy. benzoyl)-benzylamine HCL.-It is a White, odourless, crystalline powder which is water soluble (more than 50 per cent at 25 ~ C), and has a bitter taste. It has been used primarily as an anti-emetic, t Its anti-emetic effect appears to act at the chemoreceptor trigger zone, as with the phenothiazine derivatives, although its chemical structure resembles the dimethyl aminoethoxy antihistamines, such as diphenhydramine. It is not as effective in preventing vomiting caused by strong reflex visceral impulses. It does not cause,any hypnotic sedation or behavioural depression as is observed with chlorpromazine. Tigan does ~lot have the anti- histaminic or antiadrenaline effects of the phenothiazines or structuralb: related compounds. 2 Trimeprazine tartrate (Panectyl| is a iphenothiazine derivative whose anti. histaminic and anti-emetic properties exceed those of promethazine. It has only a weak antiadrenaline effect, but its spasmolytic effect exceeds that of chlorpro- mazine. The hypnotic sedative action is of the same order as promdthazine. -

Cardiovascular Effects of Trimethobenzamide
C'.ARDIOVASCULAR. BlFICTS OF TlllMITHOBBNZAMIDI by DON NOLAN BENSLAY A TBISIS submitted to ORIGON STATI COLLIGB in partial fulfillment of the re~uirementa for the degree of MASTEl. Ol SCIENCE June 1961 AltlilDr Redacted for Privacy & 0hrrfr r! il.rcr Redacted for Privacy Redacted for Privacy Redacted for Privacy hGr tlrrt L ptrratrl .M/ r-/Z9o - tn a Dy Ydlr D. mrllln ACltNOWLEDGMDT The author wishes to expre•e hie sincere thanks and gratitude to Dr. Rob s. McCutcheon for his efforts in securing the generous gz.-ant from Hoffmann•La Roche Laboratories, which made thia work pottible, and for his help throughout the couz.-se of the ttudy and writing of this paper. Thankt is also due Boffmann•La Roche for their generoua eon• tributions and other pharmaceutical companies; named 1n the text, for theiz.- donations of drugs used 1n this study. Special thanks and appreciation is felt for the help, encour ag•ent and patience given by my wife, Mary Lea, and her mother, Velda D. Mullina, duri113 the paat year. TAILI or COHTIMTS IITI.ODUCTIOM • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • . • • • • • • • • • • • • • • . • • • • 1 IUilliMD'lAL MITBODS ............... ' ........................... 8 BI.OOD russuu STUDDS. • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • a CAIDU.C STUDIES ........................................... 10 liSULTS AND DISCUSSION ......................................... 17 BLOOD PIKSSURI STUDY liSOLTS ••••••••••••••••••••••••••••••• 17 BLOOD PIISSUU STUDY DISCUSSION •••••••••••••••••••••••••••