Emerging Infectious Diseases of Chelonians
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Disease of Aquatic Organisms 105:1
Vol. 105: 1–8, 2013 DISEASES OF AQUATIC ORGANISMS Published July 9 doi: 10.3354/dao02594 Dis Aquat Org Megalocytivirus infection in orbiculate batfish Platax orbicularis Preeyanan Sriwanayos1, Ruth Francis-Floyd1,2, Mark F. Stidworthy3, Barbara D. Petty1,2, Karen Kelley4, Thomas B. Waltzek5,* 1Program in Fisheries and Aquatic Sciences, School of Forestry Resources and Conservation, University of Florida, Gainesville, Florida 32653, USA 2Department of Large Animal Clinical Sciences, College of Veterinary Medicine, University of Florida, Gainesville, Florida 32610, USA 3International Zoo Veterinary Group, Station House, Parkwood Street, Keighley, West Yorkshire BD21 4NQ, UK 4Interdisciplinary Center for Biotechnology Research (ICBR), Cellomics Division, Electron Microscopy and Bio-imaging Core Laboratory, University of Florida, Gainesville, Florida 32611, USA 5Department of Infectious Diseases and Pathology, College of Veterinary Medicine, University of Florida, Gainesville, Florida 32608, USA ABSTRACT: Megalocytiviruses cause systemic disease in both marine and freshwater fishes, neg- atively impacting ornamental and food fish aquaculture. In this report, we characterize a megalo- cytivirus infection in a captive marine ornamental fish, the orbiculate batfish Platax orbicularis. Histologic examination revealed cytomegalic cells characterized by strongly basophilic granular intracytoplasmic inclusions within various organs. Transmission electron microscopy revealed icosahedral virus particles within the cytoplasm of cytomegalic cells consistent -

Body Condition Assessment – As a Welfare and Management Assessment Tool for Radiated Tortoises (Astrochelys Radiata)
Body condition assessment – as a welfare and management assessment tool for radiated tortoises (Astrochelys radiata) Hullbedömning - som ett verktyg för utvärdering av välfärd och skötsel av strålsköldpadda (Astrochelys radiata) Linn Lagerström Independent project • 15 hp Swedish University of Agricultural Sciences, SLU Department of Animal Environment and Health Programme/Education Uppsala 2020 2 Body condition assessment – as a welfare and management tool for radiated tortoises (Astrochelys radiata) Hullbedömning - som ett verktyg för utvärdering av välfärd och skötsel av strålsköldpadda (Astrochelys radiata) Linn Lagerström Supervisor: Lisa Lundin, Swedish University of Agricultural Sciences, Department of Animal Environment and Health Examiner: Maria Andersson, Swedish University of Agricultural Sciences, Department of Animal Environment and Health Credits: 15 hp Level: First cycle, G2E Course title: Independent project Course code: EX0894 Programme/education: Course coordinating dept: Department of Aquatic Sciences and Assessment Place of publication: Uppsala Year of publication: 2020 Cover picture: Linn Lagerström Keywords: Tortoise, turtle, radiated tortoise, Astrochelys radiata, Geochelone radiata, body condition indices, body condition score, morphometrics Swedish University of Agricultural Sciences Faculty of Natural Resources and Agricultural Sciences Department of Animal Environment and Health 3 Publishing and archiving Approved students’ theses at SLU are published electronically. As a student, you have the copyright to your own work and need to approve the electronic publishing. If you check the box for YES, the full text (pdf file) and metadata will be visible and searchable online. If you check the box for NO, only the metadata and the abstract will be visiable and searchable online. Nevertheless, when the document is uploaded it will still be archived as a digital file. -

Coccidiosis in Large and Small Ruminants
Coccidiosis in Large and Small Ruminants a, b Sarah Tammy Nicole Keeton, PhD, MS *, Christine B. Navarre, DVM, MS KEYWORDS Coccidia Coccidiosis Diarrhea Ruminants Cattle Sheep Goats Ionophores KEY POINTS Coccidiosis is an important parasitic disease of ruminant livestock caused by the proto- zoan parasite of the genus Eimeria. Calves between 6 and 12 months of age and lambs and kids between 1 and 6 months of age are most susceptible. Subclinical disease is characterized by poor growth. Clinical disease is most commonly characterized by diarrhea. Control of coccidiosis is based on sound management, the use of preventive medications, and treatment of clinical cases as necessary. INTRODUCTION: NATURE OF THE PROBLEM Coccidiosis is a parasitic disease of vertebrate animals, including domestic ruminants.1 It is economically significant, with losses from both clinical and subclinical disease. Coccidiosis is caused by the protozoan parasite of the genus Eimeria. Eimeria are host specific, meaning that an Eimeria species that infect goats does not infect sheep or cattle and vice versa. Certain species of Eimeria are nonpathogenic and do not cause disease. The pathogenic species and sites of infection are listed in Table 1. Mixed infections with multiple pathogenic and nonpathogenic species is common. LIFE CYCLE Proper treatment and control of coccidiosis requires an understanding of the complex life cycle and transmission of Eimeria spp (Fig. 1). The life cycle can be divided into Disclosure: The authors have nothing to disclose. a Department of Veterinary Clinical Sciences, School of Veterinary Medicine, Louisiana State University, Skip Bertman Drive, Baton Rouge, LA 70803, USA; b LSU AgCenter, School of Animal Sciences, Louisiana State University, 111 Dalrymple Bldg, 110 LSU Union Square, Baton Rouge, LA 70803-0106, USA * Corresponding author. -

English and French Cop17 Inf
Original language: English and French CoP17 Inf. 36 (English and French only / Únicamente en inglés y francés / Seulement en anglais et français) CONVENTION ON INTERNATIONAL TRADE IN ENDANGERED SPECIES OF WILD FAUNA AND FLORA ____________________ Seventeenth meeting of the Conference of the Parties Johannesburg (South Africa), 24 September – 5 October 2016 JOINT STATEMENT REGARDING MADAGASCAR’S PLOUGHSHARE / ANGONOKA TORTOISE 1. This document has been submitted by the United States of America at the request of the Wildlife Conservation Society, Durrell Wildlife Conservation Trust, Turtle Survival Alliance, and The Turtle Conservancy, in relation to agenda item 73 on Tortoises and freshwater turtles (Testudines spp.)*. 2. This species is restricted to a limited range in northwestern Madagascar. It has been included in CITES Appendix I since 1975 and has been categorized as Critically Endangered on the IUCN Red List of Threatened Species since 2008. There has been a significant increase in the level of illegal collection and trafficking of this species to supply the high end pet trade over the last 5 years. 3. Attached please find the joint statement regarding Madagascar’s Ploughshare/Angonoka Tortoise, which is considered directly relevant to Document CoP17 Doc. 73 on tortoises and freshwater turtles. * The geographical designations employed in this document do not imply the expression of any opinion whatsoever on the part of the CITES Secretariat (or the United Nations Environment Programme) concerning the legal status of any country, territory, or area, or concerning the delimitation of its frontiers or boundaries. The responsibility for the contents of the document rests exclusively with its author. -

Whole Blood Fatty Acid Concentrations in the San Cristóbal Galápagos Tortoise (Chelonoidis Chathamensis)
Whole blood fatty acid concentrations in the San Cristóbal Galápagos tortoise (Chelonoidis chathamensis) Khushboo Dass1, Gregory A. Lewbart1, Juan Pablo Muñoz-Pérez2,3, Maryuri I. Yépez4, Andrea Loyola4, Emile Chen5 and Diego Páez-Rosas3 1 Department of Clinical Sciences, College of Veterinary Medicine, North Carolina State University, Raleigh, NC, United States of America 2 Faculty of Science and Engineering, University of the Sunshine Coast, Sippy Downs, Queensland, Australia 3 USFQ & UNC-Chapel Hill Galápagos Science Center (GSC), Universidad San Francisco de Quito, Quito, Ecuador 4 Direcion Parque Nacional Galápagos, Islas Galápagos, Ecuador 5 9 Oneida Court, Chester Springs, PA, United States of America ABSTRACT To continue releasing San Cristóbal Galápagos tortoises housed in managed-care facil- ities at the Giant Tortoise Breeding Center of Galápagos National Park (Galapaguera de Cerro Colorado) to the Otoy Ecological Farm, health assessments and physical examinations were conducted. As a part of these wellness examinations, blood was drawn from 11 tortoises to analyze fatty acid concentrations. Fatty acid levels can provide insight into the nutritional profiles, immune status, and reproductive health of vertebrates. To the co-author's knowledge, there is no current information about fatty acids in this species. It was hypothesized that there would be inherent differences based on the different geographic ranges, diets, sex, and age of turtles. It was noted that the !-6/!-3 ratio was higher for the breeding center than for the ecological farm and that overall polyunsaturated fatty acids (PUFAs) did not have any significant differences. The !-6/!-3 findings can contribute to a global picture of these fatty acids across taxa, as reptiles are underrepresented in this area of research. -
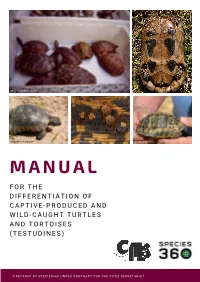
Manual for the Differentiation of Captive-Produced and Wild-Caught Turtles and Tortoises (Testudines)
Image: Peter Paul van Dijk Image:Henrik Bringsøe Image: Henrik Bringsøe Image: Andrei Daniel Mihalca Image: Beate Pfau MANUAL F O R T H E DIFFERENTIATION OF CAPTIVE-PRODUCED AND WILD-CAUGHT TURTLES AND TORTOISES (TESTUDINES) PREPARED BY SPECIES360 UNDER CONTRACT FOR THE CITES SECRETARIAT Manual for the differentiation of captive-produced and wild-caught turtles and tortoises (Testudines) This document was prepared by Species360 under contract for the CITES Secretariat. Principal Investigators: Prof. Dalia A. Conde, Ph.D. and Johanna Staerk, Ph.D., Species360 Conservation Science Alliance, https://www.species360.orG Authors: Johanna Staerk1,2, A. Rita da Silva1,2, Lionel Jouvet 1,2, Peter Paul van Dijk3,4,5, Beate Pfau5, Ioanna Alexiadou1,2 and Dalia A. Conde 1,2 Affiliations: 1 Species360 Conservation Science Alliance, www.species360.orG,2 Center on Population Dynamics (CPop), Department of Biology, University of Southern Denmark, Denmark, 3 The Turtle Conservancy, www.turtleconservancy.orG , 4 Global Wildlife Conservation, globalwildlife.orG , 5 IUCN SSC Tortoise & Freshwater Turtle Specialist Group, www.iucn-tftsG.org. 6 Deutsche Gesellschaft für HerpetoloGie und Terrarienkunde (DGHT) Images (title page): First row, left: Mixed species shipment (imaGe taken by Peter Paul van Dijk) First row, riGht: Wild Testudo marginata from Greece with damaGe of the plastron (imaGe taken by Henrik BrinGsøe) Second row, left: Wild Testudo marginata from Greece with minor damaGe of the carapace (imaGe taken by Henrik BrinGsøe) Second row, middle: Ticks on tortoise shell (Amblyomma sp. in Geochelone pardalis) (imaGe taken by Andrei Daniel Mihalca) Second row, riGht: Testudo graeca with doG bite marks (imaGe taken by Beate Pfau) Acknowledgements: The development of this manual would not have been possible without the help, support and guidance of many people. -

The Conservation Biology of Tortoises
The Conservation Biology of Tortoises Edited by Ian R. Swingland and Michael W. Klemens IUCN/SSC Tortoise and Freshwater Turtle Specialist Group and The Durrell Institute of Conservation and Ecology Occasional Papers of the IUCN Species Survival Commission (SSC) No. 5 IUCN—The World Conservation Union IUCN Species Survival Commission Role of the SSC 3. To cooperate with the World Conservation Monitoring Centre (WCMC) The Species Survival Commission (SSC) is IUCN's primary source of the in developing and evaluating a data base on the status of and trade in wild scientific and technical information required for the maintenance of biological flora and fauna, and to provide policy guidance to WCMC. diversity through the conservation of endangered and vulnerable species of 4. To provide advice, information, and expertise to the Secretariat of the fauna and flora, whilst recommending and promoting measures for their con- Convention on International Trade in Endangered Species of Wild Fauna servation, and for the management of other species of conservation concern. and Flora (CITES) and other international agreements affecting conser- Its objective is to mobilize action to prevent the extinction of species, sub- vation of species or biological diversity. species, and discrete populations of fauna and flora, thereby not only maintain- 5. To carry out specific tasks on behalf of the Union, including: ing biological diversity but improving the status of endangered and vulnerable species. • coordination of a programme of activities for the conservation of biological diversity within the framework of the IUCN Conserva- tion Programme. Objectives of the SSC • promotion of the maintenance of biological diversity by monitor- 1. -

Development of a Canine Coccidiosis Model and the Anticoccidial Effects of a New Chemotherapeutic Agent
DEVELOPMENT OF A CANINE COCCIDIOSIS MODEL AND THE ANTICOCCIDIAL EFFECTS OF A NEW CHEMOTHERAPEUTIC AGENT Sheila Mitchell Dissertation submitted to the faculty of the Virginia Polytechnic Institute and State University in partial fulfillment of the requirements for the degree of Doctor of Philosophy In Biomedical and Veterinary Sciences David S. Lindsay Anne M. Zajac Nammalwar Sriranganathan Sharon G. Witonsky Byron L. Blagburn April 11, 2008 Blacksburg, Virginia Keywords: Apicomplexa, coccidia, canine, animal model, monozoic cyst, cell culture, Toxoplasma gondii, treatment DEVELOPMENT OF A CANINE COCCIDIOSIS MODEL AND THE ANTICOCCIDIAL EFFECTS OF A NEW CHEMOTHERAPEUTIC AGENT Sheila Mitchell ABSTRACT Coccidia are obligate intracellular parasites belonging to the phylum Apicomplexa. Many coccidia are of medical and veterinary importance such as Cystoisospora species and Toxoplasma gondii. The need to discover new anticoccidial therapies has increased due to development of resistance by the parasite or toxicity issues in the patient. The goals of this work were to develop a model for canine coccidiosis while proving that Cystoisospora canis is a true primary pathogen in dogs and to determine the efficacy of a new anticoccidial agent. A canine coccidiosis model would be useful in evaluating new anticoccidial treatments. Oral infections with 5 X 104 (n=2) and 1 X 105 (n=20) sporulated C. canis oocysts were attempted in 22 purpose bred beagle puppies. Clinical signs associated with disease were observed in all dogs. Bacterial and viral pathogens were ruled out by transmission electron microscopy (TEM) and bacterial growth assays. Development of C. canis in cell culture was also evaluated. The efficacy of ponazuril, a new anticoccidial drug, was examined in T. -

The DNA Virus Invertebrate Iridescent Virus 6 Is a Target of the Drosophila Rnai Machinery
The DNA virus Invertebrate iridescent virus 6 is a target of the Drosophila RNAi machinery Alfred W. Bronkhorsta,1, Koen W. R. van Cleefa,1, Nicolas Vodovarb,2, Ikbal_ Agah Ince_ c,d,e, Hervé Blancb, Just M. Vlakc, Maria-Carla Salehb,3, and Ronald P. van Rija,3 aDepartment of Medical Microbiology, Nijmegen Centre for Molecular Life Sciences, Nijmegen Institute for Infection, Inflammation, and Immunity, Radboud University Nijmegen Medical Centre, 6500 HB Nijmegen, The Netherlands; bViruses and RNA Interference Group, Institut Pasteur, Centre National de la Recherche Scientifique, Unité de Recherche Associée 3015, 75015 Paris, France; cLaboratory of Virology, Wageningen University, 6708 PB Wageningen, The Netherlands; dDepartment of Genetics and Bioengineering, Yeditepe University, Istanbul 34755, Turkey; and eDepartment of Biosystems Engineering, Faculty of Engineering, Giresun University, Giresun 28100, Turkey Edited by Peter Palese, Mount Sinai School of Medicine, New York, NY, and approved October 19, 2012 (received for review April 28, 2012) RNA viruses in insects are targets of an RNA interference (RNAi)- sequently, are hypersensitive to virus infection and succumb more based antiviral immune response, in which viral replication inter- rapidly than their wild-type (WT) controls (11–14). mediates or viral dsRNA genomes are processed by Dicer-2 (Dcr-2) Small RNA cloning and next-generation sequencing provide into viral small interfering RNAs (vsiRNAs). Whether dsDNA virus detailed insights into vsiRNA biogenesis. In several studies in infections are controlled by the RNAi pathway remains to be insects, the polarity of the vsiRNA population deviates strongly determined. Here, we analyzed the role of RNAi in DNA virus from the highly skewed distribution of positive strand (+) over infection using Drosophila melanogaster infected with Invertebrate negative (−) viral RNAs that is generally observed in (+) RNA iridescent virus 6 (IIV-6) as a model. -

Feline—Aerosol Transmission
Feline—Aerosol Transmission foreign animal disease zoonotic disease Anthrax (Bacillus anthracis) Aspergillus spp. Bordetella bronchiseptica Calicivirus (FCV) Canine Parvovirus 2 Chlamydophila felis Coccidioides immitis Cryptococcus neoformans Feline Distemper (Feline Panleukopenia, Feline Parvovirus) Feline Infectious Peritonitis (FIP) Feline Viral Rhinotracheitis (FRV) Glanders (Burkholderia mallei) Hendra Virus Histoplasma capsulatum Melioidosis (Burkholderia pseudomallei) Nipah Virus Plague (Yersinia pestis) Pneumocystis carinii Q Fever (Coxiella burnetii) Tuberculosis (Mycobacterium spp.) www.cfsph.iastate.edu Feline—Oral Transmission foreign animal disease zoonotic disease Anthrax (Bacillus anthracis) Babesia spp. Botulism (Clostridium botulinum) Campylobacter jejuni Canine Parvovirus 2 Coccidiosis (Isospora spp.) Cryptosporidium parvum Escherichia coli (E. coli) Feline Coronavirus (FCoV) Feline Distemper (Feline Panleukopenia, Feline Parvovirus) Feline Immunodefi ciency Virus (FIV) Feline Infectious Peritonitis (FIP) Feline Leukemia Virus (FeLV) Giardia spp. Glanders (Burkholderia mallei) Helicobacter pylori Hookworms (Ancylostoma spp.) Leptospirosis (Leptospira spp.) Listeria monocytogenes Melioidosis (Burkholderia pseudomallei) Pseudorabies Roundworms (Toxocara spp.) Salmonella spp. Strongyles (Strongyloides spp.) Tapeworms (Dipylidium caninum, Echinococcus spp.) Toxoplasma gondii Tuberculosis (Mycobacterium spp.) Tularemia (Francisella tularensis) Whipworms (Trichuris campanula) www.cfsph.iastate.edu -

Can Unwanted Suburban Tortoises Rescue Native Hawaiian Plants?
CAN UNWANTED SUBURBAN TORTOISES RESCUE NATIVE HAWAIIAN PLANTS? by David A. Burney, James O. Juvik, Lida Pigott Burney, and Tomas Diagne 104 THE TORTOISE ・ 2012 hrough a series of coincidences, surplus pet tortoises in Hawaii may end up offering a partial solution to the seemingly insurmountable challenge posed by invasive plants in the Makauwahi Cave Reserve Ton Kaua`i. This has come about through a serendipitous intersection of events in Africa, the Mascarene Islands, North America, and Hawaii. The remote Hawaiian Islands were beyond the reach of naturally dispersing island tortoises, but the niches were apparently still there. Giant flightless ducks and geese evolved on these islands with tortoise-like beaks and other adaptations as terrestrial “meso-herbivores.” Dating of these remarkable fossil remains shows that they went extinct soon after the arrival of Polynesians at the beginning of the last millennium leaving the niches for large native herbivores entirely empty. Other native birds, including important plant pollinators, and some plant species have also suffered extinction in recent centuries. This trend accelerated after European settlement ecosystem services and a complex mix of often with the introduction of many invasive alien plants conflicting stakeholder interests clearly requires and the establishment of feral ungulate populations new paradigms and new tools. such as sheep, goats, cattle, and European swine, as Lacking any native mammalian herbivores, the well as other insidious invasives such as deer, rats, majority of the over 1,000 native Hawaiian plant mongoose, feral house cats, and even mosquitoes, species on the islands have been widely regarded which transmit avian malaria to a poorly resistant in the literature as singularly lacking in defensive native avifauna. -

(Geochelone Pardalis) on Farmland in the Nama-Karoo
THE STATUS AND ECOLOGY OF THE LEOPARD TORTOISE (GEOCHELONE PARDALIS) ON FARMLAND IN THE NAMA-KAROO MEGAN KAY McMASTER Submitted in fulfilment ofthe academic requirements for the degree of MASTER OF SCIENCE School ofBotany and Zoology University ofNatal Pieterrnaritzburg March 2001 Preface The experimental work described in this dissertation was carried out in the School of Botany and Zoology, University ofNatal, Pietermaritzburg, from November 1997 to March 2001, under the supervision ofDr. Colleen T. Downs. This study is the original work ofthe author and has not been submitted in any form for any diploma or degree to another university. Where use has been made ofthe work of others, it is duly acknowledged in the text. Each chapter is written in the format ofthe journal it has been submitted to. ..fj~K'. Megan Kay McMaster Pietermaritzburg March 2001 11 This thesis is dedicated to myfather, the late Eric Ralph McMaster, for his constant encouragement and beliefin me, and to my brother, the late Gregory CIifton McMaster,for always making me smile. III Abstract The Family Testudinidae (Suborder Cryptodira) is represented by 40 species worldwide and reaches its greatest diversity in southern Africa, where 14 species occur (33%), ten of which are endemic to the subcontinent. Despite the strong representation ofterrestrial tortoise species in southern Africa, and the importance ofthe Karoo as a centre of endemism ofthese tortoise species, there is a paucity ofecological information for most tortoise species in South Africa. With chelonians being protected in < 15% ofall southern African reserves it is necessary to find out more about the ecological requirements, status, population dynamics and threats faced by South African tortoise species to enable the formulation ofeffective conservation measures.