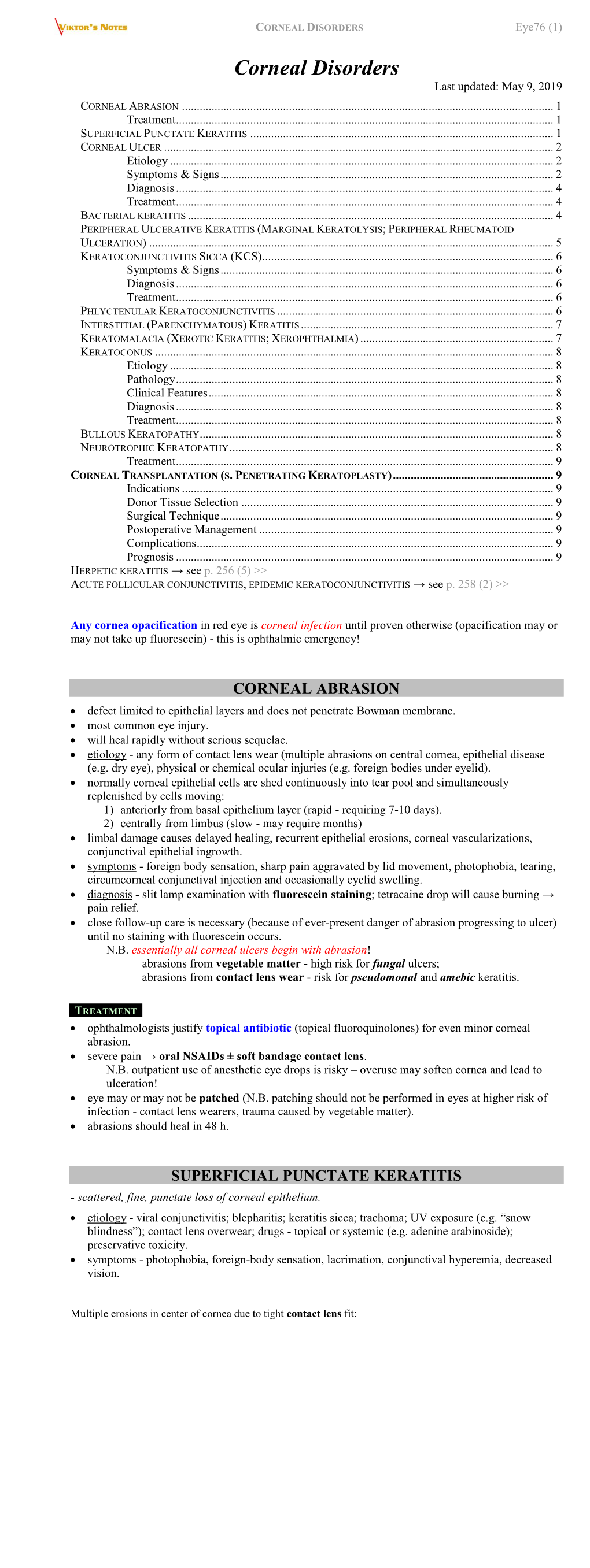
Eye76. Corneal Disorders.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Intraoperative Optical Coherence Tomography Imaging in Corneal Surgery: a Literature Review and Proposal of Novel Applications
Hindawi Journal of Ophthalmology Volume 2020, Article ID 1497089, 10 pages https://doi.org/10.1155/2020/1497089 Research Article Intraoperative Optical Coherence Tomography Imaging in Corneal Surgery: A Literature Review and Proposal of Novel Applications Hiroshi Eguchi ,1 Fumika Hotta,1 Shunji Kusaka,1 and Yoshikazu Shimomura2 1Department of Ophthalmology, Kindai University, Faculty of Medicine, 377-2 Ohnohigashi, Osakasayama, Osaka 589-8511, Japan 2Department of Ophthalmology, Fuchu Eye Center, 1-10-17 Hiko-cho, Izumi, Osaka 594-0076, Japan Correspondence should be addressed to Hiroshi Eguchi; [email protected] Received 26 June 2020; Revised 12 August 2020; Accepted 21 August 2020; Published 11 September 2020 Academic Editor: Sang Beom Han Copyright © 2020 Hiroshi Eguchi et al. &is is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Intraoperative optical coherence tomography (iOCT) is widely used in ophthalmic surgeries for cross-sectional imaging of ocular tissues. &e greatest advantage of iOCTis its adjunct diagnostic efficacy, which facilitates to decision-making during surgery. Since the development of microscopic-integrated iOCT (MIOCT), it has been widely used mainly for vitreoretinal and anterior segment surgeries. In corneal transplantation, MIOCT allows surgeons to visualise structure underneath the turbid and distorted cornea, which are impossible to visualise with a usual microscope. Real-time visualisation of hard-to-see area reduces the operation time and leads to favorable surgical outcomes. &e use of MIOCT is advantageous for a variety of corneal surgical procedures. Here, we have reviewed articles focusing on the utility of iOCT and MIOCTin penetrating keratoplasty, deep anterior lamellar keratoplasty, Descemet stripping automated endothelial keratoplasty, and Descemet membrane endothelial keratoplasty. -

Differentiate Red Eye Disorders
Introduction DIFFERENTIATE RED EYE DISORDERS • Needs immediate treatment • Needs treatment within a few days • Does not require treatment Introduction SUBJECTIVE EYE COMPLAINTS • Decreased vision • Pain • Redness Characterize the complaint through history and exam. Introduction TYPES OF RED EYE DISORDERS • Mechanical trauma • Chemical trauma • Inflammation/infection Introduction ETIOLOGIES OF RED EYE 1. Chemical injury 2. Angle-closure glaucoma 3. Ocular foreign body 4. Corneal abrasion 5. Uveitis 6. Conjunctivitis 7. Ocular surface disease 8. Subconjunctival hemorrhage Evaluation RED EYE: POSSIBLE CAUSES • Trauma • Chemicals • Infection • Allergy • Systemic conditions Evaluation RED EYE: CAUSE AND EFFECT Symptom Cause Itching Allergy Burning Lid disorders, dry eye Foreign body sensation Foreign body, corneal abrasion Localized lid tenderness Hordeolum, chalazion Evaluation RED EYE: CAUSE AND EFFECT (Continued) Symptom Cause Deep, intense pain Corneal abrasions, scleritis, iritis, acute glaucoma, sinusitis, etc. Photophobia Corneal abrasions, iritis, acute glaucoma Halo vision Corneal edema (acute glaucoma, uveitis) Evaluation Equipment needed to evaluate red eye Evaluation Refer red eye with vision loss to ophthalmologist for evaluation Evaluation RED EYE DISORDERS: AN ANATOMIC APPROACH • Face • Adnexa – Orbital area – Lids – Ocular movements • Globe – Conjunctiva, sclera – Anterior chamber (using slit lamp if possible) – Intraocular pressure Disorders of the Ocular Adnexa Disorders of the Ocular Adnexa Hordeolum Disorders of the Ocular -

Cultivating a Cure for Blindness
news and views were taken in a l-mm2 biopsy from the good eye, then they were cultured and, on second Cultivating a cure passage, they formed a tightly packed and communicating (confluent) monolayer of cells. For grafting, the conjunctiva! epi for blindness thelium was completely removed from the cornea and limbus of the recipient eye, and replaced with a slightly larger monolayer of Stuart Hodson cultured limbal epithelium. The eyes were Damaged corneas can often be repaired using donor grafts, but if the then covered with therapeutic soft contact damage is too great the graft wlll be rejected. This may change with the lenses, and tightly patched for several days. development of a method to Inhibit rejection which uses cultivated cells. The results after the limbal epithelial graft were very promising. The grafted epithelium he human cornea has a special proper epithelium can mould a smooth apical and was stable, transparent, multi-layered and Tty known as immune privilege, which basal surface, the limbal epithelial stem cells smooth. One of the patients had suffered an allows tissue grafts from donors to be do not form such a smooth surface. alkali burn to his left eye ten years earlier, and carried out without the usual problems of If the corneal epithelium is lost it can be had undergone three previous unsuccessful immune rejection. However, immune privi functionally regenerated by the limbal stem corneal grafts. Before the treatment he had lege is lost at the perimeter of the cornea - cells. But if both the corneal and limbal continual severe corneal vascularization the limb us of the eye - where the transpar epithelia are lost, the corneal surface is re ( development of blood vessels) and persis ent corneal stroma meets the opaque sclera colonized by the other neighbour of the tent ulceration, and the eye was painful and (Fig. -

Quantitative Assessment of Central and Limbal Epithelium After Long
Eye (2016) 30, 979–986 © 2016 Macmillan Publishers Limited All rights reserved 0950-222X/16 www.nature.com/eye 1,5 1,5 1 Quantitative RK Prakasam , BS Kowtharapu , K Falke , CLINICAL STUDY K Winter2,3, D Diedrich4, A Glass4, A Jünemann1, assessment of central RF Guthoff1 and O Stachs1 and limbal epithelium after long-term wear of soft contact lenses and in patients with dry eyes: a pilot study Abstract Purpose Analysis of microstructural Eye (2016) 30, 979–986; doi:10.1038/eye.2016.58; alterations of corneal and limbal epithelial published online 22 April 2016 cells in healthy human corneas and in other ocular conditions. Introduction Patients and methods Unilateral eyes of three groups of subjects include healthy The X, Y, Z hypothesis1 explains cell mechanism volunteers (G1, n = 5), contact lens wearers that is essential for the renewal and maintenance 1Department of (G2, n = 5), and patients with dry eyes of the corneal epithelium. This hypothesis Ophthalmology, University = proposes that the loss of corneal epithelial of Rostock, Rostock, (G3, n 5) were studied. Imaging of basal Germany (BC) and intermediate (IC) epithelial cells surface cells (Z) can be maintained by the from central cornea (CC), corneal limbus proliferation of basal epithelial cells (X), and the 2Faculty of Medicine, centripetal movements of the peripheral (CL) and scleral limbus (SL) was obtained by Institute of Anatomy, epithelial cells (Y). By utilizing this mechanism, University of Leipzig, in vivo confocal microscopy (IVCM). An it is also possible to categorize both disease and Leipzig, Germany appropriate image analysis algorithm was therapies according to the specific component 3 used to quantify morphometric parameters involved.1 Therefore it is vital to understand the Institute for Medical including mean cell area, compactness, Informatics, Statistics and cellular structures of both central and limbal Epidemiology (IMISE), solidity, major and minor diameter, and epithelial cells in normal and in various corneal University of Leipzig, maximum boundary distance. -
Development of in Vitro Corneal Models: Opportunity for Pharmacological Testing
Review Development of In Vitro Corneal Models: Opportunity for Pharmacological Testing Valentina Citi 1, Eugenia Piragine 1, Simone Brogi 1,* , Sara Ottino 2 and Vincenzo Calderone 1 1 Department of Pharmacy, University of Pisa, Via Bonanno 6, 56126 Pisa, Italy; [email protected] (V.C.); [email protected] (E.P.); [email protected] (V.C.) 2 Farmigea S.p.A., Via G.B. Oliva 6/8, 56121 Pisa, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-050-2219-613 Received: 24 October 2020; Accepted: 30 October 2020; Published: 2 November 2020 Abstract: The human eye is a specialized organ with a complex anatomy and physiology, because it is characterized by different cell types with specific physiological functions. Given the complexity of the eye, ocular tissues are finely organized and orchestrated. In the last few years, many in vitro models have been developed in order to meet the 3Rs principle (Replacement, Reduction and Refinement) for eye toxicity testing. This procedure is highly necessary to ensure that the risks associated with ophthalmic products meet appropriate safety criteria. In vitro preclinical testing is now a well-established practice of significant importance for evaluating the efficacy and safety of cosmetic, pharmaceutical, and nutraceutical products. Along with in vitro testing, also computational procedures, herein described, for evaluating the pharmacological profile of potential ocular drug candidates including their toxicity, are in rapid expansion. In this review, the ocular cell types and functionality are described, providing an overview about the scientific challenge for the development of three-dimensional (3D) in vitro models. -

Neurotrophic Keratopathy and Diabetes Mellitus a Lockwood Et Al 838
Eye (2006) 20, 837–839 & 2006 Nature Publishing Group All rights reserved 0950-222X/06 $30.00 www.nature.com/eye 1 1 2 Neurotrophic A Lockwood , M Hope-Ross and P Chell CASE SERIES keratopathy and diabetes mellitus Abstract no history of previous corneal trauma or herpes simplex infection. Ocular examination revealed Diabetes mellitus is frequently associated a best-corrected visual acuity of 6/12 in both with microvascular complications such as eyes. There was an epithelial irregularity retinopathy, nephropathy, and peripheral extending across the inferonasal quadrant of the neuropathy. Neurotrophic keratopathy occurs right cornea. A diagnosis of exposure in response to a neuropathy of the ophthalmic keratopathy was made. She was treated with division of the trigeminal nerve. Rarely has artificial tears and a month later the epithelium diabetic neurotrophic keratopathy been had healed. A year later, an epithelial defect in described. This paper discusses the the same area was seen at follow-up. Again she ophthalmic histories of three patients who was asymptomatic and the visual acuity was presented with diabetic neurotrophic unchanged. Decreased corneal sensation was keratopathy. In one patient the corneal noted using a cotton swab to touch the ulceration was the sole presenting feature of peripheral and central cornea. A diagnosis of his diabetes. We discuss the need for increased diabetic neurotrophic keratopathy was made. vigilance in the ophthalmic community for She was treated with ocular lubricants. After suspecting diabetes in patients with 6 months, the defect had increased in size to unexplained corneal epithelial disease. 5.5 mm. There was associated corneal Eye (2006) 20, 837–839. -
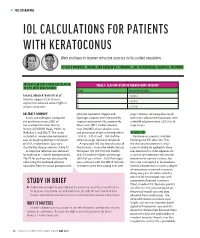
Iol Calculations for Patients with Keratoconus
s THE LITERATURE IOL CALCULATIONS FOR PATIENTS WITH KERATOCONUS Work continues to improve refractive accuracy in this patient population. BY ALICE ROTHWELL, MBCHB, AND ANDREW M.J. TURNBULL, BM, PGCERTMEDED, PGDIPCRS, FRCOPHTH INTRAOCULAR LENS POWER CALCULATION TABLE 1. CLASSIFICATION OF KERATOCONUS SEVERITY IN EYES WITH KERATOCONUS Stage Keratometry Reading Savini G, Abbate R, Hoffer KJ, et al1 1 ≤ 48.00 D Industry support: K.J.H. licenses 2 > 48.00 D registered trademark name Hoffer to various companies 3 > 53.00 D ABSTRACT SUMMARY spherical equivalent. Myopic and stage 1 disease. Accuracy decreased Savini and colleagues compared hyperopic surprises were indicated by with more advanced keratoconus, with the prediction errors (PEs) of negative and positive PEs, respectively. a MedAE of greater than 2.50 D in all five standard formulas: Barrett Mean error (ME), median absolute stage 3 eyes. Universal II (BUII), Haigis, Hoffer Q, error (MedAE), mean absolute error, Holladay 1, and SRK/T. The study and percentage of eyes achieving within DISCUSSION included 41 consecutive keratoconic ±0.50 D, ±0.75 D, and ±1.00 D of the Keratoconus presents multiple eyes undergoing phacoemulsification refractive target were also calculated. challenges to IOL selection. First, and IOL implantation. Eyes were A hyperopic ME was found across all the standard keratometric index classified by disease severity (Table 1). five formulas. Across the whole dataset, cannot reliably be applied to these A subjective refraction was obtained the lowest ME (0.91 D) and MedAE eyes because this index depends on for each eye at 1 month postoperatively. (0.62 D) and the highest percentage a normal ratio between the anterior The PE for each eye was calculated by (36%) of eyes within ±0.50 D of target and posterior corneal surfaces, but subtracting the predicted spherical were achieved with the SRK/T formula. -

Onchocerciasis
11 ONCHOCERCIASIS ADRIAN HOPKINS AND BOAKYE A. BOATIN 11.1 INTRODUCTION the infection is actually much reduced and elimination of transmission in some areas has been achieved. Differences Onchocerciasis (or river blindness) is a parasitic disease in the vectors in different regions of Africa, and differences in cause by the filarial worm, Onchocerca volvulus. Man is the the parasite between its savannah and forest forms led to only known animal reservoir. The vector is a small black fly different presentations of the disease in different areas. of the Simulium species. The black fly breeds in well- It is probable that the disease in the Americas was brought oxygenated water and is therefore mostly associated with across from Africa by infected people during the slave trade rivers where there is fast-flowing water, broken up by catar- and found different Simulium flies, but ones still able to acts or vegetation. All populations are exposed if they live transmit the disease (3). Around 500,000 people were at risk near the breeding sites and the clinical signs of the disease in the Americas in 13 different foci, although the disease has are related to the amount of exposure and the length of time recently been eliminated from some of these foci, and there is the population is exposed. In areas of high prevalence first an ambitious target of eliminating the transmission of the signs are in the skin, with chronic itching leading to infection disease in the Americas by 2012. and chronic skin changes. Blindness begins slowly with Host factors may also play a major role in the severe skin increasingly impaired vision often leading to total loss of form of the disease called Sowda, which is found mostly in vision in young adults, in their early thirties, when they northern Sudan and in Yemen. -

A Description of the Clinical Features of Brimonidine- Associated Uveitis Alyssa Louie Primary Care Resident, San Francisco VA
Drug-induced intraocular inflammation: A description of the clinical features of brimonidine- associated uveitis Alyssa Louie Primary Care Resident, San Francisco VA Abstract: A description of the clinical features, diagnostic work-up, and management of acute anterior uveitis caused by brimonidine, a widely used glaucoma medication. I. Case History a. Patient demographics: 74 year-old white male b. Chief complaint: eye pain, redness, irritation for last 2 weeks c. Ocular and medical history: i. Ocular history 1. Primary open angle glaucoma OU, diagnosed 8 years ago 2. Senile cataracts OU, not visually significant 3. Type 2 Diabetes without retinopathy OU 4. No prior history of uveitis ii. Medical history: Diabetes Mellitus Type 2 iii. No known drug allergies d. Medications i. Ocular: dorzolamide BID OU (1.5 years), brimonidine BID OU (11 months), travatan QHS OU (5.5 years) ii. Medical: metformin 500mg tab BID PO II. Pertinent Findings a. Clinical exam i. Visual acuities: OD 20/20-, OS 20/20- ii. Goldmann applanation tonometry: 13 mm Hg OD, 13 mm Hg OS iii. Anterior segment 1. OU: 3+ diffuse conjunctival injection 2. OU: central and inferior granulomatous keratic precipitates 3. OU: Grade 1+ cell, 1+ flare 4. OU: No synechiae or iris changes were present iv. Posterior segment 1. Optic Nerve a. OD: Cup-to-disc ratio 0.70H/V, distinct margins b. OS: Cup-to-disc ratio 0.75H/V, distinct margins 2. Posterior pole, periphery, vitreous: unremarkable OU b. Laboratory Studies i. ACE, Lysozyme, FTA-ABS, VDRL, HLA-B27, Rheumatoid Factor, ANA, PPD, Chest X- ray: all negative/unreactive III. -

MRSA Ophthalmic Infection, Part 2: Focus on Orbital Cellulitis
Clinical Update COMPREHENSIVE MRSA Ophthalmic Infection, Part 2: Focus on Orbital Cellulitis by gabrielle weiner, contributing writer interviewing preston h. blomquist, md, vikram d. durairaj, md, and david g. hwang, md rbital cellulitis is a poten- Acute MRSA Cellulitis tially sight- and life-threat- ening disease that tops the 1A 1B ophthalmology worry list. Add methicillin-resistant OStaphylococcus aureus (MRSA) to the mix of potential causative bacteria, and the level of concern rises even higher. MRSA has become a relatively prevalent cause of ophthalmic infec- tions; for example, one study showed that 89 percent of preseptal cellulitis S. aureus isolates are MRSA.1 And (1A) This 19-month-old boy presented with left periorbital edema and erythema preseptal cellulitis can rapidly develop five days after having been diagnosed in an ER with conjunctivitis and treated into the more worrisome condition of with oral and topical antibiotics. (1B) Axial CT image of the orbits with contrast orbital cellulitis if not treated promptly shows lacrimal gland abscess and globe displacement. and effectively. Moreover, the community-associ- and Hospital System in Dallas, 86 per- When to Suspect ated form of MRSA (CA-MRSA) now cent of those with preseptal cellulitis MRSA Orbital Cellulitis accounts for a larger proportion of and/or lid abscesses had CA-MRSA. Patients with orbital cellulitis com- ophthalmic cases than health care– These studies also found that preseptal monly complain of pain when moving associated MRSA (HA-MRSA). Thus, cellulitis was the most common oph- the eye, decreased vision, and limited many patients do not have the risk fac- thalmic MRSA presentation from 2000 eye movement. -

Special Considerations in Cataract Surgery: Five Cornea Challenges
Clinical Update EXTRA CONTENT AVAILABLE CATARACT Special Considerations in Cataract Surgery: Five Cornea Challenges by linda roach, contributing writer interviewing preston h. blomquist, md, rosa a. braga-mele, md, kimberly a. drenser, md, phd, herbert e. kaufman, md, marguerite mcdonald, md, and roger f. steinert, md s the most common surgical choices, said Marguerite McDonald, IOL Selection procedure in ophthalmol- MD, of Lynbrook, N.Y. The device en- ogy, replacement of a cloudy ables the surgeon to directly measure 1 crystalline lens with an the eye’s aphakic refractive power in intraocular lens (IOL) usu- the operating room. Aally presents the ophthalmologist with Using intraoperative aberrometry is familiar sets of surgical routines. But becoming more commonplace, as “it what about those cases that involve may help in achieving more accuracy comorbidities or other complicating with IOL power selection,” Dr. Mc- factors? Donald said. Several experts shared their per- Tips on IOL selection. The chosen spectives on approaching out-of-the- IOL should be shaped to neutralize After an off-center LASIK procedure ordinary cataract surgeries in ways spherical aberrations, said Rosa A. such as this, the irregularity of the that offer the best chance at optimiz- Braga-Mele, MD, at the University of corneal topography indicates that a ing patient outcomes. This month, Toronto. “In anybody who has had multifocal IOL should be avoided. here’s a look at five challenges involv- myopic LASIK or PRK, I think it’s very ing the cornea. important to use a negatively aspheric prior to cataract surgery. 2) A dysfunc- IOL, because these patients have more tional, unstable tear film will affect the Challenge: Prior Refractive Surgery positively aberrant corneas. -

Olivia Steinberg ICO Primary Care/Ocular Disease Resident American Academy of Optometry Residents Day Submission
Olivia Steinberg ICO Primary Care/Ocular Disease Resident American Academy of Optometry Residents Day Submission The use of oral doxycycline and vitamin C in the management of acute corneal hydrops: a case comparison Abstract- We compare two patients presenting to clinic with an uncommon complication of keratoconus, acute corneal hydrops. Management of the patients differs. One heals quickly, while the other has a delayed course to resolution. I. Case A a. Demographics: 40 yo AAM b. Case History i. CC: red eye, tearing, decreased VA x 1 day OS ii. POHx: (+) keratoconus OU iii. PMHx: depression, anxiety, asthma iv. Meds: Albuterol, Ziprasidone v. Scleral CL wearer for approximately 6 months OU vi. Denies any pain OS, denies previous occurrence OU, no complaints OD c. Pertinent Findings i. VA cc (CL’s)- 20/25 OD, 20/200 PH 20/60+2 OS ii. Slit Lamp 1. Inferior corneal thinning and Fleisher ring OD, central scarring OD, 2+ diffuse microcystic edema OS, Descemet’s break OS (photos and anterior segment OCT) 2. 2+ diffuse injection OS 3. D&Q A/C OU iii. Intraocular Pressures: deferred OD due to CL, 9mmHg OS (tonopen) iv. Fundus Exam- unremarkable OU II. Case B a. Demographics: 39 yo AAM b. Case History i. CC: painful, red eye, tearing, decreased VA x 1 day OS ii. POHx: unremarkable iii. PMHx: hypertension iv. Meds: unknown HTN medication v. Wears Soflens toric CL’s OU; reports previous doctor had difficulty achieving proper fit OU; denies diagnosis of keratoconus OU vi. Denies any injury OS, denies previous occurrence OU, no complaints OD c.