Antipsoriatic Agents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Left/Right Comparison of Twice-Daily Calcipotriol Ointment and Calcitriol Ointment in Patients with Psoriasis: the Effect on Keratinocyte Subpopulations
Acta Derm Venereol 2004; 84: 195–200 INVESTIGATIVE REPORT A Left/Right Comparison of Twice-Daily Calcipotriol Ointment and Calcitriol Ointment in Patients with Psoriasis: The Effect on Keratinocyte Subpopulations Mannon E.J. FRANSSEN, Gys J. DE JONGH, Piet E.J. VAN ERP and Peter C.M. VAN DE KERKHOF Department of Dermatology, University Medical Centre Nijmegen, The Netherlands Vitamin D3 analogues are a first-line treatment of Calcipotriol (Daivonex1,50mg/g ointment, Leo chronic plaque psoriasis, but so far, comparative clinical Pharmaceutical Products, Denmark) has been investi- studies on calcipotriol and calcitriol ointment are sparse, gated intensively during the last decade, and has proven and in particular no comparative studies are available on to be a valuable tool in the management of chronic cell biological effects of these compounds in vivo. Using plaque psoriasis. A review by Ashcroft et al. (1), based on flow cytometric assessment, we investigated whether these a large number of randomized controlled trials, showed compounds had different effects on the composition and that calcipotriol was at least as effective as potent DNA synthesis of epidermal cell populations responsible topical corticosteroids, 1a,-25-dihydroxycholecalciferol for the psoriatic phenotype. For 8 weeks, 20 patients with (calcitriol), short-contact dithranol, tacalcitol and coal psoriasis vulgaris were treated twice daily with calcipo- tar. Recently, Scott et al. (2) presented an overview of triol and calcitriol ointment in a left/right comparative studies on the use of calcipotriol ointment in the study. Before and after treatment, clinical assessment of management of psoriasis. They reconfirmed the super- target lesions was performed, together with flow cyto- ior efficacy of a twice-daily calcipotriol ointment metric analysis of epidermal subpopulations with respect regimen to the treatments as mentioned above, and to keratin (K) 10, K6, vimentin and DNA distribution. -

Reseptregisteret 2013–2017 the Norwegian Prescription Database
LEGEMIDDELSTATISTIKK 2018:2 Reseptregisteret 2013–2017 Tema: Legemidler og eldre The Norwegian Prescription Database 2013–2017 Topic: Drug use in the elderly Reseptregisteret 2013–2017 Tema: Legemidler og eldre The Norwegian Prescription Database 2013–2017 Topic: Drug use in the elderly Christian Berg Hege Salvesen Blix Olaug Fenne Kari Furu Vidar Hjellvik Kari Jansdotter Husabø Irene Litleskare Marit Rønning Solveig Sakshaug Randi Selmer Anne-Johanne Søgaard Sissel Torheim Utgitt av Folkehelseinstituttet/Published by Norwegian Institute of Public Health Område for Helsedata og digitalisering Avdeling for Legemiddelstatistikk Juni 2018 Tittel/Title: Legemiddelstatistikk 2018:2 Reseptregisteret 2013–2017 / The Norwegian Prescription Database 2013–2017 Forfattere/Authors: Christian Berg, redaktør/editor Hege Salvesen Blix Olaug Fenne Kari Furu Vidar Hjellvik Kari Jansdotter Husabø Irene Litleskare Marit Rønning Solveig Sakshaug Randi Selmer Anne-Johanne Søgaard Sissel Torheim Acknowledgement: Julie D. W. Johansen (English text) Bestilling/Order: Rapporten kan lastes ned som pdf på Folkehelseinstituttets nettsider: www.fhi.no The report can be downloaded from www.fhi.no Grafisk design omslag: Fete Typer Ombrekking: Houston911 Kontaktinformasjon/Contact information: Folkehelseinstituttet/Norwegian Institute of Public Health Postboks 222 Skøyen N-0213 Oslo Tel: +47 21 07 70 00 ISSN: 1890-9647 ISBN: 978-82-8082-926-9 Sitering/Citation: Berg, C (red), Reseptregisteret 2013–2017 [The Norwegian Prescription Database 2013–2017] Legemiddelstatistikk 2018:2, Oslo, Norge: Folkehelseinstituttet, 2018. Tidligere utgaver / Previous editions: 2008: Reseptregisteret 2004–2007 / The Norwegian Prescription Database 2004–2007 2009: Legemiddelstatistikk 2009:2: Reseptregisteret 2004–2008 / The Norwegian Prescription Database 2004–2008 2010: Legemiddelstatistikk 2010:2: Reseptregisteret 2005–2009. Tema: Vanedannende legemidler / The Norwegian Prescription Database 2005–2009. -

Topically Used Herbal Products for the Treatment of Psoriasis – Mechanism of Action, Drug Delivery, Clinical Studies
Reviews 1447 Topically Used Herbal Products for the Treatment of Psoriasis – Mechanism of Action, Drug Delivery, Clinical Studies Authors Anna Herman1, Andrzej P. Herman 2 Affiliations 1 Faculty of Cosmetology, The Academy of Cosmetics and Health Care, Warsaw, Poland 2 Laboratory of Molecular Biology, The Kielanowski Institute of Animal Physiology and Nutrition, Polish Academy of Sciences, Jabłonna, Poland Key words Abstract several electronic databases and literature refer- l" Psoriasis ! ences were used to summarize the current l" herbal products Psoriasis is a chronic inflammatory skin disease knowledge acquired on the basis of animal stud- l" keratinocyte hyper- characterized histologically by hyperproliferation ies and clinical trials regarding herbal products proliferation and aberrant differentiation of epidermal kerati- used to treat psoriasis topically. This review dis- l" inflammatory reaction l" skin barrier nocytes. A wide range of conventional medical cusses the mechanisms of herbal products activ- l" herbal drug delivery systems therapies to treat psoriasis is established, from ities through (1) inhibition of the keratinocyte hy- topical therapies and systemic medications perproliferation and inducing apoptosis, (2) inhi- through to phototherapy or combinations of bition of immune-inflammatory reaction, (3) those. However, most of these therapies have a suppression of phosphorylase kinase (PhK) activ- limited efficacy and may cause a number of side ity, and (4) inhibition of the hedgehog (Hh) sig- effects, including cutaneous atrophy, organ toxic- naling pathway. Moreover, the penetration of ity, carcinogenicity, and broadband immunosup- herbal products through the psoriatic skin barrier, pression, which are restricting their long-term novel herbal drug delivery systems in psoriasis use. Therefore, it would be desirable to use herbal treatment, and possible adverse effects of herbal products as an alternative treatment for psoriasis therapy are discussed. -

Nurse-Led Drug Monitoring Clinic Protocol for the Use of Systemic Therapies in Dermatology for Patients
Group arrangements: Salford Royal NHS Foundation Trust (SRFT) Pennine Acute Hospitals NHS Trust (PAT) Nurse-led drug monitoring clinic protocol for the use of systemic therapies in dermatology for patients with inflammatory dermatoses Lead Author: Dawn Lavery Dermatology Advanced Nurse Practitioner Additional author(s) N/A Division/ Department:: Dermatology, Clinical Support and Tertiary Medicine Applies to: (Please delete) Salford Royal Care Organisation Approving Committee Dermatology clinical governance committee Salford Royal Date approved: 13 February 2019 Expiry date: February 2022 Contents Contents Section Page Document summary sheet 1 Overview 2 2 Scope & Associated Documents 2 3 Background 3 4 What is new in this version? 3 5 Policy 4 Drugs monitored by nurses 4 Acitretin 7 Alitretinoin Toctino 11 Apremilast 22 Azathioprine 26 Ciclosporin 29 Dapsone 34 Fumaric Acid Esters – Fumaderm and Skilarence 36 Hydroxycarbamide 39 Hydroxychloroquine 43 Methotrexate 50 Mycophenolate moefetil 57 Nurse-led drug monitoring clinic protocol for the use of systemic therapies in dermatology for patients with inflammatory dermatoses Reference Number GSCDerm01(13) Version 3 Issue Date: 11/06/2019 Page 1 of 77 It is your responsibility to check on the intranet that this printed copy is the latest version Standards 67 6 Roles and responsibilities 67 7 Monitoring document effectiveness 67 8 Abbreviations and definitions 68 9 References 68 10 Appendices N/A 11 Document Control Information 71 12 Equality Impact Assessment (EqIA) screening tool 73 Group arrangements: Salford Royal NHS Foundation Trust (SRFT) Pennine Acute Hospitals NHS Trust (PAT) 1. Overview (What is this policy about?) The dermatology directorate specialist nurses are responsible for ensuring prescribing and monitoring for patients under their care, is in accordance with this protocol. -
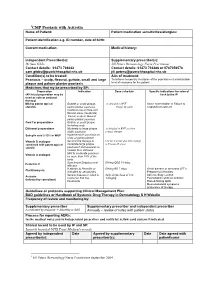
CMP 2 Psoriasis with Acitretin/Methotrexate
1CMP Psoriasis with Acitretin Name of Patient: Patient medication sensitivities/allergies: Patient identification e.g. ID number, date of birth: Current medication: Medical history: Independent Prescriber(s): Supplementary prescriber(s): Dr Sam Gibbs Jill Peters Dermatology Nurse Practitioner Contact details: 01473 704042 Contact details: 01473 704386 or 0787056578 [email protected] [email protected] Condition(s) to be treated: Aim of treatment: Psoriasis – scalp, flexural, guttate, small and large To achieve temporary clearance of the psoriasis or a maintainable plaque and palmer planter psoriasis level of clearance for the patient Medicines that my be prescribed by SP: Preparation Indication Dose schedule Specific indications for referral (All listed preparation may be back to the IP used as sole or conjunct therapy) Mild to potent topical Guttate or small plaque, As detailed in BNF Acute exacerbation or Failure to steroids palmo plantar psoriasis. Finger tip units respond to treatment Cautious use on face and flexural areas (moderate) Facial, scalp or flexural, palmo plantar psoriasis Coal Tar preparations Guttate or small plaque including scalp Dithranol preparations Moderate to large plaque As detailed in BNF as short stable psoriasis contact therapy Salicylic acid 2-10% in WSP Hyperkeratotic psoriasis on scalp or palmo plantar Vitamin D analogue Second line therapy to Use for 4 weeks and then change combined with potent topical moderate/large plaque to Vitamin D alone steroid psoriasis if unresponsive -
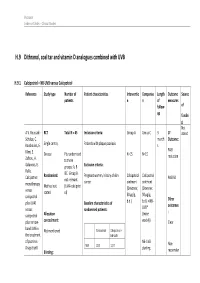
H.9 Dithranol, Coal Tar and Vitamin D Analogues Combined with UVB
Psoriasis Evidence Tables – Clinical Studies H.9 Dithranol, coal tar and vitamin D analogues combined with UVB H.9.1 Calcipotriol + NB-UVB versus Calcipotriol Reference Study type Number of Patient characteristics Interventio Compariso Length Outcome Source patients n n of measures follow- of up fundin g Not A.V. Roussaki- RCT Total N = 45 Inclusion criteria: Group A Group C 3 1º stated Schulze, C. month Outcome: Kouskoukis, E. Single centre, Patients with plaque psoriasis s Klimi, E. PASI Greece Pts randomised N=15 N=15 reduction Zafirou, A. to three Galanous, E. groups: A, B Exclusion criteria: Rallis. &C. Group B Calcipotriol Randomised: Pregnant women, history of skin Calcipotriol Calcipotriol PASI 50 not relevant cancer ointment ointment monotherapy Method not (UVA+calcipotri versus (Dovonex; (Dovonex stated ol) 50 µg/g, 50 µg/g, calcipotriol Other plus UVA1 Baseline characteristics of b.d.) b.d.) + NB- UVB* outcomes versus randomised patients: : calcipotriol Allocation (twice plus narrow- concealment: weekly) Clear band UVB in Calcipotriol Calcipotriol + Not mentioned the treatment NB-UVB of psoriasis. NB-UVB Non- Drugs Exptl. M/F 12/3 12/3 starting Blinding: responder Psoriasis Evidence Tables – Clinical Studies Cl in. Res , dose 80% 31(5/6):169- Not mentioned Age 44.93±6.48 49.53±22.01 MED and 174.2005 inc. by 20% Skin type 0/11/3/1 2/5/6/2 I/II/III/IV every 3 REFID: Washout sessions ROUSSAKISCH period: ULZE2005 90 days if using systemic *Cosmetico therapy, 30 days , 10 lamps if using topicals Helarium B1, 100 W each. -

Daivonex, Topical Ointment
NEW ZEALAND DATA SHEET 1 DAIVONEX® 50 microgram/gram topical ointment 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Daivonex® ointment contains calcipotriol 50 microgram per gram Daivonex® ointment contains the anhydrous form of calcipotriol. For full list of excipients, see section 6.1 List of excipients. 3 PHARMACEUTICAL FORM Daivonex® is a topical ointment. It is a smooth, white preservative free ointment base. 4 CLINICAL PARTICULARS 4.1 Indications Daivonex® ointment is indicated for the topical treatment of psoriasis vulgaris, including plaque psoriasis in adults and children (see section 4.4 Special warnings and precautions for use - paediatric population). In adult patients, Daivonex® ointment may also be used in combination with systemic acitretin or cyclosporin. 4.2 Dosage and method of administration Adults Daivonex® ointment therapy: Daivonex® ointment should be applied topically to the affected area once or twice daily (i.e. in the morning and/or in the evening). Initially, twice daily application of the ointment is usually preferred. Application may then be reduced to once daily, provided individual clinical response is satisfactory. After satisfactory improvement has occurred, treatment should be discontinued. If recurrence develops after reduction in frequency of application or after discontinuation, the treatment may be reinstituted at the initial dosage. Experience is lacking in the use of calcipotriol for periods longer than 1 year. The maximum recommended weekly dose of Daivonex® ointment is 100 g/week. When using a combination of ointment and cream the total maximum dose should not exceed 100 g per week. eDoc-000783454 - Version 1. 0 It should be noted that there are no long-term clinical studies assessing the safety of using Daivonex® ointment during exposure to sunlight. -

1 EMA Tender EMA/2017/09/PE, Lot 2 Impact of EU Label
EMA tender EMA/2017/09/PE, Lot 2 Impact of EU label changes and revised pregnancy prevention programme for oral retinoid containing medicinal products: risk awareness and adherence Protocol • Prof. Anna Birna Almarsdóttir, Professor in Social and Clinical Pharmacy at the Department of Pharmacy, Faculty of Health and Medical Sciences, University of Copenhagen • Prof. Marcel Bouvy, Professor of Pharmaceutical Care at the Division of Pharmacoepidemiology & Clinical Pharmacology of the Department of Pharmaceutical Sciences, Utrecht University. • Dr Rob Heerdink, Associate Professor at the Division of Pharmacoepidemiology & Clinical Pharmacology of the Department of Pharmaceutical Sciences, Utrecht University. • Dr Teresa Leonardo Alves, Researcher at the Centre for Health Protection, National Institute for Public Health and the Environment, The Netherlands. 1 Table of contents Background ...................................................................................................................... 3 Aims of the study ............................................................................................................. 4 Methods ........................................................................................................................... 4 Setting ........................................................................................... Error! Bookmark not defined. Study design ............................................................................................................................ 4 Population -

Acitretin; Adapalene; Alitretinoin; Bexarotene; Isotretinoin
8 February 2018 EMA/254364/2018 Pharmacovigilance Risk Assessment Committee (PRAC) Assessment report Referral under Article 31 of Directive 2001/83/EC resulting from pharmacovigilance data Retinoids containing medicinal products INN: Acitretin, Adapalene, Alitretinoin, Bexarotene, Isotretinoin, Tretinoin, Tazarotene Procedure number: EMEA/H/A-31/1446 Panretin EMEA/H/A-31/1446/C/000279/0037 Targretin EMEA/H/A-31/1446/C/000326/0043 Note: Assessment report as adopted by the PRAC and considered by the CHMP with all information of a commercially confidential nature deleted. 30 Churchill Place ● Canary Wharf ● London E14 5EU ● United Kingdom Telephone +44 (0)20 3660 6000 Facsimile +44 (0)20 3660 5555 Send a question via our website www.ema.europa.eu/contact An agency of the European Union © European Medicines Agency, 2018. Reproduction is authorised provided the source is acknowledged. Table of contents Table of contents ......................................................................................... 2 1. Information on the procedure ................................................................. 3 2. Scientific discussion ................................................................................ 3 2.1. Introduction......................................................................................................... 3 2.2. Clinical aspects .................................................................................................... 5 2.3. Data on efficacy .................................................................................................. -

Acitretin; Adapalene; Alitretinoin; Bexarotene; Isotretinoin
21 June 2018 EMA/261767/2018 Updated measures for pregnancy prevention during retinoid use Warning on possible risk of neuropsychiatric disorders also to be included for oral retinoids On 22 March 2018, the European Medicines Agency (EMA) completed its review of retinoid medicines, and confirmed that an update of measures for pregnancy prevention is needed. In addition, a warning on the possibility that neuropsychiatric disorders (such as depression, anxiety and mood changes) may occur will be included in the prescribing information for oral retinoids (those taken by mouth). Retinoids include the active substances acitretin, adapalene, alitretinoin, bexarotene, isotretinoin, tazarotene and tretinoin. They are taken by mouth or applied as creams or gels to treat several conditions mainly affecting the skin, including severe acne and psoriasis. Some retinoids are also used to treat certain forms of cancer. The review confirmed that oral retinoids can harm the unborn child and must not be used during pregnancy. In addition, the oral retinoids acitretin, alitretinoin and isotretinoin, which are used to treat conditions mainly affecting the skin, must be used in accordance with the conditions of a new pregnancy prevention programme by women able to have children. Topical retinoids (those applied to the skin) must also not be used during pregnancy, and by women planning to have a baby. More information is available below. Regarding the risk of neuropsychiatric disorders, the limitations of the available data did not allow to clearly establish whether this risk was due to the use of retinoids. However, considering that patients with severe skin conditions may be more vulnerable to neuropsychiatric disorders due to the nature of the disease, the prescribing information for oral retinoids will be updated to include a warning about this possible risk. -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -

Calcipotriol/Betamethasone Dipropionate: Daivobet®/Dovobet®
DRUG PROFILE Calcipotriol/betamethasone dipropionate: Daivobet®/Dovobet® Lyn C Guenther Psoriasis is a common skin condition that causes significant morbidity. Treatments can be 835 Richmond St., complex and time consuming. Calcipotriol plus betamethasone dipropionate ointment London, Ontario, (Daivobet® or Dovobet®) is a stable, convenient, once-daily topical treatment for psoriasis. N6A 3H7, Canada Tel.: +1 519 435 1738 Compared with its individual ingredients or tacalcitol, it has a faster speed of onset and Fax: +1 519 435 1740 greater efficacy. Consistent Psoriasis Area Severity Index reductions of approximately 40% [email protected] after 1 week and 70% after 4 weeks were seen in multicenter studies involving more than 6000 patients. After 4 weeks of once-daily therapy, approximately 50% of patients are clear or almost clear. This product is associated with a similar safety profile to betamethasone dipropionate ointment, 50% fewer cutaneous adverse events than calcipotriol ointment and 75% fewer than tacalcitol ointment. Psoriasis affects 0.3 to 2.6% of the population and receptor, acts as a heterodimer with the retinoid X has a significant impact on the patient’s quality of receptor (RXR) [9]. Keratinocytes and lympho- life [1–4]. A 1998 US survey of 17,488 National cytes have vitamin D receptors. In psoriasis, Psoriasis Foundation patient members showed that vitamin D analogues normalize differentiation psoriasis had a significant impact on psychosocial and proliferation, induce apoptosis in inflamma- activities (e.g., interacting in the workplace and tory cells, induce a T-helper (Th)1 to 2 switch with family/spouse, making and keeping friends, and are antiangiogenic [10–12].