Penicillamine/Pentetic Acid 1459
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Safety Data Sheet
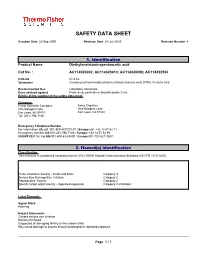
SAFETY DATA SHEET Creation Date 22-Sep-2009 Revision Date 24-Jun-2020 Revision Number 4 1. Identification Product Name Diethylenetriaminepentaacetic acid Cat No. : AC114320000; AC114320010; AC114320050; AC114322500 CAS-No 67-43-6 Synonyms (Carboxymethylimino)bis(ethylenenitrilo)tetraacetic acid; DTPA; Pentetic acid Recommended Use Laboratory chemicals. Uses advised against Food, drug, pesticide or biocidal product use. Details of the supplier of the safety data sheet Company Fisher Scientific Company Acros Organics One Reagent Lane One Reagent Lane Fair Lawn, NJ 07410 Fair Lawn, NJ 07410 Tel: (201) 796-7100 Emergency Telephone Number For information US call: 001-800-ACROS-01 / Europe call: +32 14 57 52 11 Emergency Number US:001-201-796-7100 / Europe: +32 14 57 52 99 CHEMTREC Tel. No.US:001-800-424-9300 / Europe:001-703-527-3887 2. Hazard(s) identification Classification This chemical is considered hazardous by the 2012 OSHA Hazard Communication Standard (29 CFR 1910.1200) Acute Inhalation Toxicity - Dusts and Mists Category 4 Serious Eye Damage/Eye Irritation Category 2 Reproductive Toxicity Category 2 Specific target organ toxicity - (repeated exposure) Category 2 Inhalation Label Elements Signal Word Warning Hazard Statements Causes serious eye irritation Harmful if inhaled Suspected of damaging fertility or the unborn child May cause damage to organs through prolonged or repeated exposure ______________________________________________________________________________________________ Page 1 / 7 Diethylenetriaminepentaacetic acid Revision -

Nitric Oxide Modulation of Interleukin-1Я-Evoked Intracellular
The Journal of Neuroscience, December 15, 2000, 20(24):8980–8986 Nitric Oxide Modulation of Interleukin-1-Evoked Intracellular Ca2؉ Release in Human Astrocytoma U-373 MG Cells and Brain Striatal Slices Antonella Meini,1 Alberto Benocci,1 Maria Frosini,1 Gianpietro Sgaragli,1 Gianpaolo Pessina,2 Carlo Aldinucci,2 Gise` le Tchuisseu Youmbi,1 and Mitri Palmi1 1Istituto di Scienze Farmacologiche and 2Istituto di Fisiologia, Universita` di Siena, 53100 Siena, Italy Intracellular Ca 2ϩ mobilization and release into mammal CSF Ca 2ϩ release induced by 2.5 but not 10 ng/ml IL-1. Ruthenium plays a fundamental role in the etiogenesis of fever induced by red (50 M) and, to a lesser extent, heparin (3 mg/ml) antagonized the proinflammatory cytokine interleukin-1 (IL-1) and other IL-1-induced Ca 2ϩ release, and both compounds administered pyrogens. The source and mechanism of IL-1-induced intracel- together completely abolished this response. Similar results were lular Ca 2ϩ mobilization was investigated using two experimental obtained in human astrocytoma cells in which IL-1 elicited a models. IL-1 (10 ng/ml) treatment of rat striatal slices preloaded delayed (30 min) increase in intracellular Ca 2ϩ concentration 45 2ϩ 2ϩ Ϯ with Ca elicited a delayed (30 min) and sustained increase ([Ca ]i ) (402 71.2% of baseline), which was abolished by 1 45 2ϩ (125–150%) in spontaneous Ca release that was potentiated mML-NAME. These data indicate that the NO/cGMP-signaling by L-arginine (300 M) and counteracted by N--nitro-L-arginine pathway is part of the intracellular mechanism transducing IL- 2ϩ methyl ester (L-NAME) (1 and 3 mM). -

(12) United States Patent (10) Patent No.: US 8,158,152 B2 Palepu (45) Date of Patent: Apr
US008158152B2 (12) United States Patent (10) Patent No.: US 8,158,152 B2 Palepu (45) Date of Patent: Apr. 17, 2012 (54) LYOPHILIZATION PROCESS AND 6,884,422 B1 4/2005 Liu et al. PRODUCTS OBTANED THEREBY 6,900, 184 B2 5/2005 Cohen et al. 2002fOO 10357 A1 1/2002 Stogniew etal. 2002/009 1270 A1 7, 2002 Wu et al. (75) Inventor: Nageswara R. Palepu. Mill Creek, WA 2002/0143038 A1 10/2002 Bandyopadhyay et al. (US) 2002fO155097 A1 10, 2002 Te 2003, OO68416 A1 4/2003 Burgess et al. 2003/0077321 A1 4/2003 Kiel et al. (73) Assignee: SciDose LLC, Amherst, MA (US) 2003, OO82236 A1 5/2003 Mathiowitz et al. 2003/0096378 A1 5/2003 Qiu et al. (*) Notice: Subject to any disclaimer, the term of this 2003/OO96797 A1 5/2003 Stogniew et al. patent is extended or adjusted under 35 2003.01.1331.6 A1 6/2003 Kaisheva et al. U.S.C. 154(b) by 1560 days. 2003. O191157 A1 10, 2003 Doen 2003/0202978 A1 10, 2003 Maa et al. 2003/0211042 A1 11/2003 Evans (21) Appl. No.: 11/282,507 2003/0229027 A1 12/2003 Eissens et al. 2004.0005351 A1 1/2004 Kwon (22) Filed: Nov. 18, 2005 2004/0042971 A1 3/2004 Truong-Le et al. 2004/0042972 A1 3/2004 Truong-Le et al. (65) Prior Publication Data 2004.0043042 A1 3/2004 Johnson et al. 2004/OO57927 A1 3/2004 Warne et al. US 2007/O116729 A1 May 24, 2007 2004, OO63792 A1 4/2004 Khera et al. -

FDA Listing of Established Pharmacologic Class Text Phrases January 2021
FDA Listing of Established Pharmacologic Class Text Phrases January 2021 FDA EPC Text Phrase PLR regulations require that the following statement is included in the Highlights Indications and Usage heading if a drug is a member of an EPC [see 21 CFR 201.57(a)(6)]: “(Drug) is a (FDA EPC Text Phrase) indicated for Active Moiety Name [indication(s)].” For each listed active moiety, the associated FDA EPC text phrase is included in this document. For more information about how FDA determines the EPC Text Phrase, see the 2009 "Determining EPC for Use in the Highlights" guidance and 2013 "Determining EPC for Use in the Highlights" MAPP 7400.13. -

(NSP15) Inhibitors: Repurposing FDA-Approved Drugs
Potential SARS-CoV-2 Nonstructural Protein 15 (NSP15) Inhibitors: Repurposing FDA-Approved Drugs Jason Y Tang1, Igor F. Tsigelny2-4*, Jerry P. Greenberg2, Mark A. Miller2, Valentina L. Kouznetsova2,4 1REHS program, San Diego Supercomputer Center, UC San Diego, La Jolla, California, USA 2San Diego Supercomputer Center, UC San Diego, La Jolla, California., USA 3Department of Neurosciences, UC San Diego, La Jolla, California, USA 4BiAna. San Diego, California, USA *Corresponding author: UC San Diego, 9500 Gilman Drive, La Jolla, CA 92093-0505, USA Email: [email protected] (Orcid ID: 0000-0002-7155-8947) Running Head: NSP-15 inhibitors as COVID-19 Drugs Word Count: 3743 1 Abstract Purpose: Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has caused millions of deaths worldwide, pushing the urgent need for an efficient treatment. Nonstructural protein 15 (NSP15) is a promising target due to its importance for SARS-CoV-2’s evasion of the host’s innate immune response. Methods: Using the crystal structure of SARS-CoV-2 NSP15 endoribonuclease, we developed a pharmacophore model of the functional centers in the NSP15 inhibitor’s binding pocket. With this model, we conducted data mining of the conformational database of FDA-approved drugs. The conformations of these compounds underwent 3D fingerprint similarity clustering, and possible conformers were docked to the NSP15 binding pocket. We also simulated docking of random compounds to the NSP15 binding pocket for comparison. Results: This search identified 170 compounds as potential inhibitors of SARS-CoV-2 NSP15. The mean free energy of docking for the group of potential inhibitors were significantly lower than for the group of random compounds. -

Analytical Methods for the Detection and Quantification of Adcs in Biological Matrices
pharmaceuticals Review Analytical Methods for the Detection and Quantification of ADCs in Biological Matrices Héloïse Cahuzac and Laurent Devel * Département Médicaments et Technologies pour la Santé (MTS), CEA, INRAE, SIMoS, Université Paris-Saclay, 91191 Gif-sur-Yvette, France; [email protected] * Correspondence: [email protected]; Tel.: +33-1-69-08-95-65 Received: 8 October 2020; Accepted: 11 December 2020; Published: 14 December 2020 Abstract: Understanding pharmacokinetics and biodistribution of antibody–drug conjugates (ADCs) is a one of the critical steps enabling their successful development and optimization. Their complex structure combining large and small molecule characteristics brought out multiple bioanalytical methods to decipher the behavior and fate of both components in vivo. In this respect, these methods must provide insights into different key elements including half-life and blood stability of the construct, premature release of the drug, whole-body biodistribution, and amount of the drug accumulated within the targeted pathological tissues, all of them being directly related to efficacy and safety of the ADC. In this review, we will focus on the main strategies enabling to quantify and characterize ADCs in biological matrices and discuss their associated technical challenges and current limitations. Keywords: antibody–drug conjugates; pharmacokinetics and biodistribution; liquid chromatography coupled to mass spectrometry; ligand-binding assays; in vivo imaging; ex vivo autoradiography 1. Introduction Antibody–drug conjugates (ADCs) consist of a small-molecule drug (payload) covalently bound to a monoclonal antibody via a chemical linker. By merging the specific binding properties of antibodies to the potency of small molecules, ADCs are designed to selectively deliver cell-killing agents to targeted pathogenic tissues, while limiting systemic toxicity. -
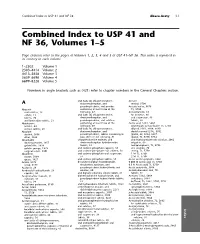
Combined Index to USP 41 and NF 36, Volumes 1–5
Combined Index to USP 41 and NF 36 Abaca-Acety I-1 Combined Index to USP 41 and NF 36, Volumes 1–5 Page citations refer to the pages of Volumes 1, 2, 3, 4 and 5 of USP 41±NF 36. This index is repeated in its entirety in each volume. 1–2302 Volume 1 2303–4414 Volume 2 4415–5658 Volume 3 5659–6698 Volume 4 6699–8228 Volume 5 Numbers in angle brackets such as 〈421〉 refer to chapter numbers in the General Chapters section. and (salts of) chlorpheniramine, Acetate A dextromethorphan, and methyl, 5706 pseudoephedrine, oral powder Acetate buffer, 5676 Abacavir containing at least three of the TS, 5750 oral solution, 19 following, 47 Acetazolamide, 65 sulfate, 23 and (salts of) chlorpheniramine, for injection, 66 tablets, 20 dextromethorphan, and oral suspension, 68 and lamivudine tablets, 21 pseudoephedrine, oral solution tablets, 68 Abiraterone containing at least three of the Acetic acid, 5181, 5664 acetate, 24 following, 49 ammonium acetate buffer TS, 5750 acetate tablets, 26 and (salts of) chlorpheniramine, diluted, 5181, 5664, 5690 Absolute dextromethorphan, and double-normal (2 N), 5762 alcohol, 5666 pseudoephedrine, tablets containing at glacial, 69, 5664, 5697 ether, 5664 least three of the following, 51 glacial, TS, 5750, 5754 Absorbable chlorpheniramine maleate, and and hydrocortisone otic solution, 2062 dusting powder, 1457 dextromethorphan hydrobromide irrigation, 69 gelatin film, 1929 tablets, 53 metaphosphoric, TS, 5756 gelatin sponge, 1929 and codeine phosphate capsules, 55 otic solution, 70 surgical suture, 3901 and codeine phosphate -

Combatting Wound Biofilm and Recalcitrance with a Novel Anti- Biofilm Hydrofiber Wound Dressing
Accepted Manuscript Title: Combatting Wound Biofilm and Recalcitrance with a Novel Anti-biofilm Hydrofiber Wound Dressing Author: Philip G. Bowler David Parsons PII: S2213-9095(16)30020-9 DOI: http://dx.doi.org/doi:10.1016/j.wndm.2016.05.005 Reference: WNDM 79 To appear in: Received date: 6-5-2016 Accepted date: 9-5-2016 Please cite this article as: Philip G.Bowler, David Parsons, Combatting Wound Biofilm and Recalcitrance with a Novel Anti-biofilm Hydrofiber Wound Dressing, Wound Medicine http://dx.doi.org/10.1016/j.wndm.2016.05.005 This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain. Title: Combatting Wound Biofilm and Recalcitrance with a Novel Anti- biofilm Hydrofiber Wound Dressing Authors: Philip G Bowler, MPhil David Parsons, PhD Address: ConvaTec GDC, First Avenue, Deeside Industrial Park, Deeside, Flintshire, UK, CH5 2NU Email/Correspondence: [email protected] 1 ABSTRACT Background: Biofilm is an impediment to wound healing as a consequence of its proven ability to impair epithelialization, granulation tissue formation and normal inflammatory processes, as well as protecting wound pathogens from antibiotics and antiseptics. With this in mind, a project was initiated to develop a combined anti-biofilm/antimicrobial technology that could be incorporated into a wound dressing to maximize effectiveness against wound pathogens existing in their predominant biofilm form. -

Edta Ethylene Diamine Tetra Acetic Acid
EDTA GENERAL Chelation is a chemical combination with a metal in complexes in which the metal is part of a ring. Organic ligand is called chelator or chelating agent, the chelate is a metal complex. The larger number of ring closures to a metal atom is the more stable the compound. This phenomenon is called the chelate effect; it is generally attributed to an increase in the thermodynamic quantity called entropy that accompanies chelation. The stability of a chelate is also related to the number of atoms in the chelate ring. Monodentate ligands which have one coordinating atom like H 2O or NH 3 are easily broken apart by other chemical processes, whereas polydentate chelators, donating multiple binds to metal ion, provide more stable complexes. Chlorophyll, green plant pigment, is a chelate that consists of a central magnesium atom joined with four complex chelating agent (pyrrole ring). The molecular structure of the chlorophyll is similar to that of the heme bound to proteins to form hemoglobin, except that the latter contains iron(II) ion in the center of the porphyrin. Heme is an iron chelate. Chelation is applied in metal complex chemistry, organic and inorganic chemistry, biochemistry, and environment protection. It is used in chemotherapeutic treatments for metal poisoning. Chelating agents offers a wide range of sequestrants to control metal ions in aqueous systems. By forming stable water soluble complexes with multivalent metal ions, chelating agents prevent undesired interaction by blocking normal reactivity of metal ions. EDTA (ethylenediamine tetraacetate) is a good example of common chelating agent which have nitrogen atoms and short chain carboxylic groups. -

Hemumurta Unhau
HEMUMURTAUS 20170365883A1UNHAU ( 19) United States (12 ) Patent Application Publication ( 10) Pub . No. : US 2017/ 0365883 A1 Luski et al. ( 43) Pub . Date : Dec . 21 , 2017 ( 54 ) LITHIUM ION BATTERY ( 52 ) U . S . CI. CPC .. HOIM 10 / 4235 ( 2013 .01 ) ; HOIM 10 /0525 (71 ) Applicants :GM GLOBAL TECHNOLOGY ( 2013 .01 ) ; HOIM 2 / 1653 ( 2013 .01 ) ; HOIM OPERATIONS LLC , DETROIT , MI 2 / 166 (2013 .01 ) (US ) ; Bar - Ilan University , Ramat Gan ( IL ) ( 57 ) ABSTRACT (72 ) Inventors : Shalom Luski, Rehovot ( IL ) ; Doron Aurbach , Bnei Brak ( IL ) ; Bob R . A lithium ion battery includes a positive and a negative Powell, JR ., Birmingham , MI (US ) ; Ion electrode , and a nanoporous or microporous polymer sepa C . Halalay , Grosse Pointe Park , MI rator soaked in electrolyte solution and disposed between the (US ) ; Timothy J . Fuller, Pittsford , NY electrodes . At least two different chelating agents are (US ) ; Anjan Banerjee , West Bengal included and selected to complex with : i ) two or more State ( IN ) ; Baruch Ziv , Ramat -Gan different transition metal ions ; ii ) a transition metal ion in ( IL ) ; Yuliya Shilina , Bat Yam ( IL ) two or more different oxidation states ; or iii ) both i ) and ii ) . The at least two different selected chelating agents are to (21 ) Appl. No. : 15 / 186 , 526 complex with transition metal ions in a manner sufficient to (22 ) Filed : Jun . 19 , 2016 not affect movement of lithium ions across the separator during operation of the battery . The chelating agents are : Publication Classification dissolved or dispersed in the electrolyte solution ; grafted (51 ) Int . Cl. onto the polymer of the separator ; attached to the binder HOIM 10 /42 ( 2006 . -

Overview of Role of Radionuclides in Scanning the Brain in Health and Disease
Journal of Neurology & Stroke Overview of Role of Radionuclides in Scanning the Brain in Health and Disease Preface Review Article revolutionary technique called Computerised Axial Tomography Volume 6 Issue 4 - 2017 (CAT)When Scan GN in Hounsfield1972, it was announced thought that the nuclear development imaging ofwill a get relegated to the pages of history. Since then the world has witnessed the development of MRI, spiral CT, 3-D reconstruction Professor and Head of Anatomical Sciences, All Saints etc. Though the role of nuclear imaging has decreased with the University, St. Vincent and the Grenadines advent of these techniques, it still occupies a niche for itself which cannot be usurped. In this article radio-nuclide scans of the brain *Corresponding author: Sanjoy Sanyal, Professor and Head of Anatomical Sciences, Neuroscientist and Surgeon, Austin Pond Drive, Cary, North Carolina, NC 27519, USA, Email: Isotopeswill be briefly and reviewed. Imaging Received: October 14, 2016 | Published: April 17, 2017 Though radio-isotopes 73As (Arsenic), 197Hg and 203Hg (Mercury) have been used for brain scanning, Technitium pertechnetate (99mTc-pertechnetate) is most commonly used. Following intravenous (IV) injection its gamma ray emissions are Table 1: Radio-isotopes in brain scan. captured by a gamma camera. The scanned image may be seen on a digital screen or on a developed photographic plate, where 99mTcO (pertechnetate) 4 All space occupying lesions increased or decreased gamma emissions correspond to areas of 99mTc-DTPA (pentetate) ‘hot’ -

Dissolvine® DZ-P Pentetic Acid - Meets the Chemical Specification Requirements of the USP
Product Data Leaflet Dissolvine® DZ-P Pentetic Acid - meets the chemical specification requirements of the USP Chemical Name Diethylenetriaminepentaacetic acid Chemical formula DTPA-H5 Structure O O HO C CH 2 CH2 C OH N CH CH CH 2 CH2 N 2 2 N HO C CH 2 CH2 CH2 C OH O C-OH O O Mol. Weight 393.4 CAS Number 67-43-6 Specifications Checkpoint Specification Units Method Identification (IR test) Passes test USP Assay as DTPA-H5 98.0 - 100.5 % USP Residue on ignition 0.2 max % USP Heavy metals as Pb 0.005 max % USP Iron 0.01 max % USP Nitrilotriacetic acid < 0.1 % USP Main Characteristics Dissolvine® DZ-P is a high purity sequestering agent, forming very stable water soluble complexes with polyvalent metal ions in a wide pH range. Solubility in water : approx. 5 g/l water (20°C) : approx. 13 g/l water (50°C) : approx. 48 g/l water (80°C) Addition of alkali hydroxide changes solubility considerably Bulk density untapped (poured) : approx. 500-700 kg/m3 Bulk density tapped : approx. 850-1050 kg/m3 Sequestering values for Dissolvine® DZ-P are approximately (theoretical calculated figures – mg metal ion / g DZ-P): ® Metal ion pH range Dissolvine DZ calcium 6 - 14 100 copper 2 - 14 160 ferric 1 - 11 140 magnesium 6 - 12 60 manganese 4 - 13 140 zinc 2 - 13 165 FPD 1201-07-4, Feb-2012 / Update 1 The information presented herein is true and accurate to the best of our knowledge, but without any guarantee unless explicitly given.