Toxicological Profile for Beryllium
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Llllllllllllllllllllllllllllllll^
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization llllllllllllllllllllllllllllllll^ International Bureau (10) International Publication Number (43) International Publication Date WO 2018/097733 A3 31 May 2018 (31.05.2018) WIPO I PCT (51) International Patent Classification: (88) Date of publication of the international search report: A61K31/194 (2006.01) A61P 9/00 (2006.01) 02 August 2018 (02.08.2018) A61K31/195 (2006.01) A61P 3/00 (2006.01) A61P 21/00 (2006.01) GOIN 33/48 (2006.01) (21) International Application Number: PCT/NO2017/000032 (22) International Filing Date: 23 November 2017 (23.11.2017) (25) Filing Language: English (26) Publication Language: English (30) Priority Data: 20161866 23 November2016 (23.11.2016) NO (71) Applicant: BOHNE ASK0Y AS [NO/NO]; Romledalen 51, 5310 Hauglandshella (NO). (72) Inventors: BOHNE, Oyvind; Romledalen 51, 5310 Haug- landshella (NO). BOHNE, Victoria; Romledalen 51, 5310 Hauglandshella (NO). (74) Agent: ACAPO AS; P.O. Box 1880 Nordnes, 5817 Bergen (NO). (81) Designated States (unless otherwise indicated, for every kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DJ, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, HR, HU, ID, IL, IN, IR, IS, JO, JP, KE, KG, KH, KN, KP, KR, KW, KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. -

[email protected] +1-703-527-3887 (International) Website
Date of Issue: 17 June 2015 SAFETY DATA SHEET 1. SUBSTANCE AND SOURCE IDENTIFICATION Product Identifier SRM Number: 1877 SRM Name: Beryllium Oxide Powder Other Means of Identification: Not applicable. Recommended Use of This Material and Restrictions of Use This Standard Reference Material (SRM) is intended for use in laboratory analysis and health research for the development and validation of analytical methods and instruments used to determine beryllium, as well as for proficiency testing of laboratories involved in beryllium determinations. A unit of SRM 1877 consists of one bottle containing 20 g of beryllium oxide powder. Company Information National Institute of Standards and Technology Standard Reference Materials Program 100 Bureau Drive, Stop 2300 Gaithersburg, Maryland 20899-2300 Telephone: 301-975-2200 Emergency Telephone ChemTrec: FAX: 301-948-3730 1-800-424-9300 (North America) E-mail: [email protected] +1-703-527-3887 (International) Website: http://www.nist.gov/srm 2. HAZARDS IDENTIFICATION Classification Physical Hazard: Not classified. Health Hazard: Acute Toxicity, Inhalation Category 2 Skin Corrosion/Irritation Category 2 Serious Eye Damage/Irritation Category 2B Skin Sensitization Category 1 Carcinogenicity Category 1A STOT-Repeat Exposure Category 1 Label Elements Symbol Signal Word DANGER Hazard Statement(s) H330 Fatal if inhaled. H315+H320 Causes skin and eye irritation. H317 May cause an allergic skin reaction. H350 May cause lung cancer. H372 Causes damage to lungs through prolonged or repeated inhalation. Precautionary Statement(s) P201 Obtain special instructions before use. P202 Do not handle until all safety precautions have been read and understood. P260 Do not breathe dust. P264 Wash hands thoroughly after handling. -

The Heat of Combustion of Beryllium in Fluorine*
JOURNAL OF RESEARCH of the National Bureau of Standards -A. Physics and Chemistry Vol. 73A, No.3, May- June 1969 The Heat of Combustion of Beryllium in Fluorine* K. L. Churney and G. T. Armstrong Institute for Materials Research, National Bureau of Standards, Washington, D.C. 20234 (February 11, 1969) An expe rimental dete rmination of the e ne rgies of combustion in Auorine of polyte traAuoroethylene film and Q.o wder and of mixtures of beryllium with polytetraAuoroethyle ne gi ves for reacti on ( 1)f).H ~.or= - 1022.22 kJ 111 0 1- 1 (- 244.32 kcal mol - I) wit h a n ove ra ll precision of 0.96 kJ 111 0 1- 1 (0. 23 kcal 111 0 1- 1 ) at the 95 pe rce nt confid ence limit s. The tota l un cert a int y is estimated not to exceed ±3.2 kJ mol- I (±0.8 kcal mol - I). The measureme nts on polytetraflu oroeth yle ne giv e for reaction (2a) and reacti on (2 b) f).H ~. o c =- 10 369. 7 and - 10392.4 Jg- I, respective ly. Overall precisions e xpressed at the 95 pe rcent confide nce Ijmits are 3.3 and 6.0 Jg- I, respective ly. Be(c)+ F,(g) = BeF2(a morphous) (1) C,F.(polym e r powd er) + 2F2(g) = 2CF.(g) (2a) C2F.(polyme r film ) + 2F2 (g) = 2CF.(g) (2b) Be2C and Be metal were observed in a small carbonaceous residue from the co mbustion of the beryll iul11 -polytetraAuoroethylene mixtures. -
Exposure Data
BERYLLIUM AND BERYLLIUM eOMPOUNDS Beryllium and beryllium compounds were considered by previous Working Groups, In 1971,1979 and 1987 (lARe, 1972, 1980, 1987a). New data have since become available, and these are included in the present monograph and have been taken into consideration In the evaluation. The agents considered herein Include (a) metallic beryllium, (b) beryllium- aluminium and -copper alloys and (c) some beryllum compounds. 1. Exposure Data 1.1 Chemical and physical data and analysis 1.1.1 Synonyms, trade names and molecular formulae Synonyms, trade names and molecular formulae for beryllium, beryllum-aluminium and -copper alloys and certain beryllium compounds are presented in Thble 1. The list is not exhaustive, nor does it comprise necessarily the most commercially important beryllum- containing substances; rather, it indicates the range of beryllum compounds available. 1. 1.2 Chemical and physical properties of the pure substances Selected chemical and physical properties of beryllium, beryllum-aluminium and -copper alloys and the beryllium compounds covered in this monograph are presented in Thble 2. The French chemist Vauquelin discovered beryllium in 1798 as the oxide, while analysing emerald to prove an analogous composition (Newland, 1984). The metallc element was first isolated in independent experiments by Wöhler (1828) and Bussy (1828), who called it 'glucinium' owing to the sweet taste of its salts; that name is stil used in the French chemical literature. Wöhler's name 'beryllum' was offcially recognized by IUPAe in 1957 (WHO, 1990). The atomic weight and corn mon valence of beryllum were originally the subject of much controversy but were correctly predicted by Mendeleev to be 9 and + 2, respectively (Everest, 1973). -

Neopterin, a Promising Biomarker for the Diagnosis of Intraocular Inflammation
ISSN 0030-0675. Journal of Ophthalmology (Ukraine) - 2021 - Number 3 (500) Neopterin, a promising biomarker for the diagnosis of intraocular inflammation N. B. Kuryltsiv 1, O. V. Zborovska 2 1 Danylo Halytsky Lviv National Medical We reviewed studies on the role of neopterin as a biomarker of various University infectious and non-infectious diseases and presented the benefits of Lviv (Ukraine) measuring the levels of this biomarker in biological fluids in disorders involving cell-mediated immunity. The results of relevant studies in multiple 2 SI "The Filatov Institute of Eye fields of medicine are desctibed herein. Measuring neoptherin levels in Diseases and Tissue Therapy of the biological fluids may be beneficial not only for diagnosis or verification of NAMS of Ukraine"; a particular disease, but also for differentiation of the disease from others Одеса (Україна) resembling it, assessment of treatment efficacy and prediction of subsequent disease course. E-mail: [email protected] Keywords: neoptherin, biomarker of inflammation, cell- mediated immunity, biological fluid The problem of uveitis is still a problem of significant active cytokine interaction is essential for full immune proportions. The importance of the disease is determined response. Usually, the biological effect of a single cytokine by its prevalence, chronic recurrent course, numerous is a portion of the combination effect of different cytokines potential complications and a high rate of certified visual [20]. disability among patients with the disease [1-4]. Uveitis is It is important that concentrations of individual estimated to be the cause of 5–10% of blindness or visual cytokines in biological fluids reflect only limited impairment worldwide [5]. -

Understanding Lead Uptake and Effects Across Species Lines: a Conservation Medicine Based Approach
UNDERSTANDING LEAD UPTAKE AND EFFECTS ACROSS SPECIES LINES: A CONSERVATION MEDICINE BASED APPROACH MARK A. POKRAS AND MICHELLE R. KNEELAND Center for Conservation Medicine, Tufts University Cummings School of Veterinary Medicine, 200 Westboro Rd., North Grafton, MA 01536, USA. E-mail: [email protected] ABSTRACT.—Conservation medicine examines the linkages among the health of people, animals and the environment. Few issues illustrate this approach better than an examination of lead (Pb) toxicity. We briefly review the current state of knowledge on the toxicity of lead and its effects on wildlife, humans, and domestic animals. Lead is cheap and there is a long tradition of its use. But the toxic effects of Pb have also been recognized for centuries. As a result, western societies have greatly reduced many traditional uses of Pb, including many paints, gasoline and solders because of threats to the health of humans and the environment. Legisla- tion in several countries has eliminated the use of lead shot for hunting waterfowl. Despite these advances, a great many Pb products continue to be readily available. Conservationists recognize that hunting, angling and shooting sports deposit thousands of tons of Pb into the environment each year. Because of our concerns for human health and over 100 years of focused research, we know the most about lead poisoning in people. Even today, our knowledge of the long-term sublethal effects of Pb on human health continues to grow dramatically. Our knowledge about lead poisoning in domestic animals is signifi- cantly less. For wild animals, our understanding of lead poisoning is roughly where our knowledge about humans was in the mid-1800s when Tanquerel Des Planches made his famous medical observations (Tan- querel Des Planches 1850). -

Gender and the Quest in British Science Fiction Television CRITICAL EXPLORATIONS in SCIENCE FICTION and FANTASY (A Series Edited by Donald E
Gender and the Quest in British Science Fiction Television CRITICAL EXPLORATIONS IN SCIENCE FICTION AND FANTASY (a series edited by Donald E. Palumbo and C.W. Sullivan III) 1 Worlds Apart? Dualism and Transgression in Contemporary Female Dystopias (Dunja M. Mohr, 2005) 2 Tolkien and Shakespeare: Essays on Shared Themes and Language (ed. Janet Brennan Croft, 2007) 3 Culture, Identities and Technology in the Star Wars Films: Essays on the Two Trilogies (ed. Carl Silvio, Tony M. Vinci, 2007) 4 The Influence of Star Trek on Television, Film and Culture (ed. Lincoln Geraghty, 2008) 5 Hugo Gernsback and the Century of Science Fiction (Gary Westfahl, 2007) 6 One Earth, One People: The Mythopoeic Fantasy Series of Ursula K. Le Guin, Lloyd Alexander, Madeleine L’Engle and Orson Scott Card (Marek Oziewicz, 2008) 7 The Evolution of Tolkien’s Mythology: A Study of the History of Middle-earth (Elizabeth A. Whittingham, 2008) 8 H. Beam Piper: A Biography (John F. Carr, 2008) 9 Dreams and Nightmares: Science and Technology in Myth and Fiction (Mordecai Roshwald, 2008) 10 Lilith in a New Light: Essays on the George MacDonald Fantasy Novel (ed. Lucas H. Harriman, 2008) 11 Feminist Narrative and the Supernatural: The Function of Fantastic Devices in Seven Recent Novels (Katherine J. Weese, 2008) 12 The Science of Fiction and the Fiction of Science: Collected Essays on SF Storytelling and the Gnostic Imagination (Frank McConnell, ed. Gary Westfahl, 2009) 13 Kim Stanley Robinson Maps the Unimaginable: Critical Essays (ed. William J. Burling, 2009) 14 The Inter-Galactic Playground: A Critical Study of Children’s and Teens’ Science Fiction (Farah Mendlesohn, 2009) 15 Science Fiction from Québec: A Postcolonial Study (Amy J. -

An Exploratory Study of Neopterin and Kynurenine Pathway in Pterygium Received January 5, 2019; Accepted June 25, 2019
Pteridines 2019; 30: 153–157 Research Article Open Access Bilge Kilicarslan*, Aziz Cardak, Gozde Girgin, Ozlem Evren Kemer, Terken Baydar An exploratory study of neopterin and kynurenine pathway in pterygium https://doi.org/10.1515/pteridines-2019-0019 received January 5, 2019; accepted June 25, 2019. Introduction Abstract: Pterygium is an inflammatory, vascular and Pterygium is an inflammatory, fibrovascular and degenerative disorder with unknown aetiology. The aim degenerative ocular disease. The disease has taken its name of this study was to evaluate the changes in neopterin from the Greek word ‘pterygion’, meaning ‘small wing’ levels, reflecting T-cell immunity, and the kynurenine due to the triangular wing-shaped growth of conjunctival pathway, the main degradation process of tryptophan, tissue on the cornea [1, 2]. In pterygium inflammation, in pterygium. For this purpose, neopterin concentrations uncontrolled cell division and angiogenesis are observed were measured in serum and tear samples by enzyme- together which refer to neoplasia; however, pterygium linked immunosorbent assay (ELISA) in pterygium patients is considered as neither a cancer, nor an inflammatory (n=31) and control group (n=32). Kynurenine (KYN) and disease. According to some researchers, pterygium can be tryptophan (TRP) serum levels were simultaneously defined as a “neoplastic-like growth disorder” [3-5]. It is determined by high-performance liquid chromatography known that factors such as ultraviolet (UV) radiation, p53 (HPLC) for evaluation of the kynurenine pathway. Serum tumour suppressor gene, immunologic and inflammatory neopterin concentrations and kynurenine to tryptophan mechanisms play a role in the pathogenesis, but its ratio (KYN/TRP) as an index of tryptophan breakdown aetiology remains unclear [6-8]. -
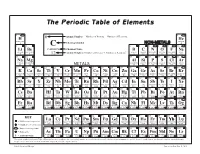
The Periodic Table of Elements
The Periodic Table of Elements 1 2 6 Atomic Number = Number of Protons = Number of Electrons HYDROGENH HELIUMHe 1 Chemical Symbol NON-METALS 4 3 4 C 5 6 7 8 9 10 Li Be CARBON Chemical Name B C N O F Ne LITHIUM BERYLLIUM = Number of Protons + Number of Neutrons* BORON CARBON NITROGEN OXYGEN FLUORINE NEON 7 9 12 Atomic Weight 11 12 14 16 19 20 11 12 13 14 15 16 17 18 SODIUMNa MAGNESIUMMg ALUMINUMAl SILICONSi PHOSPHORUSP SULFURS CHLORINECl ARGONAr 23 24 METALS 27 28 31 32 35 40 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 POTASSIUMK CALCIUMCa SCANDIUMSc TITANIUMTi VANADIUMV CHROMIUMCr MANGANESEMn FeIRON COBALTCo NICKELNi CuCOPPER ZnZINC GALLIUMGa GERMANIUMGe ARSENICAs SELENIUMSe BROMINEBr KRYPTONKr 39 40 45 48 51 52 55 56 59 59 64 65 70 73 75 79 80 84 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 RUBIDIUMRb STRONTIUMSr YTTRIUMY ZIRCONIUMZr NIOBIUMNb MOLYBDENUMMo TECHNETIUMTc RUTHENIUMRu RHODIUMRh PALLADIUMPd AgSILVER CADMIUMCd INDIUMIn SnTIN ANTIMONYSb TELLURIUMTe IODINEI XeXENON 85 88 89 91 93 96 98 101 103 106 108 112 115 119 122 128 127 131 55 56 72 73 74 75 76 77 78 79 80 81 82 83 84 85 86 CESIUMCs BARIUMBa HAFNIUMHf TANTALUMTa TUNGSTENW RHENIUMRe OSMIUMOs IRIDIUMIr PLATINUMPt AuGOLD MERCURYHg THALLIUMTl PbLEAD BISMUTHBi POLONIUMPo ASTATINEAt RnRADON 133 137 178 181 184 186 190 192 195 197 201 204 207 209 209 210 222 87 88 104 105 106 107 108 109 110 111 112 113 114 115 116 117 118 FRANCIUMFr RADIUMRa RUTHERFORDIUMRf DUBNIUMDb SEABORGIUMSg BOHRIUMBh HASSIUMHs MEITNERIUMMt DARMSTADTIUMDs ROENTGENIUMRg COPERNICIUMCn NIHONIUMNh -

Llfltfits Paul Stanek, MST-6
COAJF- 9 50cDo/-~^0 LA-UR- 9 5-1666 Title: AGE HARDENING IN RAPIDLY SOLIDIFIED AND HOT ISOSTATICALLY PRESSED BERYLLIUM-ALUM1UM SILVER ALLOYS HVAUli Author(s): David H. Carter, MST-6 Andrew McGeorge, MST-6 Loren A. Jacobson, MST-6 llfltfits Paul Stanek, MST-6 IflllS,Ic 8-o° ,S8 si Proceedings of TMS Annual Meeting, Las Vegas, jJffilJSif—- Nevada, February 1995 as-IVUiS' i in Los Alamos NATIONAL LABORATORY Los Alamos National Laboratory, an affirmative action/equal opportunity employer, is operated by the University of California for the U.S. Department of Energy under contract W-7405-ENG-36. By acceptance of this article, the publisher recognizes that the U.S. Government retains a nonexclusive, royalty-free license to publish or reproduce the published form of this contribution, or to allow others to do so, for U.S. Government purposes. The Los Alamos National Laboratory requests that the publisher identify this article as work performed under the auspices of the U.S. Department of Energy* FotmNo.B36R5 MCTOIQimnM f\c mie hAMMr&T 10 i mi in ST26291M1 DISCLAIMER Portions of this document may be illegible in electronic image products. Images are produced from the best available original document. Age Hardening in Rapidly Solidified and Hot Isostatically Pressed Beryllium-Aluminum-Silver Alloys David H. Carter, Andrew C. McGeorge,* Loren A. Jacobson, and Paul W. Stanek Los Alamos National Laboratory, Los Alamos NM 87545 Abstract Three different alloys of beryllium, aluminum and silver were processed to powder by centrifugal atomization in a helium atmosphere. Alloy com• positions were, by weight, 50% Be, 47.5% Al, 2.5% Ag, 50% Be, 47% Al, 3% Ag, and 50% Be, 46% Al, 4% Ag. -

Toxicological Profile for Beryllium
BERYLLIUM 19 3. HEALTH EFFECTS 3.1 INTRODUCTION The primary purpose of this chapter is to provide public health officials, physicians, toxicologists, and other interested individuals and groups with an overall perspective on the toxicology of beryllium. It contains descriptions and evaluations of toxicological studies and epidemiological investigations and provides conclusions, where possible, on the relevance of toxicity and toxicokinetic data to public health. A glossary and list of acronyms, abbreviations, and symbols can be found at the end of this profile. 3.2 DISCUSSION OF HEALTH EFFECTS BY ROUTE OF EXPOSURE To help public health professionals and others address the needs of persons living or working near hazardous waste sites, the information in this section is organized first by route of exposure (inhalation, oral, and dermal) and then by health effect (death, systemic, immunological, neurological, reproductive, developmental, genotoxic, and carcinogenic effects). These data are discussed in terms of three exposure periods: acute (14 days or less), intermediate (15–364 days), and chronic (365 days or more). Levels of significant exposure for each route and duration are presented in tables and illustrated in figures. The points in the figures showing no-observed-adverse-effect levels (NOAELs) or lowest-observed-adverse-effect levels (LOAELs) reflect the actual doses (levels of exposure) used in the studies. LOAELS have been classified into "less serious" or "serious" effects. "Serious" effects are those that evoke failure in a biological system and can lead to morbidity or mortality (e.g., acute respiratory distress or death). "Less serious" effects are those that are not expected to cause significant dysfunction or death, or those whose significance to the organism is not entirely clear. -

+14 Days of Tv Listings Free
CINEMA VOD SPORTS TECH + 14 DAYS OF TV LISTINGS 1 JUNE 2015 ISSUE 2 TVGUIDE.CO.UK TVDAILY.COM Jurassic World Orange is the New Black Formula 1 Addictive Apps FREE 1 JUNE 2015 Issue 2 Contents TVGUIDE.CO.UK TVDAILY.COM EDITOR’S LETTER 4 Latest TV News 17 Food We are living in a The biggest news from the world of television. Your television dinners sorted with revolutionary age for inspiration from our favourite dramas. television. Not only is the way we watch television being challenged by the emergence of video on 18 Travel demand, but what we watch on television is Journey to the dizzying desert of Dorne or becoming increasingly take a trip to see the stunning setting of diverse and, thankfully, starting to catch up with Downton Abbey. real world demographics. With Orange Is The New Black back for another run on Netflix this month, we 19 Fashion decided to celebrate the 6 Top 100 WTF Steal some shadespiration from the arduous journey it’s taken to get to where we are in coolest sunglass-wearing dudes on TV. 2015 (p14). We still have a Moments (Part 2) long way to go, but we’re The final countdown of the most unbelievable getting there. Sports Susan Brett, Editor scenes ever to grace the small screen, 20 including the electrifying number one. All you need to know about the upcoming TVGuide.co.uk Formula 1 and MotoGP races. 104-08 Oxford Street, London, W1D 1LP [email protected] 8 Cinema CONTENT 22 Addictive Apps Editor: Susan Brett Everything you need to know about what’s Deputy Editor: Ally Russell A handy guide to all the best apps for Artistic Director: Francisco on at the Box Office right now.