Analytical Methods for the Detection and Quantification of Adcs in Biological Matrices
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Safety Data Sheet
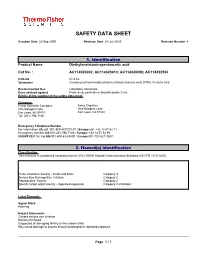
SAFETY DATA SHEET Creation Date 22-Sep-2009 Revision Date 24-Jun-2020 Revision Number 4 1. Identification Product Name Diethylenetriaminepentaacetic acid Cat No. : AC114320000; AC114320010; AC114320050; AC114322500 CAS-No 67-43-6 Synonyms (Carboxymethylimino)bis(ethylenenitrilo)tetraacetic acid; DTPA; Pentetic acid Recommended Use Laboratory chemicals. Uses advised against Food, drug, pesticide or biocidal product use. Details of the supplier of the safety data sheet Company Fisher Scientific Company Acros Organics One Reagent Lane One Reagent Lane Fair Lawn, NJ 07410 Fair Lawn, NJ 07410 Tel: (201) 796-7100 Emergency Telephone Number For information US call: 001-800-ACROS-01 / Europe call: +32 14 57 52 11 Emergency Number US:001-201-796-7100 / Europe: +32 14 57 52 99 CHEMTREC Tel. No.US:001-800-424-9300 / Europe:001-703-527-3887 2. Hazard(s) identification Classification This chemical is considered hazardous by the 2012 OSHA Hazard Communication Standard (29 CFR 1910.1200) Acute Inhalation Toxicity - Dusts and Mists Category 4 Serious Eye Damage/Eye Irritation Category 2 Reproductive Toxicity Category 2 Specific target organ toxicity - (repeated exposure) Category 2 Inhalation Label Elements Signal Word Warning Hazard Statements Causes serious eye irritation Harmful if inhaled Suspected of damaging fertility or the unborn child May cause damage to organs through prolonged or repeated exposure ______________________________________________________________________________________________ Page 1 / 7 Diethylenetriaminepentaacetic acid Revision -

Affinity-Based, Biophysical Methods to Detect and Analyze Ligand Binding
Journal of Structural Biology 172 (2010) 142–157 Contents lists available at ScienceDirect Journal of Structural Biology journal homepage: www.elsevier.com/locate/yjsbi Affinity-based, biophysical methods to detect and analyze ligand binding to recombinant proteins: Matching high information content with high throughput Geoff A. Holdgate a, Malcolm Anderson a, Fredrik Edfeldt b, Stefan Geschwindner b,* a Lead Generation Sciences, AstraZeneca R&D Alderley Park, 50F49 Mereside, Alderley Park, United Kingdom b Lead Generation Sciences, AstraZeneca R&D Mölndal, S-43183 Mölndal, Sweden article info abstract Article history: Affinity-based technologies have become impactful tools to detect, monitor and characterize molecular Available online 4 July 2010 interactions using recombinant target proteins. This can aid the understanding of biological function by revealing mechanistic details, and even more importantly, enables the identification of new improved Keywords: ligands that can modulate the biological activity of those targets in a desired fashion. The selection of the Affinity appropriate technology is a key step in that process, as each one of the currently available technologies Thermodynamic offers a characteristic type of biophysical information about the ligand-binding event. Alongside the Interaction indisputable advantages of each of those technologies they naturally display diverse restrictions that Fragment are quite frequently related to the target system to be studied but also to the affinity, solubility and Ligand Screening molecular size of the ligands. This paper discusses some of the theoretical and experimental aspects of the most common affinity-based methods, what type of information can be gained from each one of those approaches, and what requirements as well as limitations are expected from working with recombinant proteins on those platforms and how those can be optimally addressed. -

Recommendations for the Bioanalytical Method Validation Of
Pharmaceutical Research, Vol. 20, No. 11, November 2003 (© 2003) Research Paper Recommendations for the studies was held more than a decade ago in Crystal City, VA (1,2). The proceedings and recommendations of that meeting Bioanalytical Method Validation of essentially became a de facto guideline for bioanalytical meth- Ligand-binding Assays to Support ods validation within the pharmaceutical industry. The con- ference addressed validation of bioanalytical methods in gen- Pharmacokinetic Assessments eral, but acknowledged differences between chromatographic of Macromolecules and nonchromatographic assays, including immunoassays and microbiological-based methods. After the original Crystal City conference, bioanalytical methods validation was ad- dressed subsequently several times at meetings and in publi- Binodh DeSilva,1 Wendell Smith,2 Russell Weiner,3 cations (3–6). Most emphasis to date has been on validation of Marian Kelley,4,11 JoMarie Smolec,5 Ben Lee,6 bioanalytical methods for conventional small molecular Masood Khan,7 Richard Tacey,8 Howard Hill,9 and weight drugs, principally due to the rapid growth during the Abbie Celniker10 1990s in the use of hyphenated mass-spectrometry as a rou- tine analytical tool. Because of the evolution in divergent analytical tech- Received July 2, 2003; accepted July 30, 2003 nologies for conventional small molecules and macromol- Purpose. With this publication a subcommittee of the AAPS Ligand ecules and the growth in the interest of macromolecular Binding Assay Bioanalytical Focus Group (LBABFG) makes recom- therapeutics, the topic of bioanalytical methods validation mendations for the development, validation, and implementation of was revisited in 2000 in 2 meetings, one focused on small ligand binding assays (LBAs) that are intended to support pharma- molecule analytes (7) and the other focused on macromol- cokinetic and toxicokinetic assessments of macromolecules. -

Simple, Rapid Ligand-Binding Assay Using Immobilized Cellular Membranes
Simple, Rapid Ligand-Binding Assay Using Immobilized Cellular Membranes Paula Denney Eason, Renée C. Benson, Jenny T. Ly, Rachel A. Saxer, James L. Wilbur, George B. Sigal, Eli N. Glezer, Hans A. Biebuyck, Jacob N. Wohlstadter, and Robert M. Umek TM TM A division of Meso Scale Diagnostics,TM LLC. Simple, Rapid Ligand-Binding Assay Using Immobilized Cellular Membranes Abstract This poster presents a robust, receptor-ligand binding assay based upon a novel assay platform developed by Meso Scale DiscoveryTM (MSDTM). MSD’s platform combines array technologies and electrochemiluminescence detection to achieve ultra-fast, highly sensitive assays in a homogeneous format. Cellular membranes containing the EGF receptor were passively adsorbed to MSD proprietary coated electrodes embedded in multi-well plates. Binding of EGF to the EGF receptor was detected by inducing and measuring electrochemi- luminescence from a labeled EGF ligand. Approximately 1000 cell equivalents per well yielded a signal to background ratio of 20. The observed KD agrees with that reported in the literature and demonstrates that immobilization of the membranes and modification of the ligand do not alter the binding affinity. Binding specificity was confirmed with two inhibitors. The assay can be readily adapted to facilitate analysis of a broad array of receptor-ligand interactions. TM TM A division of Meso Scale Diagnostics,TM LLC. Simple, Rapid Ligand-Binding Assay Using Immobilized Cellular Membranes TM Multi-Array TechnologyTM Multi-Array Technology Unified technology platform with instruments, plates and reagents for drug discovery for drug discovery. Combines the power of microarrays with the sensitivity of electrochemiluminescence Combines the power of microarrays with the sensitivity of electrochemiluminescence.96-, 384- and 1536 microplate formats 96-,Multi-Spot 384- TMand plates 1536 with microplate high density formats. -

Pharmacokinetic-Pharmacodynamic Modelling of Systemic IL13 Blockade by Monoclonal Antibody Therapy: a Free Assay Disguised As Total
pharmaceutics Article Pharmacokinetic-Pharmacodynamic Modelling of Systemic IL13 Blockade by Monoclonal Antibody Therapy: A Free Assay Disguised as Total John Hood 1,*, Ignacio González-García 1 , Nicholas White 1, Leeron Marshall 1,2, Vincent F. S. Dubois 1 , Paolo Vicini 1,3 and Paul G. Baverel 1,4 1 Clinical Pharmacology and Quantitative Pharmacology, AstraZeneca, Cambridge CB21 6GH, UK; [email protected] (I.G.-G.); [email protected] (N.W.); [email protected] (L.M.); [email protected] (V.F.S.D.); [email protected] (P.V.); [email protected] (P.G.B.) 2 Salford Royal Foundation Trust, Salford M6 8HD, UK 3 Confo Therapeutics, 9052 Ghent, Zwijnaarde, Belgium 4 Roche Pharma Research and Early Development, Clinical Pharmacology, Pharmaceutical Sciences, Roche Innovation Center Basel F. Hoffmann-La Roche Ltd., CH-4070 Basel, Switzerland * Correspondence: [email protected]; Tel.: +44-1223-749-6288 Abstract: A sequential pharmacokinetic (PK) and pharmacodynamic (PD) model was built with Nonlinear Mixed Effects Modelling based on data from a first-in-human trial of a novel biologic, MEDI7836. MEDI7836 is a human immunoglobulin G1 lambda (IgG1λ-YTE) monoclonal antibody, Citation: Hood, J.; González-García, with an Fc modification to reduce metabolic clearance. MEDI7836 specifically binds to, and function- I.; White, N.; Marshall, L.; Dubois, ally neutralizes interleukin-13. Thirty-two healthy male adults were enrolled into a dose-escalation V.F.S.; Vicini, P.; Baverel, P.G. clinical trial. Four active doses were tested (30, 105, 300, and 600 mg) with 6 volunteers enrolled Pharmacokinetic-Pharmacodynamic per cohort. Eight volunteers received placebo as control. -

Real-Time Quantitative Measurement of Autocrine Ligand Binding Indicates That Autocrine Loops Are Spatially Localized
Proc. Natl. Acad. Sci. USA Vol. 95, pp. 15368–15373, December 1998 Cell Biology Real-time quantitative measurement of autocrine ligand binding indicates that autocrine loops are spatially localized DOUGLAS A. LAUFFENBURGER*†‡,GREGORY T. OEHRTMAN†,LAURA WALKER†, AND H. STEVEN WILEY§ *Division of Bioengineering & Environmental Health and Center for Biomedical Engineering and †Department of Chemical Engineering, Massachusetts Institute of Technology, Cambridge, MA 02139; and §Department of Pathology, University of Utah Medical Center, Salt Lake City, UT 84132 Communicated by Edwin N. Lightfoot, Jr., University of Wisconsin, Madison, WI, October 15, 1998 (received for review July 21, 1998) ABSTRACT Autocrine ligands are important regulators rapid (,30 sec) and small (,0.1 unit) changes in solution pH of many normal tissues and have been implicated in a number in the cellular microenvironment in an '1 ml chamber above of disease states, including cancer. However, because by the sensor. These pH changes [termed ‘‘extracellular acidifi- definition autocrine ligands are synthesized, secreted, and cation rate’’ (ECAR)] can arise from both metabolic and bound to cell receptors within an intrinsically self-contained regulatory events and have been shown to be quantitatively ‘‘loop,’’ standard pharmacological approaches cannot be used related to specific activation of many types of cell receptors, to investigate relationships between ligandyreceptor binding including tyrosine kinase receptors, G protein receptors, and and consequent cellular responses. We demonstrate here a ion channel receptors (16) with EC50 values similar to those new approach for measurement of autocrine ligand binding to derived from direct-labeled ligand binding (17). Hence, for cells, using a microphysiometer assay originally developed for exogenous ligands the microphysiometer can be used to obtain investigating cell responses to exogenous ligands. -

A Live Cell Nanobret Binding Assay Allows the Study of Ligand-Binding Kinetics to the Adenosine A3 Receptor
Purinergic Signalling https://doi.org/10.1007/s11302-019-09650-9 ORIGINAL ARTICLE A live cell NanoBRET binding assay allows the study of ligand-binding kinetics to the adenosine A3 receptor Monica Bouzo-Lorenzo1,2 & Leigh A. Stoddart 1,2 & Lizi Xia3 & Adriaan P. IJzerman3 & Laura H. Heitman 3 & Stephen J. Briddon1,2 & Stephen J. Hill1,2 Received: 25 November 2018 /Accepted: 14 February 2019 # The Author(s) 2019 Abstract There is a growing interest in understanding the binding kinetics of compounds that bind to G protein-coupled receptors prior to progressing a lead compound into clinical trials. The widely expressed adenosine A3 receptor (A3AR) has been implicated in a range of diseases including immune conditions, and compounds that aim to selectively target this receptor are currently under development for arthritis. Kinetic studies at the A3AR have been performed using a radiolabelled antagonist, but due to the kinetics of this probe, they have been carried out at 10 °C in membrane preparations. In this study, we have developed a live cell NanoBRET ligand binding assay using fluorescent A3AR antagonists to measure kinetic parameters of labelled and unlabelled compounds at the A3AR at physiological temperatures. The kinetic profiles of four fluorescent antagonists were determined in kinetic association assays, and it was found that XAC-ser-tyr-X-BY630 had the longest residence time (RT = 288 ± 62 min) at the A3AR. The association and dissociation rate constants of three antagonists PSB-11, compound 5, and LUF7565 were also determined using two fluorescent ligands (XAC-ser- tyr-X-BY630 or AV039, RT = 6.8 ± 0.8 min) as the labelled probe and compared to those obtained using a radiolabelled antagonist ([3H]PSB-11, RT = 44.6 ± 3.9 min). -

Nitric Oxide Modulation of Interleukin-1Я-Evoked Intracellular
The Journal of Neuroscience, December 15, 2000, 20(24):8980–8986 Nitric Oxide Modulation of Interleukin-1-Evoked Intracellular Ca2؉ Release in Human Astrocytoma U-373 MG Cells and Brain Striatal Slices Antonella Meini,1 Alberto Benocci,1 Maria Frosini,1 Gianpietro Sgaragli,1 Gianpaolo Pessina,2 Carlo Aldinucci,2 Gise` le Tchuisseu Youmbi,1 and Mitri Palmi1 1Istituto di Scienze Farmacologiche and 2Istituto di Fisiologia, Universita` di Siena, 53100 Siena, Italy Intracellular Ca 2ϩ mobilization and release into mammal CSF Ca 2ϩ release induced by 2.5 but not 10 ng/ml IL-1. Ruthenium plays a fundamental role in the etiogenesis of fever induced by red (50 M) and, to a lesser extent, heparin (3 mg/ml) antagonized the proinflammatory cytokine interleukin-1 (IL-1) and other IL-1-induced Ca 2ϩ release, and both compounds administered pyrogens. The source and mechanism of IL-1-induced intracel- together completely abolished this response. Similar results were lular Ca 2ϩ mobilization was investigated using two experimental obtained in human astrocytoma cells in which IL-1 elicited a models. IL-1 (10 ng/ml) treatment of rat striatal slices preloaded delayed (30 min) increase in intracellular Ca 2ϩ concentration 45 2ϩ 2ϩ Ϯ with Ca elicited a delayed (30 min) and sustained increase ([Ca ]i ) (402 71.2% of baseline), which was abolished by 1 45 2ϩ (125–150%) in spontaneous Ca release that was potentiated mML-NAME. These data indicate that the NO/cGMP-signaling by L-arginine (300 M) and counteracted by N--nitro-L-arginine pathway is part of the intracellular mechanism transducing IL- 2ϩ methyl ester (L-NAME) (1 and 3 mM). -

White Paper Recommendations for the Development and Validation Of
The AAPS Journal ( # 2017) DOI: 10.1208/s12248-017-0181-6 White Paper Recommendations for the Development and Validation of Neutralizing Antibody Assays in Support of Biosimilar Assessment D. Gouty,1,16 C. C. Cai,2 X. Y. Cai,3 A. Kasinath,4 V. Kumar,5 S. Alvandkouhi,6 J. Yang,7 S. Pederson,8 B. Babbitt,2 D. Peritt,9 A. Rudy,10 V. Koppenburg,11 A. Dasilva,12 M. Ullmann,13 S. Liu,14 and C. Satterwhite15 Received 23 May 2017; accepted 21 November 2017 Abstract. The American Association of Pharmaceutical Scientists (AAPS) biosimilar focus group on nonclinical and clinical assays has developed this manuscript to guide the industry on best practices and testing strategies when developing neutralizing antibody (NAb) assays for biosimilar programs. The immunogenicity assessment to biosimilar and originator drug products is one of the key aspects of clinical programs for biosimilars to demonstrate biosimilarity. Establishing that there are no clinically meaningful differences in immune response between a proposed product and the originator product is a key element in the demonstration of biosimilarity. It is critical to collect, evaluate, and compare the safety and immunogenicity data from the clinical pharmacology, safety, and/or efficacy studies especially when the originator drug product is known to have potential for immune-mediated toxicity. This manuscript aims to provide a comprehensive review and recommendations on assay formats, critical reagents, approaches to method development, and validation of the neutralizing antibody assays in extrapolation within the scope of biosimilar drug development programs. Even if there are multiple options on the development and validation of NAb assays for biosimilar programs, the type of drug and its MoA will help determine the assay format and technical platform for NAb assessment (e.g., cell-based or non-cell-based assay). -

Directed Evolution of a G Protein-Coupled Receptor for Expression, Stability, and Binding Selectivity
Directed evolution of a G protein-coupled receptor for expression, stability, and binding selectivity Casim A. Sarkar*†‡, Igor Dodevski*†, Manca Kenig*§, Stefan Dudli*, Anja Mohr*, Emmanuel Hermans¶, and Andreas Plu¨ckthun*ʈ *Biochemisches Institut, Universita¨t Zu¨ rich, Winterthurerstrasse 190, CH-8057 Zu¨rich, Switzerland; and ¶Laboratoire de Pharmacologie Expe´rimentale, Universite´catholique de Louvain, Avenue Hippocrate 54.10, B-1200 Bruxelles, Belgium. Edited by William F. DeGrado, University of Pennsylvania, Philadelphia, PA, and approved July 18, 2008 (received for review April 1, 2008) We outline a powerful method for the directed evolution of sequence of a GPCR, keeping all other variables constant, to integral membrane proteins in the inner membrane of Escherichia yield more functionally expressed protein in a convenient het- coli. For a mammalian G protein-coupled receptor, we arrived at a erologous host, Escherichia coli. We used as a model system the sequence with an order-of-magnitude increase in functional ex- rat neurotensin receptor-1 (NTR1), which has been shown to pression that still retains the biochemical properties of wild type. give a detectable yield in E. coli (10, 11) but which still needs to This mutant also shows enhanced heterologous expression in be improved to allow more convenient preparation of milligram eukaryotes (12-fold in Pichia pastoris and 3-fold in HEK293T cells) quantities of receptor. and greater stability when solubilized and purified, indicating that Detailed characterization of the best variant from the selec- the biophysical properties of the protein had been under the tion reported here reveals that it exhibits an order-of-magnitude pressure of selection. -

Quality Controls in Ligand Binding Assays: Recommendations And
The AAPS Journal (2019) 21: 89 DOI: 10.1208/s12248-019-0354-6 White Paper Quality Controls in Ligand Binding Assays: Recommendations and Best Practices for Preparation, Qualification, Maintenance of Lot to Lot Consistency, and Prevention of Assay Drift Mitra Azadeh,1,6 Perceval Sondag,2 Ying Wang,3 Maribeth Raines,4 and Jeffrey Sailstad5 Received 25 April 2019; accepted 6 June 2019; published online 11 July 2019 Abstract. Quality controls (QCs) are the primary indices of assay performance and an important tool in assay lifecycle management. Inclusion of QCs in the testing process allows for the detection of system errors and ongoing assessment of the reliability of the assay. Changes in the performance of QCs are indicative of changes in the assay behavior caused by unintended alterations to reagents or to the operating conditions. The focus of this publication is management of QC life cycle. A consensus view of the ligand binding assay (LBA) community on the best practices for factors that are critical to QC life cycle management including QC preparation, qualification, and trending is presented here. KEY WORDS: LBA; life cycle management; qualification; quality control; trending. INTRODUCTION statistical tools to trend QCs, a practice that is of paramount importance to monitoring performance and managing the life The performance of a ligand binding assay is manifested cycle of quality controls. in the performance of its quality controls during pre-study This publication aims to fill in the gap by providing method validation and in-study sample analysis. Successful guidelines for the management of LBA QC life cycle and its management of QC life cycle requires rigorous and components including recommendations and best practices established methodologies for preparation, qualification as for QC preparation, qualification, and performance trending. -

Analytical Considerations for Ligand Binding Assay Regression Curves and Quality Control Samples
American Journal of Immunology, 2012, 8 (3), 71-77 ISSN 1553-619X ©2012 Science Publication doi:10.3844/ajisp.2012.71.77 Published Online 8 (3) 2012 (http://www.thescipub.com/aji.toc) Biomarker Quantitation: Analytical Considerations for Ligand Binding Assay Regression Curves and Quality Control Samples Mark Dysinger Pfizer Global Research and Development, Eastern Point Road, Groton CT, 06340, USA Received 2012-08-02, Revised 2012-08-17; Accepted 2012-08-25 ABSTRACT As biomarkers grow in relevance for both the design and support of therapeutics and the clinical trials associated with them, there is an ever increasing need for accurate quantitation of these biochemical entities in biological matrices. While quantifying many biotherapeutics via ligand binding assay platforms can be fairly straightforward, biomarkers present some unique challenges that must be taken into account during assay development, validation and subsequent sample analysis. These challenges can be especially confounded by the relationship between two ligand binding assay tools: The regression curve and quality control samples. Due diligence must be performed to develop an assay that takes into account matrix vs. buffer effects and endogenous biomarker presence. Lack of diligence in these areas can lead to less than reliable results, thus potentially rendering the intended use of the assay moot. Keywords: Biomarker, Ligand Binding Assay, Regression Curve, Quality Control 1. INTRODUCTION adequately assess biomarker concentrations in various matrices. Many of these fall into the ligand binding assay Biomarkers play an important role in the category (Sittampalam et al ., 1997; Jong et al ., 2005), development of therapeutics. By up-regulating or down- specifically the microtiter variety.