Vitamin and Mineral Safety 3Rd Edition
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
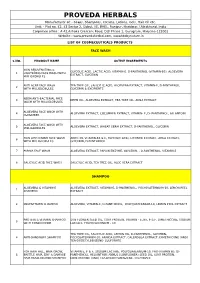
Cosmeceutical Products List
PROVEDA HERBALS Manufacturer of: - Soaps, Shampoos, Creams, Lotions, Gels, Hair Oil etc. Unit: - Plot no. 42, 43 Sector 2, Sidcul, IIE, BHEL, Ranipur, Haridwar, Uttrakhand, India Corporate office : A 42,Ashoka Crescent Road, DLF Phase 1, Gurugram, Haryana-122002 Website : www.provedaherbal.com, www.tbcbynature.in LIST OF COSMECEUTICALS PRODUCTS FACE WASH S.NO. PRODUCT NAME ACTIVE INGREDIENTS SKIN REJUVENATING & GLYCOLIC ACID, LACTIC ACID, VITAMIN-E, D-PANTHENOL (VITAMIN-B5), ALOEVERA 1 LIGHTENING FACE WASH WITH EXTRACT, GLYCERIN MILLIGLOBULES ANTI ACNE FACE WASH TEA TREE OIL, SALICYLIC ACID, ALOEVERA EXTRACT, VITAMIN-E, D-PANTHENOL, 2 WITH MILLIGLOBULES GLYCERIN & EXCIPIENTS NEEM ANTI-BACTERIAL FACE 3 NEEM OIL, ALOEVERA EXTRACT, TEA TREE OIL, AMLA EXTRACT WASH WITH MILLIGLOBULES ALOEVERA FACE WASH WITH 4 ALOEVERA EXTRACT, CUCUMBER EXTRACT, VITAMIN- E, D- PANTHENOL, ALLANTOIN CUCUMBER ALOEVERA FACE WASH WITH 5 ALOEVERA EXTRACT, WHEAT GERM EXTRACT, D-PANTHENOL, GLYCERIN MILLIGLOBULES SKIN LIGHTENING FACE WASH ARBUTIN, VITAMIN-B3 & E, GLYCOLIC ACID, LICORICE EXTRACT, AMLA EXTRACT, 6 WITH MILLIGLOBULES GLYCERIN, D-PANTHENOL 7 PAPAYA FACE WASH ALOEVERA EXTRACT, PAPAIN ENZYME, GLYCERIN, , D-PANTHENOL, VITAMIN-E 8 SALICYLIC ACID FACE WASH SALICYLIC ACID, TEA TREE OIL, ALOE VERA EXTRACT SHAMPOO ALOEVERA & VITAMIN-E ALOEVERA EXTRACT, VITAMIN-E, D-PANTHENOL, POLYQUATERNIUM-10, LEMON PEEL 1 SHAMPOO EXTRACT 2 MULTIVITAMIN SHAMPOO ALOEVERA, VITAMIN-E, D-PANTHENOL, POLYQUATERNIUM-10, LEMON PEEL EXTRACT PROTEIN & VITAMIN SHAMPOO SUN FLOWER SEED OIL, -

Inline-Supplementary-Material-1.Pdf
Appendix 1: STOPP/START criteria version 2 applied to the TRUST dataset Physiological system Criteria Criteria included Number (%) (The relevant () criteria for each participant were applied to the dataset and recorded in of Microsoft Office Excel ® (2013)) criteria included out of total criteria STOPP criteria Indication of medication A1. Any drug prescribed without an evidence-based clinical indication. X 1/3 (33.3) A2. Any drug prescribed beyond the recommended duration, where treatment duration is X well defined. A3. Any duplicate drug class prescription e.g. two concurrent NSAIDs, SSRIs, loop diuretics, ACE inhibitors, anticoagulants (optimisation of monotherapy within a single drug class should be observed prior to considering a new agent). Cardiovascular system B1. Digoxin for heart failure with preserved systolic ventricular function (no clear evidence X 7/13 (53.8) of benefit). B2. Verapamil or diltiazem with NYHA Class III or IV heart failure (may worsen heart failure). B3. Beta-blocker in combination with verapamil or diltiazem (risk of heart block). B4. Beta blocker with symptomatic bradycardia (< 50/min), type II heart block or complete heart block (risk of profound hypotension, asystole). B5. Amiodarone as first-line antiarrhythmic therapy in supraventricular tachyarrhythmias X (higher risk of side-effects than beta-blockers, digoxin, verapamil or diltiazem). B6. Loop diuretic as first-line treatment for hypertension (safer, more effective alternatives available). B7. Loop diuretic for dependent ankle oedema without clinical, biochemical evidence or radiological evidence of heart failure, liver failure, nephrotic syndrome or renal failure (leg elevation and /or compression hosiery usually more appropriate). B8. Thiazide diuretic with current significant hypokalaemia (i.e. -

Bartges – REACTIONS by CONSUMERS – ADVERSE FOOD
REACTIONS B Y C O N S U M E R S - A D V E R S E F O O D R E A C T I O N S Joe Bartges, DVM, PhD, DACVIM, DACVN* Claudia Kirk, DVM, PhD, DACVIM, DACVN, Susan Lauten, PhD, Angela Lusby, DVM, Beth Hamper, DVM, Susan Wynn, DVM Veterinary Nutrition Center, Knoxville, IN 1. Introduction A. Although providing nutrition to companion animals should be relatively easy and safe, occasionally you will encounter situations where an adverse reaction to a diet or nutrient or exposure to a food hazard occurs 2. Food components. A. Hazardous food components encompass dietary components that are present in the food. These may be components that should be present, but are present in an unbalanced manner, or components that should not be present. B. Nutrient imbalances may occur when there is a problem in the formulation or manufacture of a diet, or if the owner supplements a complete and balanced diet with an incomplete and unbalanced food or supplements. a. Excesses (1) Hypervitaminosis A is uncommonly seen, but results in ankylosing spondylosis particularly of the cervical vertebrae in cats. Excessive vitamin A is supplemented to a cat in the form of raw liver or cod liver oil because liver contains high levels of fat-soluble vitamins. (2) Hypervitaminosis D also occurs uncommonly, but may occur with supplemental vitamin D. More commonly, hypervitaminosis D occurs due to ingestion of vitamin D containing rodenticides and causes an acute disease manifested as hypercalcemia, polyuria/polydipsia, muscle fasciculations, vomiting, diarrhea, anorexia, seizures, and possibly renal failure. -

Choline for a Healthy Pregnancy
To support healthy for a Healthy weight gain and keep up with the nutritional needs of both mom and Pregnancy the developing baby, CHOLINE additional nutrients are necessary. Nine out of 10 Americans don’t meet the daily recommended choline intake of 550 mg1,2 and it can be challenging to reach this goal even when choosing choline-containing foods like beef, eggs, wheat germ and Brussels sprouts. Choline is particularly important during pregnancy for both mom and baby because it supports healthy brain growth and offers protection against neural tube defects. Women are encouraged to take a prenatal supplement before and during pregnancy to ensure they’re meeting vitamin and mineral recommendations. In fact, the American Medical Association recommends that choline be included in all prenatal vitamins to help ensure women get enough choline to maintain a normal pregnancy.3 Look for a prenatal supplement that contains folic acid, iron, DHA (omega-3s), vitamin D and choline. Consider smart swaps to get the most choline in your diet for a healthy pregnancy, as well as optimal health after baby arrives. PREGNANCY EATING PATTERN* CHOLINE-FOCUSED PREGNANCY EATING PATTERN* 1 1 hard-cooked egg 1 2 cups toasted whole grain oat cereal / 1 large peach 1 cup nonfat milk 1 1 slice whole grain bread /3 cup blueberries 1 1 tablespoon jelly /3 cup sliced banana BREAKFAST 1 cup nonfat milk 1 /2 whole grain bagel 1 whole wheat tortilla 2 tablespoons peanut butter 2 tablespoons peanut butter 1 small apple 1 SNACK 1 /2 large banana /2 cup nonfat vanilla Greek yogurt 2 slices whole grain bread 3 oz. -

Is There an Ideal Diet to Protect Against Iodine Deficiency?
nutrients Review Is There an Ideal Diet to Protect against Iodine Deficiency? Iwona Krela-Ka´zmierczak 1,† , Agata Czarnywojtek 2,3,†, Kinga Skoracka 1,* , Anna Maria Rychter 1 , Alicja Ewa Ratajczak 1 , Aleksandra Szymczak-Tomczak 1, Marek Ruchała 2 and Agnieszka Dobrowolska 1 1 Department of Gastroenterology, Dietetics and Internal Diseases, Poznan University of Medical Sciences, Heliodor Swiecicki Hospital, 60-355 Poznan, Poland; [email protected] (I.K.-K.); [email protected] (A.M.R.); [email protected] (A.E.R.); [email protected] (A.S.-T.); [email protected] (A.D.) 2 Department of Endocrinology, Metabolism and Internal Medicine, Poznan University of Medical Sciences, 60-355 Poznan, Poland; [email protected] (A.C.); [email protected] (M.R.) 3 Department of Pharmacology, Poznan University of Medical Sciences, 60-806 Poznan, Poland * Correspondence: [email protected]; Tel.: +48-665-557-356 or +48-8691-343; Fax: +48-8691-686 † These authors contributed equally to this work. Abstract: Iodine deficiency is a global issue and affects around 2 billion people worldwide, with preg- nant women as a high-risk group. Iodine-deficiency prevention began in the 20th century and started with global salt iodination programmes, which aimed to improve the iodine intake status globally. Although it resulted in the effective eradication of the endemic goitre, it seems that salt iodination did not resolve all the issues. Currently, it is recommended to limit the consumption of salt, which is the main source of iodine, as a preventive measure of non-communicable diseases, such as hypertension or cancer the prevalence of which is increasing. -

Raynaud's Phenomenon and the Possible Use of Foods
JFS R: Concise Reviews/Hypotheses in Food Science Raynaud’s Phenomenon and the Possible Use of Foods CHRIS I. WRIGHT, CHRISTINE I. KRONER, AND RICHARD DRAIJER R: Concise Reviews in Food Science ABSTRACT: In this article we focus on the possible use of foods to alleviate Raynaud’s phenomenon (RP). RP is evoked, predominately, by cold and results in a potent vascular constriction of the microvascular blood vessels in the hands, thus leading to reduced hand blood flow and the elevation of pain sensation. To alleviate RP by diet, food components need to be able to promote hand skin blood flow, which may be achieved using fish oil, garlic, ginkgo biloba, L-carnitine, or inositol nicotinate, or to increase hand skin temperature, using evening primrose oil, ginkgo biloba, or inositol nicotinate. Although there are a number of studies documenting such improvements with these ingredients, they often are poorly designed. Hence, there is a need for more controlled studies to substantiate their use, but also to test alternative foods or target new ones. Therefore, we also discuss some alternate food options and briefly outline clinical drugs for the treatment of RP, as their mechanisms of action may also be possible targets for food. It is the intention of this article to address the research needs of this field and to provide a better understanding of alternative options for those with RP. Keywords: Raynaud’s, vascular constriction, dietary intervention, nutraceutical, functional foods Introduction Mahoney 1999; Generini and others 2003; Herrick 2003); however, lit- here are a growing number of studies focusing on the con- tle work has been published on the use of foods as a complementary Tceivable health benefits of foods, botanicals, and supplements treatment for RP patients or as a safeguard for those at high or future (Boelsma and others 2001; Green and others 2003). -
Zinc Citrate – a Highly Bioavailable Zinc Source
Wellness Foods Europe THE MAGAZINE FOR NUTRITION, FUNCTIONAL FOODS & BEVERAGES AND SUPPLEMENTS Zinc citrate – a highly bioavailable zinc source Reprint from Wellness Foods Europe issue 3/2014 Wellness Foods Europe Special salts Zinc citrate – a highly bioavailable zinc source Markus Gerhart, Jungbunzlauer Ladenburg GmbH Zinc, the versatile mineral, is about to be- Zinc is a component of about 300 enzymes and come the next star in the minerals catego- 2000 transcriptional factors, and 10 % of the ry. Profiting from its various health benefits human proteome contain zinc-binding motives. and its relatively low cost in use, zinc sales Impairment of intestinal zinc absorption results in supplements have shown a double digit in severe clinical manifestations like skin lesions, growth in 2012 and are starting to catch up developmental retardation, stunted growth and with calcium, magnesium and iron, the cate- immune deficiency. gory leaders. Its importance for human health was empha- sised by the European health claim regu lation, Zinc is an essential transition metal that is where zinc received more positive opinions (18 directly or indirectly involved in a wide varie- in total) than any other mineral. The range of ty of physiological processes. After discover- claims (Table 1) includes, amongst others, im- ing the necessity of zinc for Aspergillus niger, it portant health benefits like immunity, bone took another 100 years before its relevance for health, cognitive function and healthy vision. humans was recognised, when the zinc deficien- These health benefits can be clearly defined and cy syndrome was described for the first time by are easy for the consumer to understand. -

Poisons and Narcotic Drugs (Amendment) Ordinance 1988
AUSTRALIAN CAPITAL TERRITORY Poisons and Narcotic Drugs (Amendment) Ordinance 1988 No. 96 of 1988 I, THE GOVERNOR-GENERAL of the Commonwealth of Australia, acting with the advice of the Federal Executive Council, hereby make the following Ordinance under the Seat of Government (Administration) Act 1910. Dated 15 December 1988 N. M. STEPHEN Governor-General By His Excellency’s Command, CLYDE HOLDING Minister of State for the Arts and Territories An Ordinance to amend the Poisons and Narcotic Drugs Ordinance 1978 Short title 1. This Ordinance may be cited as the Poisons and Narcotic Drugs (Amendment) Ordinance 1988.1 Commencement 2. This Ordinance commences on such date as is fixed by the Minister by notice in the Gazette. Principal Ordinance 3. In this Ordinance, “Principal Ordinance” means the Poisons and Narcotic Drugs Ordinance 1978.2 (Ord. 79/88)—Cat. No. Authorised by the ACT Parliamentary Counsel—also accessible at www.legislation.act.gov.au 2 Poisons and Narcotic Drugs (Amendment) No. 96, 1988 Substances to which Division applies 4. Section 27B of the Principal Ordinance is amended by adding at the end the following paragraphs: “; (f) follicle stimulating hormone; (g) luteinising hormone; (h) thalidomide.”. Grant of authorisation 5. Section 27E of the Principal Ordinance is amended— (a) by omitting from paragraph (1) (a) “or cyclofenil” and substituting “, cyclofenil, follicle stimulating hormone or luteinising hormone”; (b) by omitting from paragraph (1) (b) “and”; and (c) by adding at the end of subsection (1) the following word and paragraph: “; and (d) in the case of an application that relates to thalidomide— the applicant is a specialist physician with no less than 5 years’ experience in the treatment of erythema nodosum leprosum.”. -
Cellular Uptake and Toxicological Effects of Differently Sized Zinc Oxide Nanoparticles in Intestinal Cells †
toxics Article Cellular Uptake and Toxicological Effects of Differently Sized Zinc Oxide Nanoparticles in Intestinal Cells † Anna Mittag 1,* , Christian Hoera 2, Alexander Kämpfe 2 , Martin Westermann 3, Jochen Kuckelkorn 4, Thomas Schneider 1 and Michael Glei 1 1 Department of Nutritional Toxicology, Institute of Nutritional Sciences, Friedrich Schiller University Jena, Dornburger Straße 24, 07743 Jena, Germany; [email protected] (T.S.); [email protected] (M.G.) 2 German Environment Agency, Swimming Pool Water, Chemical Analytics, Heinrich-Heine-Straße 12, 08645 Bad Elster, Germany; [email protected] (C.H.); [email protected] (A.K.) 3 Electron Microscopy Centre, Friedrich Schiller University Jena, Ziegelmühlenweg 1, 07743 Jena, Germany; [email protected] 4 German Environment Agency, Toxicology of Drinking Water and Swimming Pool Water, Heinrich-Heine-Straße 12, 08645 Bad Elster, Germany; [email protected] * Correspondence: [email protected] † In respectful memory of Dr. Tamara Grummt. Abstract: Due to their beneficial properties, the use of zinc oxide nanoparticles (ZnO NP) is constantly increasing, especially in consumer-related areas, such as food packaging and food additives, which is leading to an increased oral uptake of ZnO NP. Consequently, the aim of our study was to investigate the cellular uptake of two differently sized ZnO NP (<50 nm and <100 nm; 12–1229 µmol/L) using two human intestinal cell lines (Caco-2 and LT97) and to examine the possible resulting toxic effects. ZnO NP (<50 nm and <100 nm) were internalized by both cell lines and led to intracellular changes. Citation: Mittag, A.; Hoera, C.; Kämpfe, A.; Westermann, M.; Both ZnO NP caused time- and dose-dependent cytotoxic effects, especially at concentrations of Kuckelkorn, J.; Schneider, T.; Glei, M. -

Vitamin and Mineral Requirements in Human Nutrition
P000i-00xx 3/12/05 8:54 PM Page i Vitamin and mineral requirements in human nutrition Second edition VITPR 3/12/05 16:50 Page ii WHO Library Cataloguing-in-Publication Data Joint FAO/WHO Expert Consultation on Human Vitamin and Mineral Requirements (1998 : Bangkok, Thailand). Vitamin and mineral requirements in human nutrition : report of a joint FAO/WHO expert consultation, Bangkok, Thailand, 21–30 September 1998. 1.Vitamins — standards 2.Micronutrients — standards 3.Trace elements — standards 4.Deficiency diseases — diet therapy 5.Nutritional requirements I.Title. ISBN 92 4 154612 3 (LC/NLM Classification: QU 145) © World Health Organization and Food and Agriculture Organization of the United Nations 2004 All rights reserved. Publications of the World Health Organization can be obtained from Market- ing and Dissemination, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel: +41 22 791 2476; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permis- sion to reproduce or translate WHO publications — whether for sale or for noncommercial distri- bution — should be addressed to Publications, at the above address (fax: +41 22 791 4806; e-mail: [email protected]), or to Chief, Publishing and Multimedia Service, Information Division, Food and Agriculture Organization of the United Nations, 00100 Rome, Italy. The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization and the Food and Agriculture Organization of the United Nations concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. -

Zinc and Manganese Inhibition of Biological Hematite Reduction
ENVIRONMENTAL ENGINEERING SCIENCE Volume 23, Number 5, 2006 © Mary Ann Liebert, Inc. Zinc and Manganese Inhibition of Biological Hematite Reduction James J. Stone,1* William D. Burgos,2 Richard A. Royer,3 and Brian A. Dempsey2 1Department of Civil and Environmental Engineering Rapid City, SD 57701 2Department of Civil and Environmental Engineering The Pennsylvania State University University Park, PA 16802 3Environmental Technology Laboratory General Electric Company Niskayuna, NY 12309 ABSTRACT The effects of zinc and manganese on the reductive dissolution of hematite by the dissimilatory metal-re- ducing bacterium (DMRB) Shewanella putrefaciens CN32 were studied in batch culture. Experiments Ϫ1 were conducted with hematite (2.0 g L ) in 10 mM PIPES (pH 6.8), and H2 as the electron donor un- der nongrowth conditions (108 cell mLϪ1), spiked with zinc (0.02–0.23 mM) or manganese (0.02–1.8 mM) and incubated for 5 days. Zinc inhibition was calculated based on the 5-day extent of hematite biore- duction in the absence and presence of zinc. Zinc inhibition of hematite bioreduction increased with an- thraquinone-2,6-disulfonate (AQDS), a soluble electron shuttling agent, and ferrozine, a strong Fe(II) com- plexant. Both amendments would otherwise stimulate hematite bioreduction. These amendments did not significantly increase zinc sorption, but may have increased zinc toxicity by some unknown mechanism. At equal total Me(II) concentrations, zinc inhibited hematite reduction more than manganese and caused greater cell death. At equal sorbed Me(II) concentrations, manganese inhibited hematite reduction more than zinc and caused greater cell death. Results support the interpretation that Me(II) toxicity was more important than Me(II) sorption/surface blockage in inhibiting hematite reduction. -

Estimation of Elemental Concentrations of Ethiopia Coffee Arabica on Different Coffee Bean Varieties (Subspecies) Using Energy Dispersive X-Ray Florescence
International Journal of Scientific & Engineering Research Volume 9, Issue 4, April-2018 149 ISSN 2229-5518 Estimation of elemental concentrations of Ethiopia Coffee Arabica on different coffee bean Varieties (Subspecies) Using Energy Dispersive X-ray Florescence H. Masresha Feleke1*, Srinivasulu A1, K. Surendra1, B. Aruna1, Jaganmoy Biswas2, M. Sudershan2, A. D. P. Rao1, P. V. Lakshmi Narayana1 1. Dept. of Nuclear Physics, Andhra University, Visakhapatnam -530003, INDIA. 2. UGC-DAE Consortium for Scientific Research, Trace element lab, Salt Lake, Kolkata 700 098, India Abstract: Using Energy Dispersive X-ray Florescence (EDXRF) Elemental analysis, Coffee cherry of Arabica subspecies produced in crop years of 2015/2016 in nine different parts of coffee growing Area in Ethiopa were analyzed and has been found four major elements P, K, Ca, S and eight minor elements Mn, Fe, Cu, Zn, Se, Sr, Rb, Br from Twenty coffee Arabica subspecies. The Samples were washed; dried; Grinding with mortar and finally pelletized. EDXRF analysis were carried the energies of the X-rays emitted by the sample are measured using a Si- semiconductor detector and are processed by a pulse height analyzer. Computer analysis of this data yields an energy spectrum which defines the elemental composition of the sample. The system detection calibration and accuracy check was performed through different countries reported values and analysis of NIST certified reference materials SRM 1515 (Apple leaves). Most of coffee beans sample were found to be a good agreements towards NIST standards and different countries reported values. Meanwhile discussed the elemental concentration and their biological effects on human physiology. Keywords: Coffee Cherry,IJSER Subspecies coffee, Elemental Concentration and EDXRF 1.