Restless Legs Syndrome and Excessive Daytime Sleepiness
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Modafinil/Armodafinil (Provigil ® /Nuvigil
Drug and Biologic Coverage Policy Effective Date ............................................ 7/1/2020 Next Review Date… ..................................... 7/1/2021 Coverage Policy Number .................................. 1501 Modafinil / Armodafinil for Individual and Family Plans Table of Contents Related Coverage Resources Coverage Policy ................................................... 1 Obstructive Sleep Apnea Treatment Services FDA Approved Indications ................................... 2 Recommended Dosing ........................................ 3 General Background ............................................ 3 Coding/ Billing Information ................................... 6 References .......................................................... 6 INSTRUCTIONS FOR USE The following Coverage Policy applies to health benefit plans administered by Cigna Companies. Certain Cigna Companies and/or lines of business only provide utilization review services to clients and do not make coverage determinations. References to standard benefit plan language and coverage determinations do not apply to those clients. Coverage Policies are intended to provide guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please note, the terms of a customer’s particular benefit plan document [Group Service Agreement, Evidence of Coverage, Certificate of Coverage, Summary Plan Description (SPD) or similar plan document] may differ significantly from the standard benefit plans upon which these Coverage Policies -

Excessive Daytime Somnolence S44 (1)
EXCESSIVE DAYTIME SOMNOLENCE S44 (1) Excessive Daytime Somnolence Last updated: May 8, 2019 Clinical Features .................................................................................................................... 1 Differential Diagnosis ........................................................................................................... 2 Diagnosis ............................................................................................................................... 2 Treatment ............................................................................................................................... 2 NARCOLEPSY ........................................................................................................................................... 2 CLINICAL FEATURES .............................................................................................................................. 3 DIAGNOSIS ............................................................................................................................................. 4 MANAGEMENT ....................................................................................................................................... 4 IDIOPATHIC (PRIMARY) HYPERSOMNIA ................................................................................................. 5 KLEINE-LEVIN SYNDROME ...................................................................................................................... 6 SLEEP APNEA .......................................................................................................................................... -

Sleep Disturbance in Movement Disorders
Movement disorders J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp-2020-325546 on 19 March 2021. Downloaded from Review Sleep disturbance in movement disorders: insights, treatments and challenges Grace A Bailey ,1 Emily K Hubbard,2 Alfonso Fasano,3,4,5 Marina AJ Tijssen ,6 Timothy Lynch,7 Kirstie N Anderson,8 Kathryn J Peall 1 ► Prepublication history ABSTRACT well established as predating motor symptom and additional material is Sleep and circadian rhythm disturbances are central onset.1 In contrast, those such as adult- onset published online only. To view please visit the journal online features of many movement disorders, exacerbating primary, idiopathic dystonia, may have poor (http:// dx. doi. org/ 10. 1136/ motor and non- motor symptoms and impairing quality sleep with evidence suggesting a link to psychi- jnnp- 2020- 325546). of life. Understanding these disturbances to sleep is atric symptom severity.2 1 clinically important and may further our understanding This review provides an overview of the Neuroscience and Mental of the underlying movement disorder. This review common sleep disorders and the evidence to Health Research Institute, Cardiff University, Cardiff, UK evaluates the current anatomical and neurochemical date for the patterns and prevalence across a 2School of Medicine, Cardiff understanding of normal sleep and the recognised spectrum of movement disorders. We discuss the University, Cardiff, UK primary sleep disorders. In addition, we undertook a 3 tools available for sleep assessment, the impact Edmond J Safra Program in systematic review of the evidence for disruption to of medication used in motor symptom manage- Parkinson’s Disease, Morton and Gloria Shulman Movement sleep across multiple movement disorders. -

Treatment of Sleep Disorders in Dementia Sharon Ooms, Msc1,2 Yo-El Ju, MD MSCI3,*
Curr Treat Options Neurol (2016) 18:40 DOI 10.1007/s11940-016-0424-3 Dementia (E McDade, Section Editor) Treatment of Sleep Disorders in Dementia Sharon Ooms, MSc1,2 Yo-El Ju, MD MSCI3,* Address 1Department of Geriatric Medicine, Radboud University Medical Centre, Nijmegen, The Netherlands 2Radboud Alzheimer Centre, Radboud University Medical Centre, Nijmegen, The Netherlands *3Department of Neurology, Washington University School of Medicine, 660 South Euclid Avenue, Box 8111, Saint Louis, MO, 63110, USA Email: [email protected] * Springer Science+Business Media New York 2016 This article is part of the Topical Collection on Dementia Keywords Sleep I Insomnia I Circadian I Dementia I Alzheimer’s disease I Dementia with Lewy bodies I Lewy body disease I Frontotemporal dementia I Parkinson’s disease with dementia I REM sleep behavior disorder Opinion statement Sleep and circadian disorders occur frequently in all types of dementia. Due to the multifactorial nature of sleep problems in dementia, we propose a structured approach to the evaluation and treatment of these patients. Primary sleep disorders such as obstructive sleep apnea should be treated first. Comorbid conditions and medications that impact sleep should be optimally managed to minimize negative effects on sleep. Patients and caregivers should maintain good sleep hygiene, and social and physical activity should be encouraged during the daytime. Given the generally benign nature of bright light therapy and melatonin, these treatments should be tried first. Pharmacolog- ical treatments should be added cautiously, due to the risk of cognitive side effects, sedation, and falls in the demented and older population. Regardless of treatment modality, it is essential to follow patients with dementia and sleep disorders closely, with serial monitoring of individual response to treatment. -

A Comparison of Idiopathic Hypersomnia and Narcolepsy-Cataplexy Using Self Report Measures and Sleep Diary Data
57676ournal ofNeurology, Neurosurgery, and Psychiatry 1996;60:576-578 SHORT REPORT J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.60.5.576 on 1 May 1996. Downloaded from A comparison of idiopathic hypersomnia and narcolepsy-cataplexy using self report measures and sleep diary data Dorothy Bruck, J D Parkes Abstract Published data comparing patients with IH Eighteen patients with idiopathic hyper- and patients with NLS outside the sleep labo- somnia (IH) were compared with 50 ratory are scarce. Using self report question- patients with the narcoleptic syndrome of naires and sleep diary data our aim was to cataplexy and daytime sleepiness (NLS) determine the extent of group differences and using self report questionnaires and a which variables best discriminated between IH diary of sleep/wake patterns. The IH and NLS. group reported more consolidated noc- turnal sleep, a lower propensity to nap, greater refreshment after naps, and a Patients and methods greater improvement in excessive day- DIAGNOSTIC CRITERIA time sleepiness since onset than the NLS Idiopathic hypersomnia group. In IH, the onset of excessive day- Patients were selected with a complaint of time sleepiness was predominantly asso- excessive daytime sleepiness without cataplexy ciated with familial inheritance or a viral and with no evidence of any medical, psycho- illness. Two variables-number of logical, drug related, or respiratory disorder. reported awakenings during nocturnal All patients met diagnostic criteria ascertained sleep and the reported change in sleepi- from questionnaire responses: Epworth sleepi- ness since onset-provided maximum ness scale score8 > 13; duration of excessive discrimination between the IH and NLS daytime sleepiness > five years, profile of groups. -
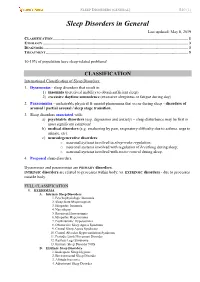
Sleep Disorders in General Last Updated: May 8, 2019 CLASSIFICATION
SLEEP DISORDERS (GENERAL) S40 (1) Sleep Disorders in General Last updated: May 8, 2019 CLASSIFICATION ...................................................................................................................................... 1 ETIOLOGY ................................................................................................................................................ 3 DIAGNOSIS................................................................................................................................................ 3 TREATMENT ............................................................................................................................................. 5 10-15% of population have sleep-related problems! CLASSIFICATION International Classification of Sleep Disorders: 1. Dyssomnias - sleep disorders that result in: 1) insomnia (perceived inability to obtain sufficient sleep) 2) excessive daytime somnolence (excessive sleepiness or fatigue during day) 2. Parasomnias - undesirable physical & mental phenomena that occur during sleep - disorders of arousal / partial arousal / sleep stage transition. 3. Sleep disorders associated with: a) psychiatric disorders (esp. depression and anxiety) – sleep disturbance may be first or most significant symptom! b) medical disorders (e.g. awakening by pain, respiratory difficulty due to asthma, urge to urinate, etc). c) neurodegenerative disorders: o neuronal systems involved in sleep-wake regulation; o neuronal systems involved with regulation of breathing during -
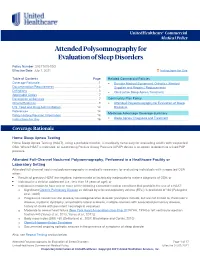
Attended Polysomnography for Evaluation of Sleep Disorders
UnitedHealthcare® Commercial Medical Policy Attended Polysomnography for Evaluation of Sleep Disorders Policy Number: 2021T0334GG Effective Date: July 1, 2021 Instructions for Use Table of Contents Page Related Commercial Policies Coverage Rationale ....................................................................... 1 • Durable Medical Equipment, Orthotics, Medical Documentation Requirements ...................................................... 3 Supplies and Repairs/ Replacements Definitions ...................................................................................... 3 • Obstructive Sleep Apnea Treatment Applicable Codes .......................................................................... 7 Description of Services ................................................................. 7 Community Plan Policy Clinical Evidence ........................................................................... 9 • Attended Polysomnography for Evaluation of Sleep U.S. Food and Drug Administration ........................................... 14 Disorders References ................................................................................... 14 Medicare Advantage Coverage Summary Policy History/Revision Information ........................................... 16 • Sleep Apnea: Diagnosis and Treatment Instructions for Use ..................................................................... 16 Coverage Rationale Home Sleep Apnea Testing Home Sleep Apnea Testing (HSAT), using a portable monitor, is medically necessary for evaluating -

Calcium, Magnesium, Potassium, and Sodium Oxybates) Oral Solution in Adult Patients with Idiopathic Hypersomnia at 2021 American Academy of Neurology Annual Meeting
Jazz Pharmaceuticals Presents Phase 3 Study Results of Xywav™ (calcium, magnesium, potassium, and sodium oxybates) Oral Solution in Adult Patients with Idiopathic Hypersomnia at 2021 American Academy of Neurology Annual Meeting April 20, 2021 Xywav demonstrated statistically significant differences in change in Epworth Sleepiness Scale score (p-value <0.0001), Patient Global Impression of Change (p-value <0.0001) and the Idiopathic Hypersomnia Severity Scale (p-value <0.0001) The safety profile in this study was consistent with the known safety profile of Xywav with no new safety signals observed in this population Company to host investor webcast today at 12:30 p.m. ET DUBLIN, April 20, 2021 /PRNewswire/ -- Jazz Pharmaceuticals plc (Nasdaq: JAZZ) today announced positive results from the Phase 3 study of XywavTM (calcium, magnesium, potassium, and sodium oxybates) oral solution in adult patients with idiopathic hypersomnia, which will be presented during the Clinical Trials Plenary Session of the 2021 American Academy of Neurology (AAN) Annual Meeting between 10:00 a.m. and 12:30 p.m. ET. Jazz will host an investor and analyst presentation via webcast today at 12:30 p.m. ET. Today's presentation will further quantify the previously reported Phase 3 top-line results. These additional data were submitted to the U.S. Food and Drug Administration (FDA) in the supplemental New Drug Application that was recently accepted for filing and granted Priority Review. "The efficacy and safety results demonstrate the potential Xywav has for people living with idiopathic hypersomnia, a debilitating, chronic sleep disorder for which there are no approved treatments in the U.S.," said Robert Iannone, M.D., M.S.C.E., executive vice president, research and development and chief medical officer of Jazz Pharmaceuticals. -

Idiopathic-Hypersomnia-.Pdf
Research & Reviews: Neuroscience Idiopathic Hypersomnia Diksha Gupta1* and Trisha Chatterjee2 1Amity Institute of Pharmacy, Amity University, India 2Department of Biotechnology, Amity University, India Review Article Received date: 08/11/2016 ABSTRACT Accepted date: 27/01/2017 Sleep is an unconsciousness form by which the person Published date: 06/02/2017 could be aroused by sensory or other stimuli. These days due to psychological and social dysfunction our daily routine affects the *For Correspondence quality of our life, according to survey much health related issues are being reported due to lack of sleep. An ancient literature Gupta D, Amity University, Noida, UP, India, Tel: review was given and explained the theory about the leading 8588829759. symptom of idiopathic hypersomnia was sleep drunkenness and the first patient was thus diagnosed with prolonged nocturnal E-mail: [email protected] sleep accompanied by excessive daytime sleepiness with long naps and difficult awakening. A severe issue with this disease is Keywords: Idiopathic hypersomnia, Lengthy that most people tend to suffer from "Depression". Due to ischemic sleep, Narcolepsy, Obstructive sleep changes along the border of mesencephalon and diencephalon and post-traumatic etiology in other, people thus suffer from "sleep apnea, Narcolepsy, Bruxism, Non-rapid eye drunkenness". The term idiopathic hypersomnia was given a variety movement, Hypersomnia of clinical labels including idiopathic central nervous hypersomnia or hypersomnolence, functional hypersomnia, mixed or harmonious hypersomnia, hypersomnia with automatic behavior, and non-rapid eye movement (NREM) narcolepsy. Two different clinical forms were recommended —idiopathic hypersomnia with long sleep time and IH without long sleep time which then reappeared in the latest International Classification of Sleep Disorders. -

Corticalâ•Fisubcortical Interactions In
Washington University School of Medicine Digital Commons@Becker Open Access Publications 2014 Cortical–subcortical interactions in hypersomnia disorders: Mechanisms underlying cognitive and behavioral aspects of the sleep–wake cycle Linda J. Larson-Prior Washington University School of Medicine in St. Louis Yo-El Ju Washington University School of Medicine in St. Louis James E. Galvin New York University School of Medicine Follow this and additional works at: https://digitalcommons.wustl.edu/open_access_pubs Recommended Citation Larson-Prior, Linda J.; Ju, Yo-El; and Galvin, James E., ,"Cortical–subcortical interactions in hypersomnia disorders: Mechanisms underlying cognitive and behavioral aspects of the sleep–wake cycle." Frontiers in Neurology.5,. 165. (2014). https://digitalcommons.wustl.edu/open_access_pubs/3264 This Open Access Publication is brought to you for free and open access by Digital Commons@Becker. It has been accepted for inclusion in Open Access Publications by an authorized administrator of Digital Commons@Becker. For more information, please contact [email protected]. REVIEW ARTICLE published: 11 September 2014 doi: 10.3389/fneur.2014.00165 Cortical–subcortical interactions in hypersomnia disorders: mechanisms underlying cognitive and behavioral aspects of the sleep–wake cycle Linda J. Larson-Prior 1,2*,Yo-El Ju 2 and James E. Galvin3,4,5 1 Department of Radiology, Washington University School of Medicine, St. Louis, MO, USA 2 Department of Neurology, Washington University School of Medicine, St. Louis, MO, USA 3 Departments of Neurology, New York University Langone School of Medicine, New York, NY, USA 4 Department of Psychiatry, New York University Langone School of Medicine, New York, NY, USA 5 Department of Population Health, New York University Langone School of Medicine, New York, NY, USA Edited by: Subcortical circuits mediating sleep–wake functions have been well characterized in ani- Maria Engström, Linköping mal models, and corroborated by more recent human studies. -
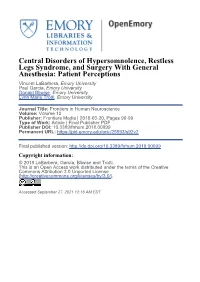
Central Disorders of Hypersomnolence, Restless Legs Syndrome, and Surgery with General Anesthesia: Patient Perceptions
Central Disorders of Hypersomnolence, Restless Legs Syndrome, and Surgery With General Anesthesia: Patient Perceptions Vincent LaBarbera, Emory University Paul Garcia, Emory University Donald Bliwise, Emory University Lynn Marie Trotti, Emory University Journal Title: Frontiers in Human Neuroscience Volume: Volume 12 Publisher: Frontiers Media | 2018-03-20, Pages 99-99 Type of Work: Article | Final Publisher PDF Publisher DOI: 10.3389/fnhum.2018.00099 Permanent URL: https://pid.emory.edu/ark:/25593/s92v2 Final published version: http://dx.doi.org/10.3389/fnhum.2018.00099 Copyright information: © 2018 LaBarbera, García, Bliwise and Trotti. This is an Open Access work distributed under the terms of the Creative Commons Attribution 3.0 Unported License (http://creativecommons.org/licenses/by/3.0/). Accessed September 27, 2021 12:18 AM EDT ORIGINAL RESEARCH published: 20 March 2018 doi: 10.3389/fnhum.2018.00099 Central Disorders of Hypersomnolence, Restless Legs Syndrome, and Surgery With General Anesthesia: Patient Perceptions Vincent LaBarbera 1, Paul S. García 2,3, Donald L. Bliwise 1 and Lynn M. Trotti 1* 1 Sleep Center and Department of Neurology, Emory University School of Medicine, Atlanta, GA, United States, 2 Department of Anesthesiology, Emory University School of Medicine, Atlanta, GA, United States, 3 Research and Anesthesiology Service Lines, Atlanta VA Medical Center, Atlanta, GA, United States Introduction: The importance of obstructive sleep apnea in patients undergoing surgery with general anesthesia is well-defined, but the surgical and anesthetic implications of other sleep disorders are less clear. We sought to evaluate response to surgery with general anesthesia in patients with central disorders of hypersomnolence or restless legs Edited by: syndrome. -

The Prevalence and Characteristics of Primary Headache and Dream
RESEARCH ARTICLE The Prevalence and Characteristics of Primary Headache and Dream-Enacting Behaviour in Japanese Patients with Narcolepsy or Idiopathic Hypersomnia: A Multi-Centre Cross-Sectional Study Keisuke Suzuki1*, Masayuki Miyamoto2, Tomoyuki Miyamoto3, Yuichi Inoue4, Kentaro Matsui4, Shingo Nishida4, Kenichi Hayashida5, Akira Usui4, Yoichiro Ueki5, Masaki Nakamura4, Momoyo Murata6, Ayaka Numao1, Yuji Watanabe1, Shiho Suzuki1, Koichi Hirata1 1 Department of Neurology, Dokkyo Medical University, Tochigi, Japan, 2 School of Nursing, Dokkyo Medical University, Tochigi, Japan, 3 Department of Neurology, Dokkyo Medical University Koshigaya Hospital, Saitama, Japan, 4 Yoyogi Sleep Disorder Centre, Tokyo, Japan, 5 Sleep & Stress Clinic, Tokyo, Japan, 6 Kokubunji Sakura Clinic, Tochigi, Japan OPEN ACCESS * [email protected] Citation: Suzuki K, Miyamoto M, Miyamoto T, Inoue Y, Matsui K, Nishida S, et al. (2015) The Prevalence and Characteristics of Primary Headache and Dream-Enacting Behaviour in Japanese Patients with Abstract Narcolepsy or Idiopathic Hypersomnia: A Multi- Centre Cross-Sectional Study. PLoS ONE 10(9): e0139229. doi:10.1371/journal.pone.0139229 Background Editor: Oscar Arias-Carrion, Hospital General Dr. Because the prevalence and characteristics of primary headache have yet to be thoroughly Manuel Gea González, MEXICO studied in patients with hypersomnia disorders, including narcolepsy and idiopathic hyper- Received: March 25, 2015 somnia, we examined these parameters in the Japanese population. Accepted: September 10, 2015 Published: September 29, 2015 Methods Copyright: © 2015 Suzuki et al. This is an open In a multicentre cross-sectional survey, among 576 consecutive outpatients with sleep dis- access article distributed under the terms of the orders, 68 narcolepsy patients and 35 idiopathic hypersomnia patients were included.