District Jind (Haryana)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Question No.*759
Question No.*759 INDEX OF INFORMATION Sr. Subject Page No. No. 1 Reply of Starred question No.759 in 1 English 2 Executive Summary 2 3 Note for the pad in English 3-6 4 Reply of Starred question No.759 in 7 Hindi 5 Note for the Pad in Hindi 8-11 6 Staff Position 4 7 District Jind at a Glance 6 8 State Health Infrastructure 6 1 Construction of PHC Building *759. SHRI SUBHASH GANGOLI, M.L.A.: Will the Health Minister be pleased to state whether there is any proposal under consideration of the Government to construct a new PHC building in village Hatt of Safidon Assembly Constituency; if so, the time by which it is likely to be constructed? Anil Vij, Health Minister. Yes Sir, administrative approval amounting to Rs. 640.85 Lakhs for construction work of Primary Health Centre including residential accommodation at village Hatt has already been issued. Construction work is expected to start soon. 2 EXECUTIVE SUMMARY Primary Health Centre Hatt is working since 1992 in 200 Sq. Yards private building. 15 Kanal 19 Marla land bearing Khasra No. 73//23(2-4)99//3(8-0).8(5- 15) is transferred on lease bases for the period of 33 years in the name of Health Department vide Government letter no. SBA-4-2018/99195- 200 dated 02/11/2018. Drawings for construction of proposed Primary Health Centre at village Hatt has been approved on dated 20/06/2019. Rough Cost Estimates amounting to Rs. 640.85 Lacs for Construction of Primary Health Centre including residential accommodation at village Hatt was received from office of Engineer-in-Chief (Bldgs) Haryana, PWD (B&R) Department Chandigarh on dated 03/03/2020. -

District Disaster Management Resource Inventory, JIND
District Disaster Management Resource Inventory, JIND INDEX FIRE Department Irrigation Police Home Guard and Civil Defense PWD B&R Red Cross Roadways Power Animal Husbandary Agriculture HSIIDC Health DFSC Revenue and Disaster Management Forest Fire Department Address M.C. Narwana, Jind Nodal Officer Name: Mukes kumar Designation: Sanitory Inspector Phone: 9068670080 Sl. Name of the Type of vehicle (With Contact Contact Location/Depot No. Vehicle Capacity) Person Details CNG Diesel Petrol 1 Double Diesel Mukes kumar 9068670080 M.C.Narwana dumpher placer Sanitary inspector narwana 2 Refuse Diesel Mukes kumar 9068670080 M.C.Narwana compeactor Sanitary inspector narwana 3 Tractor trolly Diesel Mukes kumar 9068670080 M.C.Narwana Sanitary inspector narwana Fire Hydrants 2 ½ “fill 1 One In fire brigade office All fire staff Nil fire compound motor tank in 20 minutes. 4 First Aid Kits For 1 One In fire brigade office situated All fire staff can Nil about 15 at Mela Ground Mandi operate (Name persons. Narwana. and Contact Number of all fire staff is given on Annexure human resources). 5 Walkie Nil Nil Nil Nil Nil Talkie Sets 6 Vehicles Jeep Bolero 1 One In office for office use Yes, Jeep Jeep Mahindra Driver available in Year 2011. Name: Sh. Satbir Singh Con. No. 94673-54136 Fire Motor Tank 1 One In fire brigade office at Mela Yes, Driver Fire Vehicle Capacity Ground Mandi Narwana operator Motor 4000 Name: Sh. available Ltrs. Dalbir Singh in Year 1991. Cont. No. 01684-290451 Market Committee Jind Fire Moter HR-46- One Jind Driver 3200 Operator 1- Sh. Sita Ram 9416621936 2- Sh. -

Directorate of Higher Education Rotkrt F,Qlqnr Frhnrq
Government of Haryana / $fiFmqT gCif,I{ Directorate of Higher Education rotkrt f,qlqnr frhnrq ORDER The Governor of Haryana is hereby pleased to post the following Assistant Professors against vacancy/Workload, with immediate effect, in continuation of appointment order No 9/28-2019 C-1(2) dated 2L-L2-20L9. Sr Merit Name, Father name & Address Place of posting Remarks No No/Roll No (Ms/Mrs/Sh) 1 7497 Archana / Jitender Singh R/O Village- NRS GC Rohtak A,gainst Vacancy / Fairan Pana, Baliana, Tehsil Sampla, Distt. Rohtak Workload District Rohtak- 1 24416 2 4668 Sanjeet Singh / Narender Singh R/O GCW Karnal Against Vacancy / H.No. 2944, Top Floor, Sector 37-C, Workload Chandiqarh- 160036 3 L465 Anup Singh / Wazir Singh R/O H.No. GC Kheri Chopta Against Vacancy / 98, Koth Kalan, Narnaund, Distt. Distt. Hisar Workload Hisar-125039 4 3837 Prerna / Mahavir Siwach R/O H.No. GCW Bahadurgarh A,gainst'y'acancy / 133, Sardar Patel Appartment, Distt. Jhajjar VUorkloarl Pitampura, New Delhi-1 10034 5 5545 Vikas / Hukam Singh R/O Vill. Tewari, GC Barota Distt. Against Vacancy / PO- Bajana Khurd, Tehsil Ganaur, Sonipat Workload Distt. Sonipat-131101 6 3296 Naveen Kumar / Karan Singh Punia GC Matanhail Against Vacancy / R/O VPO- Khudan, Tehsil & District Distt. Jhajjar Workload Jhaiiar-124108 7 4135 Rakesh / Darshan Singh Gahlawat R/O GC Saha Distt. Against Vacancy / V.P.O. Sillakheri, Tehsil Safidon, Distt. Ambala Workload lind-1261 12 8 2857 Mahender Pal / Prem Chand R/O H.No. GCW Bhodia Against Vacancy / 357, Back Side of Old Rada Swami Khera Distt. -
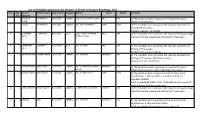
List of Ineligible Application for the Post of Driver in Haryana Roadways, Jind Sr.No
List of ineligible application for the post of Driver in Haryana Roadways, Jind Sr.No. App. Name of Father's Name Date of Birth Category Address Tehsil District REASONS No. Applicant 1 5 RAJENDER OM PARKASH 10-05-1985 GENERAL 278/3 SHEETAL PURI COLONY JIND JIND d) The Candidate does not posses the requisite Transport KUMAR Vehicle Driving Licence. 2 7 SANJEET OM PARKASH 12-06-1986 GENERAL VPO. BASS BADSHAPUR HANSI HISAR e) The Candidate does not posses the requisite experience of Driving of Three years. f) Depot Code No. not Correct. 3 8 BHUPINDER ATTAR SINGH 03-01-1985 B.C.A. 1585/7 JAWAHAR NAGAR JIND JIND e) The Candidate does not posses the requisite Heavy passenger SINGH PATIALA CHOWK Transport Vehicle experience of Driving of Three years. 4 11 KARAMVEER PALE RAM 01-07-1974 B.C.A. VPO. GULKANI JIND JIND e) The candidate does not posses the requisite experience of SINGH Driving of Three years. F) Experience columns is blank. 5 13 SANDEEP KUMAR CHANDER SINGH 10-02-1988 GENERAL VPO. KASUHAN NARWANA JIND e) The candidate does not posses the requisite experience of Driving of Three years. (Date not shown) f) Document not self attested. 6 14 SURESH KUMAR MANGE RAM 03-08-1976 GENERAL VPO. UCHANA KALAN WARD NARWANA JIND d) The Candidate does not posses the requisite Transport NO. 10 Vehicle Driving Licence . (D/L is TRV Rigd. Chasi only) 7 16 NARESH KUMAR MAHA SINGH 15-10-1981 GENERAL VPO. KHANDA KHERI HANSI HISAR b) The candidate does not posses minimum educational qualification i.e. -

BOOKSELLERS DISTRICT JIND.Xlsx
Name of Books Depot Block Name of Shop Address Mobile No. Holder Alewa SATISH BHARDWAJ SARASWATI BOOK DEPOT NEAR GGSSS NAGURAN 9416556892 Alewa RAJKUMAR SAINI RAJ BOOK DEPOT MAIN BAAZZAR NAGURAN 9466051812 Alewa PAWAN DHILLON DHILLON BOOK DEPOT CHHOTA BUS STAND NAGURAN 9466076845 Alewa ISHWAR ROHILLA ROHILLA BOOK DEPOT MAIN BAAZZAR NAGURAN 9812755007 Alewa SURENDER SHARMA SHARMA BOOK DEPOT RAJOUND ROAD ALEWA 7900070305 Alewa SURENDER KHATKAR AADITYA BOOK DEPOT RAJOUND ROAD MAIN BUS STAND ALEWA 9315172611 Alewa RAJPAL BHARAT BOOK DEPOT MAIN BAAZAR MANPHOOL PATTI ALEWA 9896916739 Alewa RAJVEER JANGRA SACHDEV BOOK DEPOT NEAR GOGA MANDIR ALEWA 7988586314 Jind Jagdish Balaji School Dress and Book Depot Patiala Chowk Jind 9996700762 , 8950651451 Jind DURGA BOOK DEPOT 8950296612 Jind EAGLE BOOK DEPOT Railway Road Jind 9034549755 Jind KOCHAR BOOK DEPOT Near SD School Jind 9416830140 Jind JAGDISH BOOK DEPOT Jind 9416178439 Jind STUDENT BOOK DEPOT Near Bus Stand Jind 9255275944 Jind ASHOKA BOOK DEPOT Near Patiala Chowk Jind 9416090334 Jind GUPTA BOOK DEPOT Jind 9416504748 Jind GULATI BOOK DEPOT Near Main Post Office Jind 9416166838 Jind AGGARWAL BOOK DEPOT Ghona road 9896607270 Jind VIKAS BOOK DEPOT Near Bus Stand Jind 9416934021 Jind Shree GOPAL PUSTAK BHANDAR GOHANA ROAD JIND 9896358125 Jind Hind Pustak Bhandar Near Hindu College Jind 8950296612 Jind Garg Pustak Bhandar Old Subji Mandi Jind 7206381005 Jind Khurana book Depot Shiv Chowk Jhanj Gate 8708547170 Jind Gopal pustak Bhandar Bhiwani road Jind 9416561948 Jind Sahu Book Depot Bhiwani road -
Village & Townwise Primary Census Abstract, Jind, Part XIII a & B, Series-6, Haryana
CENSUS OF INDIA J981 SERIES-6 HARYANA DISTRICT CENSUS HANDBOOK PARTS XIII A & B VILLAGE AND TOWN DIRECfORY VILLAGE. AND TOWNWISE PRIMARY CENSUS ABSTRACT JIND DISTRICT O. P. BHARADWAJ OF THE INDIAN ADMINISTRATIVE SERVICE Director of Census Operations Har..yana pyb}j~bed by thl( Govcrnm~nt of Haryana 1982 MOTIF The brick-built ancient temple (c 700 A.D.) at Kalayat (District Jind) is a fine specimen of architectural beauty. Local tradition traces the name Kalayat to a possible Sanskrit word Kapilayatana meaning the house of Kapil Muni. It may be identified with the Kapilatirtha of the Mahabharata. It is believed that king Shalivahana built five temples here, two of which are still existing and of the rt!maining three, only some remains are left. Out of the surviving two temples, olle has beell accepted as motif. This temple is fairly well preserved and carries intricate floral design worked out in uniform patterlls in-baked bricks.- The form suggests that this brick temple followed the Bhitargaon temple in Uttar Pradesh which goes back to about 4th-5th century A. D. It is a challenge to modern architecture that old "!onuments can withstand the rigours of time for so long. CENSUS OF INDIA-1981 ,A-CENTRAL GOVERNMENT PUBLICATIONS The publications'refating tQ- Haryana bear series No.6 and will be published as follows:- Part I- A ~Ad" mlUlstratlOu '}R eport- Enumeration . (for official use only) Part l-B Admini.stration Report-Tabulation (for official use only) Part II-A General Population Tables : 'I } combined Part U-B Primary Census Abstract: -

MOM Karnal HSPCB
FINAL ENVIRONMENTAL IMPACT ASSESSMENT REPORT& ENVIRONMENTAL MANAGEMENT PLAN For Construction of New Four/Six-lane National Highway (NH-152D) from Gangheri, district Kurukshetra to Narnaul, district Mahendergarh in the state of Haryana Project Proponent: NATIONAL HIGHWAYS AUTHORITY OF INDIA (Ministry of Road Transport &Highways, Government of India) Project Consultant SA Infrastructure Consultant Private Limited Environmental Consultant: ENVIRO INFRA SOLUTIONS PVT.LTD. (QCI Certificate No. NABET/EIA/1619/ IA 0018) January 2019 Final EIA/EMP Report for Construction of New Four Lane national Highway (NH-152D) from Gangheri, District - Kurukshetra to Narnaul, District - Mahendergarh in the state of Haryana (Length = 230 km) NATIONAL HIGHWAYS AUTHORITY OF INDIA (Ministry of Road Transport & Highways Government of India) Table of Contents Section No. Contents Page No. EXECUTIVE SUMMARY i to xi CHAPTER-1: INTRODUCTION 1.1 Project Background 1-1 1.2 Identification of Project and Project Proponent 1-1 1.3 Brief Description of the Project and its Importance to the Country 1-1 1.3.1 Salient features of the project 1-2 1.4 Scope of the EIA/EMP Study (As per TOR) 1-5 1.5 Objectives of the Consultancy Services 1-5 1.6 Policies, Legal and Administrative Framework 1-6 1.7 Structure of the Report 1-10 1.8 TOR approved by MoEF&CC and its Compliance 1-11 CHAPTER-2: PROJECT DESCRIPTION 2.1 Introduction 2-1 2.2 Description of the Project & Brief about the Project 2-1 2.2.1 Need of the Project 2-1 2.2.2 Proposed Pavement & Overlay 2-1 2.2.3 Traffic Control, -
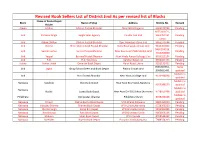
Revised Book Sellers List of District Jind As Per Revised List of Blocks Name of Books Depot Block Name of Shop Address Mobile No
Revised Book Sellers List of District Jind As per revised list of Blocks Name of Books Depot Block Name of Shop Address Mobile No. Remark Holder Alewa Dhillon Dhillon Pustak Bhandar Near GSSS Naguran 9466570744 Pending 9255103171 , Jind Parveen Singla Singla Sales Agency Gandhi Gali Jind 9466767261 Pending varun Jind Dilbag Dhillon Dhillon Pustak Bhandar Opp. Main bus stand Jind 9466570744 Pending Jind Dinesh Shree Bala Ji Book Pustak Bhandar Hansi Road paiala chowk Jind 9416365824 Pending 9466014019, Jind Suresh kumar Suresh Pustak Bhandar Near Bus stand PWD Market Jind Pending 7015200000 Jind Yaspal Beniwal Pustak Bhandar Near Hindu Kanya Colleage Jind 9034323194 Pending Jind R.D. R.D. Solutions Safidon Gate Jind 9996607744 Pending Julana Ashish Jindal Devansh Book Depot Hansi Road Julana 9253133432 Pending 9996700762 , name Jind Jagbir Balaji School Dress and Book Depot Patiala Chowk Jind 8950651451 updated Mobile no Jind Hind Pustak Bhandar Near Hindu College Jind 9416934834 updated Mobile no Narwana Sandeep Shiv Book Depot Near New Bus Stand, Narwana 9355386219 updated Mobile no Narwana Ruchir Luxmi Book Depot Near Arya Girl SSS School,Narwana 9728550296 updated Mobile no Pillukhera Ved pustak bhandar Pillukhera Mandi 8059230108 updated Narwana Dinesh Radhe Radhe Book Depot VPO-Kharal,Narwana 9807264000 Pending Narwana Vasudev Sharma Sharma Book Depot VPO-Ujhana,Narwana 9728208229 Pending Narwana Muktar Singh Balaji Biik Depot VPO-Dhamtan Sahib 9812902485 Pending Narwana Ravishwrup Ravi Book Depot VPO-Dhamtan Sahib 9466056166 Pending Narwana Mukesh Vikas Book Depot VPO-Danoda 8708544262 Pending Narwana Surender Rajesh Book Depot Punjabi Chowk,Narwana 7988374203 Pending Name of Books Depot Block Name of Shop Address Mobile No. -

Dakshin Haryana Bijli Vitran Nigam Limited
DAKSHIN HARYANA BIJLI VITRAN NIGAM LIMITED SCHEME FOR HOUSEHOLD ELECTRIFICATION DISTRICT : Jind (HARYANA) (AS PER SUPLEMENTRY DPR) DEEN DAYAL UPADHYAYA GRAM JYOTI YOJANA Table of Contents Sl.No. Format No. Name Page No. 1 A General Information 1 2 A(I) Brief Writeup 2 3 A(II) Minutes 2 4 A(III) Pert Chart 2 5 A(IV) Certificate 2 6 A(V) Basic Details of District 2 7 A(VI) Abstract : Scope of Work & Estimated Cost 4 8 A(VII) Financial Bankability 17 9 B Electrification of UE villages 19 10 B(I) Block-wise coverage of villages 20 11 B(II) Villagewise/Habitation wise coverage 21 12 B(III) Existing Habitation Wise Infrastructure 21 13 B(IV) Village Wise/Habitation Proposed Works 21 14 B(V) Existing REDB Infrastructure 21 15 B(VI) Block-Wise Substation 24 16 B(VII) Feederwise DTs 25 17 C Feeder Segregation 40 18 D Connecting unconnected RHHs 41 19 D(I) Block-wise coverage of villages 42 20 D(II) Villagewise/Habitation wise coverage 43 21 D(III) Existing Habitation Wise Infrastructure 43 22 D(IV) Village Wise/Habitation Proposed Works 43 23 D(V) Existing REDB Infrastructure 43 24 D(VI) Block-Wise Substation 46 25 D(VII) Eligibility for Augmentation of Existing 33/11 KV Substations 47 26 D(VIII) Feederwise DTs 57 27 E Metering 72 28 E(I) DTR Metering 73 29 E(II) Consumer Metering 193 30 E(III) Shifting of Meters 196 31 E(IV) Feeder Metering 197 32 F System Strengthening and Augmentation 198 33 F(I) Block-Wise Substation 199 34 F(II) EHV Substation Feeding the District 200 35 F(III) Districtwise Details of Existing 66 KV or 33 KV Lines 222 36 -

S/D Jind Ved Nagar 4.1.2013 1 Jain Nagar 5.1.2013 2 Saini Mohalla 7..1 2013 3 Aprari Mohala 9.1.2013 4 New Market 10.1.2013 5 Punjabi Bazar 11.1.2013 6 Sh
FORMAT-I Tour programme of Field Officers/Officials to Villages/Wards/Sectors for the month of January 2013 Name of Circle: - Jind Sr. No. Name of Officer/Official Designation Name of S/Divn Villages/Wards/ Sectors to be Date of visit Time of visit Mobile No. of visiting [SE/XEN/SDO/JE's] visited officer /official (OP) S/D Jind Ved Nagar 4.1.2013 1 Jain Nagar 5.1.2013 2 Saini Mohalla 7..1 2013 3 Aprari Mohala 9.1.2013 4 New Market 10.1.2013 5 Punjabi Bazar 11.1.2013 6 Sh. K.S.Redhu JE (OP) S/D Jind 10:30 AM 9355855766 Palika Bazar 12.1.2013 7 Hari Nagar 14.1.2013 8 Krishana Colony 15.1.2013 9 Om Nagar 16.1.2013 10 Hanuman Nagar 17.1.2013 11 Sh. Dinesh Kumar, Sh. Kath Mandi 18.1.2013 9315802292, 12 SDO, JE (OP) S/D Jind K.S.Redhu 9355855766 Shyam Nagar 19.1.2013 13 Bajran Mohalla 21.1.2013 14 Gandhi Gali 22.1.2013 15 Sh. K.S.Redhu JE (OP) S/D Jind 10:30 AM 9355855766 Vidya Peeth Marg 23.1.2013 16 Holi Mohalla , Arya Sasmaj Road 24.1.2013 17 Sh. Dinesh Kumar, Sh. Tanga Chowk 25.1.2013 9315802292, 18 SDO, JE (OP) S/D Jind K.S.Redhu 9355855766 Lohara Gati 26.1.2013 19 Main Bazar 28.1.2013 20 Roop Nagar 29.1.2013 21 10:30 AM Saini Old Mohalla Old 30.1.2013 22 Satina Mohalla 31.1.2013 23 Sh. -

CSP 129 Average Customers Serviced by CSP 891 Block Permanent No of Block Coordinator Operator Village and Mc No of Village No
Key Contact Details of the State Sr no. District Name Designation Looking After Contact no. Escalation Level 1 Karnal Surdershan Kumar District Coordinator Karnal 8930900842 1 2 Kaithal Satvik Garg District Coordinator Yamuna Nagar 8930900837 1 3 Kuruksherta Parveen Bansal District Coordinator Panchkula 9050008472 1 4 Panipat Ishwar Singh District Coordinator Panipat 8930900843 1 5 Jind Dharamvir Thakur District Coordinator Jind 8930900804 1 6 sonipat Lokesh Kumar District Coordinator Sonipat 9991701281 1 7 Rewari Vikash Verma District Coordinator Rewari 8930900823 1 8 Mahendergarh Hariom Yadav District Coordinator Mahendergarh 9050008468 1 9 Fatehabad Rajnish Srivastava District Coordinator Fatehabad 9850008460 1 10 Sirsa Rajnish Srivastava District Coordinator Sirsa 9850008460 1 11 Faridabad Sanjay Jha District Coordinator Faridabad 8860996602 1 12 Palwal Chandra Jha District Coordinator Palwal 8930900801 1 13 Bhiwani Vinay Gulia District Coordinator Bhiwani 8053096469, 981819033 1 14 Mewat Jitendar Deshwal District Coordinator Mewat 8930900808 1 15 Panchkula Parveen bansal District Coordinator Panchkula 9050008472 1 16 Ambala Parveen Bansal District Coordinator Ambala 9050008472 1 Faridabad, Palwal, Mewat, Mahendergarh, Rewari, 9050008464, 999804859 17 Faridabad Neeraj Lekhwar Cluster Head Karnal, Kaithal 2 Panipat, Bhiwani, Sonipat, 9850008460 18 Panipat Rajnish Srivastava Cluster Head Jind, Fatehabad, Sirsa 2 19 Bhiwani Vinay Gulia Cluster Head Sirsa, Fatehabad, Bhiwani 8053096469, 981819033 2 Ambala, Kurushetra, 9050008472 20 Kurushetra Parveen Bansal Cluster Head Kaithal, Panchkula 2 21 Karnal Anand Kumar tiwari State Head All districts 9050008465 3 District - Jind Total No of CSP 129 Average Customers serviced by CSP 891 Block Permanent No of Block Coordinator Operator Village And Mc No of village No. of customers District Block Coordinator Enrollment Point Villages Name of Disbursement CSP Beneficiaries Schedule Name Name Code covered serviced by CSP Contact no. -

Final Cluster List
FINAL CLUSTER LIST Sr District Block Cluster Cluster Head School Name UDISECode School Name Distance Head From School CRC in Code KM 1 JIND ALEWA 6090500504 GHS BADHANA 6090500503 GGMS BADHANA 0 2 JIND ALEWA 6090500504 GHS BADHANA 6090500502 GGPS BADHANA 0 3 JIND ALEWA 6090500504 GHS BADHANA 6090500504 GHS BADHANA 0 4 JIND ALEWA 6090500504 GHS BADHANA 6090503302 GHS KUCHRANA KALAN 8 5 JIND ALEWA 6090500504 GHS BADHANA 6090503403 GMS KUCHRANA KHURD 5 6 JIND ALEWA 6090500504 GHS BADHANA 6090500501 GPS BADHANA 0 7 JIND ALEWA 6090500504 GHS BADHANA 6090503301 GPS KUCHRANA KALAN 8 8 JIND ALEWA 6090500504 GHS BADHANA 6090503401 GPS KUCHRANA KHURD 5 9 JIND ALEWA 6090501503 GHS DHILLOWAL 6090501502 GGPS DHILLOWAL 0 10 JIND ALEWA 6090501503 GHS DHILLOWAL 6090501503 GHS DHILLOWAL 0 11 JIND ALEWA 6090501503 GHS DHILLOWAL 6090502802 GHS KHANDA 10 12 JIND ALEWA 6090501503 GHS DHILLOWAL 6090501501 GPS DHILLOWAL 0 13 JIND ALEWA 6090501503 GHS DHILLOWAL 6090501801 GPS GOHIAN 10 14 JIND ALEWA 6090501503 GHS DHILLOWAL 6090502801 GPS KHANDA 10 15 JIND ALEWA 6090501503 GHS DHILLOWAL 6090504001 GPS RAICHAND WALA 5 16 JIND ALEWA 6090501503 GHS DHILLOWAL 6090504004 GSSS RAI CHAND WALA 5 17 JIND ALEWA 6090501503 GHS DHILLOWAL 6090501504 KGBV DHILLOWAL 0 18 JIND ALEWA 6090500304 GSSS ALEWA 6090500302 GGPS ALEWA KHERA 0 19 JIND ALEWA 6090500304 GSSS ALEWA 6090500307 GGSSS ALEWA 0 20 JIND ALEWA 6090500304 GSSS ALEWA 6090500902 GHS BIGHANA 15 21 JIND ALEWA 6090500304 GSSS ALEWA 6090501702 GHS DURANA 8 22 JIND ALEWA 6090500304 GSSS ALEWA 6090501701 GPS DURANA 8 23