Consensus Guideline for the Diagnosis and Treatment of Tetrahydrobiopterin
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Folate and Pterin Metabolism by Cancer Cells in Culture1
[CANCER RESEARCH 38, 2378-2384, August 1978) 0008-5472/78/0038-0000$02.00 Folate and Pterin Metabolism by Cancer Cells in Culture1 Baldassarre Stea, Peter S. Backlund, Jr., Phillip B. Berkey, Arthur K. Cho, Barbara C. Halpern, Richard M. Halpern, and Roberts A. Smith2 Departments of Chemistry (B. S., P. S. B., P. B. B., B. C. H.¡,Pharmacology ¡A.K. C.], Medicine, ¡Ft.M. H.]. and Chemistry [Ft. A. SJ and Molecular Biology Institute ¡R.M. H., R. A. S.], University of California, Los Angeles, California 90024 ABSTRACT cells, a significant peak of radioactivity was observed in the blue-fluorescent region. This peak of radioactivity was ab Malignant cells grown in culture excrete into their sent in chromatograms of growth media of normal cells growth medium a folate catabolite that can be seen as a grown under the same conditions. blue-fluorescent region on paper chromatograms of such We tentatively identified this blue-fluorescent compound media. This folate catabolite has now been identified by as Pt-6-CHO,3 primarily on the basis of its inhibitory power paper chromatography, thin-layer chromatography, and toward xanthine oxidase. However, we later found that Pt- combined gas chromatography-mass spectrometry as 6- 6-CH2OH also is a potent inhibitor of the same enzyme hydroxymethylpterin and not as pterin-6-carboxaldehyde system. This prompted us to identify by unequivocal means as previously reported. the fluorescent folate catabolite characteristic of cultured Moreover, when pterin-6-carboxaldehyde was added to malignant cells. the growth medium of logarithmically growing malignant Here we report the definitive identification of this blue- cells, it was primarily reduced to 6-hydroxymethylpterin. -
Guide for Hyperphenylalaninemia
TM Guide For Hyperphenylalaninemia Laurie Bernstein, MS, RD, FADA Cindy Freehauf, RN, CGC Laurie Bernstein, MS, RD, FADA Fellow of the American Dietetic Association Assistant Professor- Department of Pediatrics Director, IMD Nutrition The Children's Hospital, Aurora CO Cindy Freehauf, RN, CGC Assistant Professor- Department of Pediatrics Clinical Coordinator, IMD Clinic The Children's Hospital, Aurora CO A special thank you to: Kathleen M. Martin, BS, BA for her enthusiasm for learning and excellent graphic skills. Intern, IMD Clinic The Children's Hospital, Aurora CO Second Edition Review Committee: Casey Burns, RD Janet A. Thomas, MD Metabolic Nutritionist Associate Professor, Pediatrics The Children's Hospital, Aurora CO Director, IMD Clinic The Children's Hospital, Aurora CO Sommer Myers, RD Metabolic Nutritionist Erica L. Wright, MS, CGC The Children's Hospital, Aurora CO Certified Genetic Counselor The Children's Hospital, Aurora CO Shannon L. Scrivner, MS, CGC Certified Genetic Counselor The Children's Hospital, Aurora CO Acknowledgments: Educational grant provided by Nutricia North America The Genetic Counseling Graduate Students of The University of Colorado at Denver and Health Sciences Center. TCH logo is a Licensed Trademark, all rights reserved. The Inherited Metabolic Clinic at The Children’s Hospital in Aurora, CO serves the Rocky Mountain Plains Region and at least 130 individuals with hyperphenylalaninemia (PKU). Children and families require a great deal of complex information, most often new and alien to their experience, in order to establish and maintain consistent and effective treatment. Our experience with the process of sharing such information with families motivated us develop this anticipatory guidance book with teaching aids. -
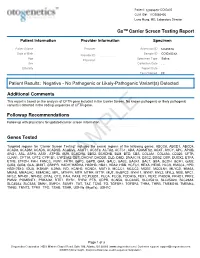
PDF Document Created by Pdffiller
Patient: 1234567843314948-COtGx0053 CLIA ID#: 11D2066426 Larry Hung, MD, Laboratory Director GxTM Carrier Screen Testing Report Patient Information Provider Information Specimen Patient Name Haley Papevies Provider Harbin Clinic Women's Accession ID 1234567843314948 Center Cartersville Date of Birth Apr 16, 1998 Sample ID COtGx0053XX Provider ID 1124488556 Age 19 Specimen Type Saliva Physician Vicki Yates Sex female Collection Date Jul 20, 2017 Ethnicity Report Date Aug 5, 2017 Test Ordered CF Patient Results: Negative - No Pathogenic or Likely-Pathogenic Variant(s) Detected Additional Comments This report is based on the analysis of CFTR gene included in the Carrier Screen. No known pathogenic or likely pathogenic variant(s) detected in the coding sequences of CFTR gene. Followup Recommendations Follow up with physicians for updated carrier screen information. The sequencing for CFTR gene was carried out with the other genes included in the Carrier Screen Testing (listed below). The analysis of the other genes in the Carrier Screen could be ordered through your physicians. Genes Tested Targeted regions for “Carrier Screen Testing” includes the exonic regions of the following genes: ABCC8, ABCD1, ABCD4, ACAD8, ACADM, ACADS, ACADSB, ACADVL, ACAT1, ACSF3, ACTA2, ACTC1, ADA, ADAMTS2, AGXT, AHCY, APC, APOB, ARG1, ASL, ASPA, ASS1, ATP7B, AUH, BCKDHA, BBS2, BCKDHB, BLM, BTD, CBS, COL3A1, COL4A3, CD320, CFTR, CLRN1, CPT1A, CPT2, CYP1B1, CYP21A2, DBT, DHCR7, DHDDS, DLD, DMD, DNAJC19, DSC2, DSG2, DSP, DUOX2, ETFA, ETFB, ETFDH, FAH, FANCC, FBN1, -

Incidence of Inborn Errors of Metabolism by Expanded Newborn
Original Article Journal of Inborn Errors of Metabolism & Screening 2016, Volume 4: 1–8 Incidence of Inborn Errors of Metabolism ª The Author(s) 2016 DOI: 10.1177/2326409816669027 by Expanded Newborn Screening iem.sagepub.com in a Mexican Hospital Consuelo Cantu´-Reyna, MD1,2, Luis Manuel Zepeda, MD1,2, Rene´ Montemayor, MD3, Santiago Benavides, MD3, Hector´ Javier Gonza´lez, MD3, Mercedes Va´zquez-Cantu´,BS1,4, and Hector´ Cruz-Camino, BS1,5 Abstract Newborn screening for the detection of inborn errors of metabolism (IEM), endocrinopathies, hemoglobinopathies, and other disorders is a public health initiative aimed at identifying specific diseases in a timely manner. Mexico initiated newborn screening in 1973, but the national incidence of this group of diseases is unknown or uncertain due to the lack of large sample sizes of expanded newborn screening (ENS) programs and lack of related publications. The incidence of a specific group of IEM, endocrinopathies, hemoglobinopathies, and other disorders in newborns was obtained from a Mexican hospital. These newborns were part of a comprehensive ENS program at Ginequito (a private hospital in Mexico), from January 2012 to August 2014. The retrospective study included the examination of 10 000 newborns’ results obtained from the ENS program (comprising the possible detection of more than 50 screened disorders). The findings were the following: 34 newborns were confirmed with an IEM, endocrinopathies, hemoglobinopathies, or other disorders and 68 were identified as carriers. Consequently, the estimated global incidence for those disorders was 3.4 in 1000 newborns; and the carrier prevalence was 6.8 in 1000. Moreover, a 0.04% false-positive rate was unveiled as soon as diagnostic testing revealed negative results. -

Enzymatic Encoding Methods for Efficient Synthesis Of
(19) TZZ__T (11) EP 1 957 644 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: C12N 15/10 (2006.01) C12Q 1/68 (2006.01) 01.12.2010 Bulletin 2010/48 C40B 40/06 (2006.01) C40B 50/06 (2006.01) (21) Application number: 06818144.5 (86) International application number: PCT/DK2006/000685 (22) Date of filing: 01.12.2006 (87) International publication number: WO 2007/062664 (07.06.2007 Gazette 2007/23) (54) ENZYMATIC ENCODING METHODS FOR EFFICIENT SYNTHESIS OF LARGE LIBRARIES ENZYMVERMITTELNDE KODIERUNGSMETHODEN FÜR EINE EFFIZIENTE SYNTHESE VON GROSSEN BIBLIOTHEKEN PROCEDES DE CODAGE ENZYMATIQUE DESTINES A LA SYNTHESE EFFICACE DE BIBLIOTHEQUES IMPORTANTES (84) Designated Contracting States: • GOLDBECH, Anne AT BE BG CH CY CZ DE DK EE ES FI FR GB GR DK-2200 Copenhagen N (DK) HU IE IS IT LI LT LU LV MC NL PL PT RO SE SI • DE LEON, Daen SK TR DK-2300 Copenhagen S (DK) Designated Extension States: • KALDOR, Ditte Kievsmose AL BA HR MK RS DK-2880 Bagsvaerd (DK) • SLØK, Frank Abilgaard (30) Priority: 01.12.2005 DK 200501704 DK-3450 Allerød (DK) 02.12.2005 US 741490 P • HUSEMOEN, Birgitte Nystrup DK-2500 Valby (DK) (43) Date of publication of application: • DOLBERG, Johannes 20.08.2008 Bulletin 2008/34 DK-1674 Copenhagen V (DK) • JENSEN, Kim Birkebæk (73) Proprietor: Nuevolution A/S DK-2610 Rødovre (DK) 2100 Copenhagen 0 (DK) • PETERSEN, Lene DK-2100 Copenhagen Ø (DK) (72) Inventors: • NØRREGAARD-MADSEN, Mads • FRANCH, Thomas DK-3460 Birkerød (DK) DK-3070 Snekkersten (DK) • GODSKESEN, -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Generated by SRI International Pathway Tools Version 25.0, Authors S
An online version of this diagram is available at BioCyc.org. Biosynthetic pathways are positioned in the left of the cytoplasm, degradative pathways on the right, and reactions not assigned to any pathway are in the far right of the cytoplasm. Transporters and membrane proteins are shown on the membrane. Periplasmic (where appropriate) and extracellular reactions and proteins may also be shown. Pathways are colored according to their cellular function. Gcf_000238675-HmpCyc: Bacillus smithii 7_3_47FAA Cellular Overview Connections between pathways are omitted for legibility. -

Malignant Hyperphenylalaninemia Tetrahydrobiopterin (BH4) Phenylalanine
Pediat. Res. 13: 1 150-1 155 (1979) Dihydropterine reductase (DHPR) phenylketonuria malignant hyperphenylalaninemia tetrahydrobiopterin (BH4) phenylalanine Malignant Hyperphenylalaninemia-Clinical Features, Biochemical Findings, and Experience with Administration of Biopterins D. M. DANKS, P. SCHLESINGER, F. FIRGAIRA, R. G. H. COTTON. B. M. WATSON, H. REMBOLD. AND G. HENNINGS Genetics Research Unit, Royal Children S Hospital Research Foundation, and Department of Paediatrics, Universi1.y of Melbourne, Parkville, Australia (D. M. D., P. S., F. F.. R. G. H. C., B. M. W.) and Max Planck Institutfur Biochemie. Germany (H. R., G. H.) Summary has been attributed to defective production of neurotransmitters derived from hydroxylation of tyrosine and of tryptophan (3, 4). Four cases of malignant hyperphenylalaninemia (MHPA) are The results of treatment with L-dopa and 5-hydroxytryptophan described. Pretreatment serum phenylalanine levels were 1.5, 3.0, support this contention (2, 3. 7). 2.4, and 0.9 mmoles/l. Dihydropteridine reductase (DHPR) defi- Four patients with MHPA seen in Melbourne since 1963 are ciency was proven in one patient by assays on cultured fibroblastic presented. One patient has been shown to have DHPR deficiency cells and was presumed in her sibling and in another deceased and her sister is presumed to have died of this defect. Both parents patient whose parents' fibroblastic cells show approximately 50% of another baby had DHPR levels in the heterozygote range of normal enzyme activity. DHPR and phenylalanine hydroxylase suggesting DHPR deficiency as the cause of her death. The 4th deficiency were excluded by assays on liver obtained at autopsy in baby had neither PH or DHPR deficiency and defective BH4 the 4th patient. -

Identification of Ataxia-Associated Mtdna Mutations (M.4052T>C And
tapraid5/za3-mus/za3-mus/za300909/za32342d09g knepper1 Sϭ7 7/20/09 11:41 Art: 08-0574 ABSTRACT: The potential pathogenicity of two homoplasmic mtDNA point mu- tations, 9035TϾC and 4452TϾC, found in a family afflicted with maternally trans- mitted cognitive developmental delay, learning disability, and progressive ataxia was evaluated using transmitochondrial cybrids. We confirmed that the 4452TϾC transition in tRNAMet represented a polymorphism; however, 9035TϾC conversion in the ATP6 gene was responsible for a defective F0-ATPase. Accordingly, mutant cybrids had a reduced oligomycin-sensitive ATP hydrolyzing activity. They had less than half of the steady-state content of ATP and nearly an 8-fold higher basal level of reactive oxygen species (ROS). Mutant cybrids were unable to cope with addi- tional insults, i.e., glucose deprivation or tertiary-butyl hydroperoxide, and they succumbed to either apoptotic or necrotic cell death. Both of these outcomes were prevented by the antioxidants CoQ10 and vitamin E, suggesting that the abnormally high levels of ROS were the triggers of cell death. In conclusion, the principal metabolic defects, i.e., energy deficiency and ROS burden, resulted from the 9035TϾC mutation and could be responsible for the development of clinical symp- toms in this family. Furthermore, antioxidant therapy might prove helpful in the management of this disease. Muscle Nerve 39: 000–000, 2009 IDENTIFICATION OF ATAXIA-ASSOCIATED mtDNA MUTATIONS (m.4052T>C and m.9035T>C) AND EVALUATION OF THEIR PATHOGENICITY IN TRANSMITOCHONDRIAL CYBRIDS MARIANNA SIKORSKA, PhD,1 JAGDEEP K. SANDHU, PhD,1 DAVID K. SIMON, MD, PhD,2 VIMUKTHI PATHIRAJA, MD,2 CAROLINE SODJA, MSc,1 YAN LI, MD,1 MARIA RIBECCO-LUTKIEWICZ, PhD,1 PATRICIA LANTHIER, BSc,1 HENRYK BOROWY-BOROWSKI, PhD,1 ADRIAN UPTON, MD, PhD,3 SANDEEP RAHA, PhD,4 STEFAN M. -

Oral Presentations
Journal of Inherited Metabolic Disease (2018) 41 (Suppl 1):S37–S219 https://doi.org/10.1007/s10545-018-0233-9 ABSTRACTS Oral Presentations PARALLEL SESSION 1A: Clycosylation and cardohydrate disorders O-002 Link between glycemia and hyperlipidemia in Glycogen Storage O-001 Disease type Ia Hoogerland J A1, Hijmans B S1, Peeks F1, Kooijman S3, 4, Bos T2, Fertility in classical galactosaemia, N-glycan, hormonal and inflam- Bleeker A1, Van Dijk T H2, Wolters H1, Havinga R1,PronkACM3, 4, matory gene expression interactions Rensen P C N3, 4,MithieuxG5, 6, Rajas F5, 6, Kuipers F1, 2,DerksTGJ1, Reijngoud D1,OosterveerMH1 Colhoun H O1,Rubio-GozalboME2,BoschAM3, Knerr I4,DawsonC5, Brady J J6,GalliganM8,StepienKM9, O'Flaherty R O7,MossC10, 1Dep Pediatrics, CLDM, Univ of Groningen, Groningen, Barker P11, Fitzgibbon M C6, Doran P8,TreacyEP1, 4, 9 Netherlands, 2Lab Med, CLDM, Univ of Groningen, Groningen, Netherlands, 3Dep of Med, Div of Endocrinology, LUMC, Leiden, 1Dept Paediatrics, Trinity College Dublin, Dublin, Ireland, 2Dept Paeds and Netherlands, 4Einthoven Lab Exp Vasc Med, LUMC, Leiden, Clin Genetics, UMC, Maastricht, Netherlands, 3Dept Paediatrics, AMC, Netherlands, 5Institut Nat Sante et Recherche Med, Lyon, Amsterdam, Netherlands, 4NCIMD, TSCUH, Dublin, Ireland, 5Dept France, 6Univ Lyon 1, Villeurbanne, France Endocrinology, NHS Foundation Trust, Birmingham, United Kingdom, 6Dept Clin Biochem, MMUH, Dublin, Ireland, 7NIBRT Glycoscience, Background: Glycogen Storage Disease type Ia (GSD Ia) is an NIBRT, Dublin, Ireland, 8UCDCRC,UCD,Dublin,Ireland,9NCIMD, inborn error of glucose metabolism characterized by fasting hypo- MMUH, Dublin, Ireland, 10Conway Institute, UCD, Dublin, Ireland, glycemia, hyperlipidemia and fatty liver disease. We have previ- 11CBAL, NHS Foundation, Cambridge, United Kingdom ously reported considerable heterogeneity in circulating triglycer- ide levels between individual GSD Ia patients, a phenomenon that Background: Classical Galactosaemia (CG) is caused by deficiency of is poorly understood. -

Circuits Regulating Superoxide and Nitric Oxide
antioxidants Article Circuits Regulating Superoxide and Nitric Oxide Production and Neutralization in Different Cell Types: Expression of Participating Genes and Changes Induced by Ionizing Radiation 1,2, 1,2, 1 1,2, Patryk Bil y, Sylwia Ciesielska y, Roman Jaksik and Joanna Rzeszowska-Wolny * 1 Department of Systems Biology and Engineering, Faculty of Automatic Control, Electronics and Computer Science, Silesian University of Technology, 44-100 Gliwice, Poland; [email protected] (P.B.); [email protected] (S.C.); [email protected] (R.J.) 2 Biotechnology Centre, Silesian University of Technology, 44-100 Gliwice, Poland * Correspondence: [email protected] These authors contributed equally. y Received: 30 June 2020; Accepted: 29 July 2020; Published: 3 August 2020 Abstract: Superoxide radicals, together with nitric oxide (NO), determine the oxidative status of cells, which use different pathways to control their levels in response to stressing conditions. Using gene expression data available in the Cancer Cell Line Encyclopedia and microarray results, we compared the expression of genes engaged in pathways controlling reactive oxygen species and NO production, neutralization, and changes in response to the exposure of cells to ionizing radiation (IR) in human cancer cell lines originating from different tissues. The expression of NADPH oxidases and NO synthases that participate in superoxide radical and NO production was low in all cell types. Superoxide dismutase, glutathione peroxidase, thioredoxin, and peroxiredoxins participating in radical neutralization showed high expression in nearly all cell types. Some enzymes that may indirectly influence superoxide radical and NO levels showed tissue-specific expression and differences in response to IR. -

Tetrahydrobiopterin Loading Test in Hyperphenylalaninemia
003 1-399819113005-0435$03.00/0 PEDIATRIC RESEARCH Vol. 30, No. 5, 1991 Copyright 0 199 1 International Pediatric Research Foundation, Inc. Pr~ntc.d in U.S. A Tetrahydrobiopterin Loading Test in Hyperphenylalaninemia ALBERT0 PONZONE, ORNELLA GUARDAMAGNA, SILVIO FERRARIS, GIOVANNI B. FERRERO, IRMA DIANZANI, AND RICHARD G. H. COTTON InstiflifeofPediatric Clinic(A.P., O.G., S.F., G.B.F., I.D.], University of Torino, 10126 Torino, Italy and Olive Miller Laboratory [R.G.H.C.],Murdoch Institute, Royal Children's Hospital, Vicroria,Australia 3052 ABSTRACT. Some cases of primary hyperphenylalanine- PKU to describe some cases clinically unresponsive to a Phe- mia are not caused by the lack of phenylalanine hydroxyl- restricted diet and later shown to be due to BH4 deficiency ase, but by the lack of its cofactor tetrahydrobiopterin. ( 1-4). These patients are not clinically responsive to a phenylal- By analyzing all the essential components of the complex anine-restricted diet, but need specific substitution therapy. hydroxylation system of aromatic amino acids, it became appar- Thus, it became necessary to examine all newborns ent that a defect in the BH4 recycling enzyme DHPR (EC screened as positive with the Guthrie test for tetrahydro- 1.66.99.7) and two defects in BH4 synthetic pathway enzymes, biopterin deficiency. Methods based on urinary pterin or guanosine triphosphate cyclohydrolase I (EC 3.5.4.16) and 6- on specific enzyme activity measurements are limited in PPH4S, may lead to cofactor deficiency resulting in HPA and in their availability, and the simplest method, based on the impaired production of dopamine and serotonin (5-7).