“CHILDREN” by Amelia Buttress a Dissertation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Explanation of Conflict of Interest Disclosure Parts: Part One: All
Explanation of Conflict of Interest Disclosure Parts: Part One: All Financial Involvement with a pharmaceutical or biotechnology company, a company providing clinical assessment, scientific, or medical companies doing business with or proposing to do business with ACNP over past 2 years (Jan. 2011-Present) Part Two: Income Sources & Equity of $10,000 or greater Part Three: Financial Involvement with a pharmaceutical or biotechnology company, a company providing clinical assessment, scientific, or medical products or companies doing business with or proposing to do business with ACNP which constitutes more than 5% of personal income (Jan. 2011-Present): Part Four: Grants from pharmaceutical or biotechnology company, a company providing clinical assessment, scientific, or medical products directly, or indirectly through a foundation, university, or any other organization (Jan. 2011-Present) Part Five: My primary employer is a pharmaceutical/biotech/medical device company. 2012 Program Committee Disclosures Anissa Abi-Dargham: Part 1: Pfizer; Otsuka; Takeda; Sunovion; Shire; Roche; Pierre Favre; Part 2: Pierre Favre William Carlezon: Part 1: Referring to 2010-2011: Scientific Advisory Board, Myneurolab.com; Consultant, Concert Pharmaceuticals; Consultant, Lantheus Medical Imaging; Consultant, Transcept Pharmaceuticals, (Spouse) Senior Scientist, EMD Serono; Part 2: (Spouse) Senior Scientist, EMD Serono, Part 3: (Spouse) Senior Scientist, EMD Serono Cameron Carter: Part1: GlaxoSmithKline research; Part 4: GlaxoSmithKline Karl Deisseroth: Part -

IMH Colloquium Serie
Interdisciplinary Colloquium Series for 2008 - 2009 Sponsored by the UBC INSTITUTE OF MENTAL HEALTH Sept. 10 Barbara Sahakian: Cognition in Depression and Mania WED. Professor of Clinical Neuropsychology, Dept. of Psychiatry and MR/Wellcome Trust Behavioural and Clinical Neuroscience Institute, University of Cambridge Co-sponsored by National Core for Neuroethics. 2nd talk on TH., Sept. 11, as part of its inaugural ceremonies. Oct. 2 Marten deVries: Minds, Media, & Early Education: Public Mental Health & Media Approaches for Children Under Difficult Conditions & Disaster Professor of Social Psychiatry and Head of Center for Public Mental Health, Maastricht University; Founder, International Inst. Psycho-social and Socio-ecological Research (IPSER) Co-sponsored by Div. of Child & Adolescent Psychiatry. 2nd talk Fri., Oct. 3, noon, at Children’s Hospital: the Dr. Hira Panikkar Memorial Lecture: Babies, Brains & Culture: Health & Development in the Context of Cultural Diversity; Cases from East Africa Nov. 6 Joseph Trimble: Infusing Psychology Courses with Diversity Content: Truths, Half-Truths, and Anecdotes in Cross-Cultural Psychology Professor, Center for Cross-Cultural Research, Dept. of Psychology; Director, Office of Institutional Assessment, Research, and Testing, Western Washington University Co-sponsored by the National Core for Neuroethics. 2nd talk Fri., Nov. 7, noon, Neuroethics Conference Room (Koerner S117): Responsible and Ethical Conduct of Research with Ethnocultural Populations Dec. 11 Steven Marans: Childhood Trauma: Challenges to Listening and Responding Harris Prof. of Child Psychiatry & Prof. of Psychiatry, Child Study Center, Yale University School of Medicine and Director, National Center for Children Exposed to Violence Co-sponsored by Div. of Child & Adolescent Psychiatry. 2nd talk Fri., Dec. 11, noon, at Children’s Hospital: Hands on Problem-Solving in Listening and Responding to Traumatized Children Feb. -
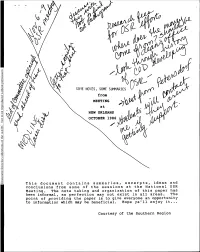
This Document Contains Summaries, Excerpts, Ideas And
permission STIE NOTES, SOME SUMMARIES without from MEETING at reproduced be NEW ORLEANS to OCTOBER 1986 Not /' AAMC the of collections the from Document This document contains summaries, excerpts, ideas and conclusions from some of the sessions at the National OSR Meeting. The note taking and organization of this paper has been informal, so perfection may not exist in all areas. The point of providing the paper is to give everyone an opportunity to information which- may be beneficial. Hope ya'll enjoy it... Courtesy of the Southern Region Informal Notes/Outline on the GeneraL Session - Friday, October 24, 1986 Dr. Leon Eisenberg, Chairman Department of Social Medicine and Health Policy Harvard Medical School Dr. Leon Eisenberg spoke following his wife, Dr. Carola Eisenberg, who presented ideas about the "Light at the End of the Medical School Tunnel." Dr. Leon Eisenberg then talked about the Trains in the tunnel. I have taken the liberty to reorganize his talk to an outline form. ,1 ia-dittAzn 7iet 71_4.4 -NottetcOlthe-coriitiuttitiorWRAiorettcalicribbftWand. ta bwAsWmorkMicin-. 19.giVOleattlm1 4SW1.- r-40%. "INC FAP 90( GALLERY 2 Prf CARY-OIRSON Ntif IN PAPERBACK. DALE :21 THE TRAINS COST OF EDUCATION MALPRACTICE CRISIS Problem Possible Solution Problem Possible Solution -1. Trend is that the edit 1. Change the time allowed for I. Less than 302 of collected I. No-fault insurance will increase repayment of loans. funds, from a law suit go to the "injured party." 2. Fees charged when trivalent 2. Applicants will come from 2. Have a surcharge (of the cases are brought to court *families with higher debt) based on Income Tax 2. -

Save Pdf (0.14
In memoriam Leon Eisenberg and the essence of Medicine I got in touch with Leon Eisenberg at the very end of were thought to be a bit odd, you were called a ‘Section his long and fulfilling professional life, or, to be precise, 8’. Army psychiatrists concerned about the stigma he got in touch with me. On December 12th, 2006 I changed the terminology from “Section 8” to “Simple received a sharp and hilarious comment on a paper I had Adult Maladjustment”. Not long after the change was written on the change of the name “mental retardation” to made, the author of the editorial was in a base camp “intellectual disability” and its relation to stigma. In a watching a film starring Jerry Lewis. He was astonished friendly tone, it distilled joy of life and “bonheur”. The to hear members of the audience call out ‘Look at the author recalled an old editorial at the American Journal of ‘Sammy’. After a moment he realized that “Sammy” Psychiatry which explained that soldiers with neuropsy- stemmed from the initial letters “S.A.M.” of “Simple chiatric problems were classified under a code known as Adult Maladjustment”. ‘Section 8’ during the Second World War. “In no time at When I reached the end of the last line I was surprised all, this classification number spread throughout the mil- to find out that the author was Leon Eisenberg. By the itary community and became a term of derision. If you time I received this email, I had admired him for many Epidemiologia e Psichiatria Sociale, 19, 1, 2010 93 Downloaded from https://www.cambridge.org/core. -

Year in Review 2018
Year in Review 2018 International Neuroethics Society Message from the President I was honored to become President of the International Neuroethics Society in November 2017 and to have a chance to build on the excellent work of my predecessors, Judy Illes, Barbara Sahakian, and Steve Hyman. I set out three goals for my two years as President: • To increase opportunities in the Society for INS members • To boost the public role of the INS in discussions, scholarly and public, of neuroethics and • To increase INS membership. I am pleased to report that we have increased the opportunities for members to take part in the Society’s activities with new committees and task forces. We have reached out to the public through, for example, our public event at the Annual Meeting on ‘My Brain Made Me Buy It? The Neuroethics of Advertising’ and our essay competition in which our members were invited to write for the lay reader. Building our membership, however, has been a little more challenging. Neuroethics is in some ways a niche field but with advances in brain research raising ever more social and ethical dilemmas, it is vital that scientists, philosophers and clinicians become involved. I am eager to get more regional INS meetings, giving opportunities for members to get together apart from the one annual meeting and to spread the word about neuroethics. We have made good progress here in 2018 with events in Oxford, UK; Milwaukee, USA; and Sydney, Australia. We have been developing new partnerships with other like-minded organizations and participating in conferences around the world. -

Howland Award Presentation to Julius B. Richmond1
003 I-3998/90/2804-04 I 1$02.00/0 PEDIATRIC RESEARCH Vol. 28, No. 4, 1990 Copyright 0 1990 International Pediatric Research Foundation, Inc. Prinled in (I.S. A. Howland Award Presentation to Julius B. Richmond1 LEON EISENBERG Chairman, Department of Social Medicine, Harvard Medical School, Boston, Massachusetts 02115 I have known Julius B. Richmond for the better part of my Julie was called to Syracuse in 1953 to be the Chair of life-the better part qualitatively as well as quantitatively; having Pediatrics. He built an outstanding academic department. A him for a friend has made my life better. There isn't time to say portrait from this era of his life is shown in Figure 2. It presents all I would like to say about Julie. Moreover, if I said it all, it to us the 1961-62 Executive Committee of the Society for might be dangerous to his health. Julie has been known to Pediatric Research. Seated are Nathan Smith, J.B.R., the Vice respond to praise with an anaphylactic reaction. The only safe President, Fred Robbins, the President that year, Clark West, thing for me to do is to dispense my encomiums in homeopathic Forrest Adams, and Edna Sobel; standing are David Gitlin, Floyd doses. Denny, Lytt Gardner, and Sid Segal. There is no more telling way to put the accomplishments of Let me now abandon dating the strata in his academic prefer- his career in perspective than by recalling what Abraham Jacobi ment to scan his research career. I haven't the time and you said in his 1889 address as the first President of this Society. -

Some Children Are Convinced, They Can't Win
DOCUMENT' rSUM P: ED 021 892 UD 004 048 By- Eisenberg Leon SOME CHILDREN ARE CONVINCED, THEY CAN'TWig Pub Date Apr 67 Note- 5p Journal Cit- Southern Education Report; v2 n8 Apr1967 EDRS Price MF-S0.25 HC-$0.28 Descripters-*ACADEMIC FAILURE CHANGING ATTITUDES*CULTURAL DIFFERENCES *DISADVANTAGED YOUTK EDUCATIONAL NEEDS ENRICHMENT EXPERIENCEFAILURE FACTORS, FAMILY LIFE. INTELLIGENCE. INTERVENTIOR LANGUAGE HANDICAPS MIDDLE CLASSPRESCHOO L PROGRAMS. *SELF CONCEPT.TEACKER ATTITUDES Identifiers-Baltimore, Maryland, PrOiect Head Start Social dass differences affect a student'sacademic achievement but do not particularly affect his intellectual potential.Adult pdgement of intelligence isbased upon observationof the student's behavior and hisperformance on standardized tests. This behavior isin turn affected by thestudent's motivation, background experience, and attitudes. Thelower-dass child comes to school with afeding of personal inadequacy and because he lacksthe language skills and generalacademic know-how necessary in formal learning situations,he inevitably fails. Thus, there is perpetuated a cycle of frustration and fadure inwhich the child's academic deficits become cumulative. The experiences of aBaltimore Head Start Proiect haveshown that for the cyde to be broken thesechildren require a continuous enrichment program with warm, varied,- active,and flexible teachers. It is important, moreover,that the worthwhile aspects of the lower-classchild's own culture not be destroyed.inthe educational process, and that the school recognizehis language and learningstyles. (LB) U.S. DEPARTMENT OF HEALTH, EDUCATION& WELFARE OFFICE OF EDUCATION THIS DOCUMENT HAS BEEN REPRODUCEDEXACTLY AS RECEIVED FROM THE POINTS OF VIEW OR OPINIONS PERSON OR ORGANIZATION ORIGINATINGIT. STATED DO NOT NECESSARILY REPRESENTOFFICIAL OFFICE Of EDUCATION POSITION OR POLICY SOME CHILDREN ARE CONVINCED THEY CAN'T WIN BY LEON EISENBERG, M.D. -

Networks of Expertise and Evidence for Public Policy Annual Report 2015 the Centre for Science and Policy in 2015
Networks of Expertise and Evidence for Public Policy Annual Report 2015 The Centre for Science and Policy in 2015 The policy challenges facing our world today demand ever-greater foresight, ingenuity and a willingness to collaborate across sectors. As this report illustrates, “Over the seven years since its launch, the Centre for Science the Centre for Science and Policy has been helping its network to navigate and Policy has pioneered new ways of bringing academia and challenges from climate resilience to new forms of healthcare; from national government together to tackle policy challenges. CSaP has security to shaping innovation in the public interest. successfully promoted long-term thinking and more robust networks of expertise and evidence for public policy. The maturity of CSaP’s unique network of academics As he moves on to chair CSaP’s Advisory Council, I and policy makers is demonstrated by the breadth would like to express my gratitude to David for his Dr Robert Doubleday and depth of our work during 2015. Our network inspirational work in founding the Centre. Executive Director Centre for Science and Policy 2015 is the year in which the Centre came of age. Having now encompasses over 200 Fellows and more than served as its founding director from 2009 to 2015, I am 1100 researchers and, during the year, we welcomed In 2016, a year set to be every bit as challenging for delighted CSaP is playing a central role in supporting the more than 2500 participants to 43 events. governments as 2015 has been, CSaP’s role in brokering links between research and policy will be University’s mission, and that the Centre is in the excellent These achievements are testimony to the vision of more important than ever. -

Psychiatry CENTENNIAL
Great Works 100 Years of Philanthropy in Service of Hopkins Psychiatry Too little, too long From the time The Johns Hopkins Hospital opened in 1889, mentally ill patients have been drawn to its care. Henry Hurd, the hospital’s first superintendent, trained in psychiatry and had headed a large asylum in Michigan. In those earliest days, psychiatric patients were seen solely as outpatients by either a part-time neurologist or psychiatrist. And teaching that specialty began then as well. By arrangement, Hopkins medical students learned current psy- chiatric care at Baltimore’s city-run Bay View Asylum, some three miles away. Yet even though psychiatry wasn’t exactly “an un- known plant in that medical Eden,” as one historian described Hopkins’ practice, it seemed to many “exotic, delicate and unattractive.” And by the cen- tury’s end, officials of both hospital and medical school were convinced that for too long they’d had too little help for some of their sickest patients. They realized that good care and meaningful study of psychiatric illness in an academic setting—that in itself a rare idea in an age of freestanding mental asylums—demanded two things: a proper, full-time psychiatry department and a clinical haven for inpa- tients. But who would bear the expense? Inspire change? The time was right for Henry Phipps. Excerpts from a letter courtesy of the Alan Mason Chesney Medical Archives of the Johns Hopkins Medical Institutions Cover: The Henry Phipps Psychiatric Clinic, dedicated April 16, 1913. Great Works The Beginning Henry Phipps’ belief in his own potential came early, when he was still in short pants. -

Leon Eisenberg Curriculum Vitae
CURRICULUM VITAE Name: Leon Eisenberg Address: 9 Clement Circle, Cambridge, MA 02138 Date of Birth: August 8, 1922 Place of Birth: Philadelphia, Pennsylvania Office Telephone: 617-432-1710 Office Fax#: 617-432-2565 HMS-E-mail: [email protected] Earned Degrees: 1944 A.B. College of University of Pennsylvania 1946 M.D. University of Pennsylvania School of Medicine Honorary Degrees: 1967 A.M. (Hon) Harvard University 1973 D.Sc. (Hon) University of Manchester, England 1991 D.Sc. (Hon) University of Massachusetts Postdoctoral Training: Internship and Residencies: 1946-1947 Rotating Intern, Mt. Sinai Hospital, New York City 1950-1952 Psychiatric Resident, Sheppard Pratt Hospital, Towson, MD. 1952-1954 Fellow in Child Psychiatry, Johns Hopkins Hospital, Baltimore, MD Military Service: 1948-1950 Captain, Medical Corps, U. S. Army Licensure and Certification: New York, Maryland, Pennsylvania, Massachusetts 1955 (Dec) Certified in Psychiatry, American Board of Psychiatry and Neurology 1960 (May) Certified in Child Psychiatry, American Board of Psychiatry and Neurology Academic Appointments: 1947-1948 Instructor in Physiology, University of Pennsylvania 1953-1955 Instructor in Psychiatry, Johns Hopkins University 1955-1958 Assistant Professor of Psychiatry, Johns Hopkins University 1 1958-1961 Associate Professor of Psychiatry, Johns Hopkins University 1961-1967 Professor of Child Psychiatry, Johns Hopkins University 1967-1993 Professor of Psychiatry, Harvard Medical School 1973-1980 Chairman, Executive Committee, Department of Psychiatry, -

Panel and Study Groups
Neuropsychopharmacology (2012) 38, S1–S78 & 2012 American College of Neuropsychopharmacology All rights reserved 0893-133X/12 www.neuropsychopharmacology.org S1 Monday, December 03, 2012 Conclusions: The signaling differences identified in this study have important implications in screening different KOR agonists and antago- nists having distinctly different ligand directed signaling properties. Mini Panel Disclosure: C. Chavkin, Part 1: Consulting for Trevena 2010-2011, 1. Renaissance in Opioid Biology: From Preclinical Concepts to Part 2: Contract with Trevena 2010-2011. Clinical Practice 1.2 The Place of Opiates in the Cortico-basal Ganglia Reward 1.1 Molecular Basis for Kappa Opioid Receptor Antagonism: Circuit Implications of Ligand-directed Signaling for the Development of Novel Antidepressants Suzanne Haber* Charles Chavkin* University of Rochester, Rochester, New York University of Washington, Seattle, Washington Background: Reward is a central component for driving incentive- based learning, appropriate responses to stimuli, and habit Background: Preclinical studies have demonstrated the role of formation. Pathology in this circuit is associated with several stress-induced dynorphin release in mediating a component of the diseases including addition. The ventral medial prefrontal cortex anxiogenic and aversive effects of stress exposure. These results (vmPFC), orbital prefrontal cortex (OFC), dorsal anterior cingulate suggest that kappa opioid receptor (KOR) antagonists or low cortex (dACC), striatum, ventral pallidum, and midbrain dopamine efficacy partial agonists may promote stress-resilience in humans neurons are at the center of the circuit associated with reward in and may potentially be useful in treating certain forms of mood general and, in particular addiction. Connectivity between these disorders exacerbated by stressful experience. In rodent models, areas forms a complex neural network that mediates different stress-induced stimulation of dynorphin release produces aversion, aspects of reward processing, that can lead to habit formation. -

June 2012 Newsletter
Newsletter “To advance education and research in the science of psychopharmacology for the public benefit” June 2012 2012 SUMMER MEETING, SUNDAY 22 TO WEDNESDAY 25 JULY, HARROGATE INTERNATIONAL CENTRE Full details of sessions are on the website, together with registration facilities http://bap.org.uk/summermeetinghome.php?meetingID=5 Highlights: The 2012 Guest Lecture, presented by Dr Nora Volkow, Director of the National Institute on Drug Abuse (NIDA) Plenary Mental Health Session, “The best treatment for treatment-resistant patients with psychiatric disorders and possibilities for developing clinical research”, including presentations from Stephen Stahl, Guy Goodwin, Gavin Malloch and Kathryn Adcock 9 invited symposia covering cutting-edge clinical and non-clinical psychopharmacology: Drugs as tools in neuropsychiatry: Ketamine; New tricks for old drugs: Opiates, addiction and beyond; Advances in understanding brain corticosteroid responses to stress: relevance to depression; Cognitive impairment in depression: A target for treatment?; New treatment strategies for targeting drug addictions – A translational perspective; Functional imaging markers for monitoring treatment: Mechanisms and efficacy; Schizophrenia Treatment: What’s wrong with it and what might work better; Epigenetics and psychiatry - current understanding and therapeutic potential; Rethinking the compulsive aspects of addiction: From bench to bedside 2 dedicated Poster Sessions Post-doc Symposium, “Neurodevelopmental models of psychiatric disease: back to the future” Satellite