Protracted Bacterial Bronchitis (PBB) in Children
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Caring for Children with Special Needs ALLERGIES and ASTHMA
caring for children with special needs ALLERGIES AND ASTHMA We don’t usually think of children with allergies or asthma as children with “special needs,” but they certainly are. In fact, children with these conditions are probably the most frequently encountered “special needs” children. Child care providers can do a great deal to help individual children manage their specific allergy or asthma needs and feel more comfortable in a child care setting. Allergies wastes. Every house has them, no matter how clean. Other inhaled Children with allergies face the allergens include mold, pollen (hay same social difficulties as do adults, fever), animal dander (especially but they have less maturity and from cats), chemicals, and per emotional resources to deal with fumes. them. Children find that they cannot eat what their friends eat or The most common allergy symp cannot play outside during some toms are seasons. Until a child is mature � a clear, runny nose and enough to understand why she sneezing, cannot do something, you must be � itchy or stuffed-up nose or careful to help the child through the itchy, runny eyes, and difficulties. Start teaching a child early on about what he is allergic to; � asthma (remember that not all you will not always be able to people with asthma have monitor everything. allergies and not all allergies Some foods can cause a life cause or develop into asthma). threatening reaction. The mouth, throat, and bronchial tubes swell enough to interfere with breathing. Strategies for inclusion The person may wheeze or faint. Some parents have found that by Often there are generalized hives volunteering to bring food to and/or a swollen face. -

Allergic Bronchopulmonary Aspergillosis Revealing Asthma
CASE REPORT published: 22 June 2021 doi: 10.3389/fimmu.2021.695954 Case Report: Allergic Bronchopulmonary Aspergillosis Revealing Asthma Houda Snen 1,2*, Aicha Kallel 2,3*, Hana Blibech 1,2, Sana Jemel 2,3, Nozha Ben Salah 1,2, Sonia Marouen 3, Nadia Mehiri 1,2, Slah Belhaj 3, Bechir Louzir 1,2 and Kalthoum Kallel 2,3 1 Pulmonary Department, Hospital Mongi Slim, La Marsa, Tunisia, 2 Faculty of Medicine, Tunis El Manar University, Tunis, Tunisia, 3 Parasitology and Mycology Department, La Rabta Hospital, Tunis, Tunisia Allergic bronchopulmonary aspergillosis (ABPA) is an immunological pulmonary disorder caused by hypersensitivity to Aspergillus which colonizes the airways of patients with asthma and cystic fibrosis. Its diagnosis could be difficult in some cases due to atypical Edited by: presentations especially when there is no medical history of asthma. Treatment of ABPA is Brian Stephen Eley, frequently associated to side effects but cumulated drug toxicity due to different molecules University of Cape Town, South Africa is rarely reported. An accurate choice among the different available molecules and Reviewed by: effective on ABPA is crucial. We report a case of ABPA in a woman without a known Shivank Singh, Southern Medical University, China history of asthma. She presented an acute bronchitis with wheezing dyspnea leading to an Richard B. Moss, acute respiratory failure. She was hospitalized in the intensive care unit. The Stanford University, United States bronchoscopy revealed a complete obstruction of the left primary bronchus by a sticky *Correspondence: Houda Snen greenish material. The culture of this material isolated Aspergillus fumigatus and that of [email protected] bronchial aspiration fluid isolated Pseudomonas aeruginosa. -

Symptoms Related to Asthma and Chronic Bronchitis in Three Areas of Sweden
Eur Respir J, 1994, 7, 2146–2153 Copyright ERS Journals Ltd 1994 DOI: 10.1183/09031936.94.07122146 European Respiratory Journal Printed in UK - all rights reserved ISSN 0903 - 1936 Symptoms related to asthma and chronic bronchitis in three areas of Sweden E. Björnsson*, P. Plaschke**, E. Norrman+, C. Janson*, B. Lundbäck+, A. Rosenhall+, N. Lindholm**, L. Rosenhall+, E. Berglund++, G. Boman* Symptoms related to asthma and chronic bronchitis in three areas of Sweden. E. Björnsson, *Dept of Lung Medicine and Asthma P. Plaschke, E. Norrman, C. Janson, B. Lundbäck, A. Rosenhall, N. Lindholm, L. Research Center, Akademiska sjukhu- Rosenhall, E. Berglund, G. Boman. ERS Journals Ltd 1994. set, Uppsala University, Uppsala, Sweden. ABSTRACT: Does the prevalence of respiratory symptoms differ between regions? **Asthma and Allergy Research Center, Sahlgren's Hospital, University of Göteborg, As a part of the European Community Respiratory Health Survey, we present data Göteborg, Sweden. +Dept of Pulmonary from an international questionnaire on asthma symptoms occurring during a 12 Medicine and Allergology, Univer- month period, smoking and symptoms of chronic bronchitis. The questionnaire was sity Hospital of Northern Sweden, Umeå, mailed to 10,800 persons aged 20–44 yrs living in three regions of Sweden (Västerbotten, Sweden. ++Dept of Pulmonary Medicine, Uppsala and Göteborg) with different environmental characteristics. The total Sahlgrenska University Hospital, Göteborg, response rate was 86%. Sweden. Wheezing was reported by 20.5%, and the combination of wheezing without a Correspondence: E. Björnsson, Dept of cold and wheezing with breathlessness by 7.4%. The use of asthma medication was Lung Medicine, Akademiska sjukhuset, S- reported by 5.3%. -

Laryngopharyngeal Reflux and Chronic Cough Disclosure
Brett MacFarlane Laryngopharyngeal reflux and chronic cough A therapeutic dilemma 1 Disclosure I have received honoraria, speaker fees, consultancy fees, travel support, am a member of advisory boards or have appeared on expert panels for: Reckitt Benkiser, Bayer, Blackmores Produce education material for AJP, Retail Pharmacy, ITK, ACP 2 Disclaimer The information contained herein has not been independently verified, confirmed, reviewed or endorsed by Reckitt Benckiser. No consideration, in any form, has been provided or promised by Reckitt Benckiser in connection with or arising out of this presentation, and all findings are based on my own independent research, experience and expert opinion. The information contained herein is for guidance only and pharmacists are encouraged to conduct their own enquiries. No representation warranty, express or implied, is made as to the accuracy, reliability or correctness of the information contained herein and all liability is disclaimed arising out of or in connection with any reliance on this presentation or the information contained herein. 3 Learning objectives After completing this activity, pharmacists should be able to: 1. Describe laryngopharyngeal reflux (LPR) and how it relates to chronic cough 2. Describe the challenges of diagnosing LPR 3. Outline the management of LPR 4 What does reflux mean to you? Heartburn Acid Burning Rising into the oesophagus 5 What does chronic cough mean to you? Respiratory Asthma COPD Infection Smoking Cancer 6 Reflux is more than just acid Refluxate also contains: Pepsin (stomach) Trypsin (duodenum) Bile salts 7 Causes of chronic cough 29% asthma 33% reflux Li X, et al. Gastroesophageal Reflux Disease and Chronic Cough: A Possible Mechanism Elucidated by Ambulatory pH‐impedance‐pressure Monitoring. -

GERD and Coughing, What PIDD Patients Need to Know
By Dharshini Mahadevan, MPH While the cause of GERD is not or many with primary immune deficiency disease (PIDD), a chronic cough is nothing new. According to Annette known, the symptoms and what F Zampelli, MSN, CRNP, a medical science liaison for CSL they trigger in PIDD patients can Behring, as well as a former clinician in the Pediatric, Allergy and Immunology Department at Penn State Children’s Hospital, a often be controlled with lifestyle potential culprit of their cough—gastroesophageal reflux disease and dietary changes. (GERD)—is often overlooked. “A lot of people think they’re just having sinus drainage,” said Zampelli, who also suffers from GERD, as well as common variable immune deficiency (CVID). “Or, they may blame coughing on asthma.” Because Zampelli deals with GERD herself, she can often immediately recognize it in others. She recalls one incident during which she realized an individual was refluxing within minutes of meeting her. “A lot of people have chronic hoarseness and intermittent coughing because GERD can cause a laryngeal spasm,” explains Zampelli. “It also causes inflammation of the vocal While the exact cause of cords, which causes them to spasm and leads to irritation to the surrounding tissues.” GERD remains unknown, To determine whether GERD is a factor in one’s cough, Zampelli recommends that patients pay attention to whether many believe hiatal hernias they wake up with morning hoarseness, if they seem to cough more after they lie down or if certain foods make their are a main cause. symptoms worse. In addition, Zampelli suggests that patients track symptoms by using “a food diary to see if there’s any correlation with certain things. -
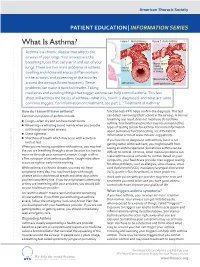
What Is Asthma? Figure 1
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES What Is Asthma? Figure 1. Normal Airway Figure 2. Acute Asthma Asthma is a chronic disease that affects the airways of your lungs. Your airways are the breathing tubes that carry air in and out of your Muscle spasm causing lungs. There are two main problems in asthma: relaxed narrowing muscles swelling and increased mucus (inflammation) of airways in the airways, and squeezing of the muscles Mucus build up around the airways (bronchospasm). These open airways Swelling/inammation problems can make it hard to breathe. Taking medicines and avoiding things that trigger asthma can help control asthma. This fact sheet will address the basics of asthma—what it is, how it is diagnosed, and what are some common triggers. For information on treatment, see part 2, “Treatment of Asthma”. How do I know if I have asthma? function test–PFT) helps confirm the diagnosis. This test Common symptoms of asthma include: can detect narrowing (obstruction) in the airways. A normal breathing test result does not mean you do not have ■ Cough—often dry and can have harsh bursts asthma. Your healthcare provider may recommend other ■ Wheezing—a whistling sound mainly when you breathe types of testing to look for asthma. For more information out through narrowed airways about pulmonary function testing, see ATS Patient ■ Chest tightness Information series at www.thoracic.org/patients. ■ Shortness of breath which may occur with activity or If you have been diagnosed with asthma, but it is not even at rest getting better with treatment, you might benefit from When you are having a problem with asthma, you may feel CLIP AND COPY AND CLIP seeing an asthma specialist. -

Acute (Serious) Bronchitis
Acute (serious) Bronchitis This is an infection of the air tubes that go down to your lungs. It often follows a cold or the flu. Most people do not need treatment for this. The infection normally goes away in 7-10 days. We make every effort to make sure the information is correct (right). However, we cannot be responsible for any actions as a result of using this information. Getting Acute Bronchitis How the lungs work Your lungs are like two large sponges filled with tubes. As you breathe in, you suck oxygen through your nose and mouth into a tube in your neck. Bacteria and viruses in the air can travel into your lungs. Normally, this does not cause a problem as your body kills the bacteria, or viruses. However, sometimes infection can get through. If you smoke or if you have had another illness, infections are more likely to get through. Acute Bronchitis Acute bronchitis is when the large airways (breathing tubes) to the lungs get inflamed (swollen and sore). The infection makes the airways swell and you get a build up of phlegm (thick mucus). Coughing is a way of getting the phlegm out of your airways. The cough can sometimes last for up to 3 weeks. Acute Bronchitis usually goes away on its own and does not need treatment. We make every effort to make sure the information is correct (right). However, we cannot be responsible for any actions as a result of using this information. Symptoms (feelings that show you may have the illness) Symptoms of Acute Bronchitis include: • A chesty cough • Coughing up mucus, which is usually yellow, or green • Breathlessness when doing more energetic activities • Wheeziness • Dry mouth • High temperature • Headache • Loss of appetite The cough usually lasts between 7-10 days. -

Allergic Bronchopulmonary Aspergillosis and Severe Asthma with Fungal Sensitisation
Allergic Bronchopulmonary Aspergillosis and Severe Asthma with Fungal Sensitisation Dr Rohit Bazaz National Aspergillosis Centre, UK Manchester University NHS Foundation Trust/University of Manchester ~ ABPA -a41'1 Severe asthma wl'th funga I Siens itisat i on Subacute IA Chronic pulmonary aspergillosjs Simp 1Ie a:spe rgmoma As r§i · bronchitis I ram une dysfu net Ion Lun· damage Immu11e hypce ractivitv Figure 1 In t@rarctfo n of Aspergillus Vliith host. ABP A, aHerg tc broncho pu~ mo na my as µe rgi ~fos lis; IA, i nvas we as ?@rgiH os 5. MANCHl·.'>I ER J:-\2 I Kosmidis, Denning . Thorax 2015;70:270–277. doi:10.1136/thoraxjnl-2014-206291 Allergic Fungal Airway Disease Phenotypes I[ Asthma AAFS SAFS ABPA-S AAFS-asthma associated with fu ngaIsensitization SAFS-severe asthma with funga l sensitization ABPA-S-seropositive a llergic bronchopulmonary aspergi ll osis AB PA-CB-all ergic bronchopulmonary aspergi ll osis with central bronchiectasis Agarwal R, CurrAlfergy Asthma Rep 2011;11:403 Woolnough K et a l, Curr Opin Pulm Med 2015;21:39 9 Stanford Lucile Packard ~ Children's. Health Children's. Hospital CJ Scanford l MEDICINE Stanford MANCHl·.'>I ER J:-\2 I Aspergi 11 us Sensitisation • Skin testing/specific lgE • Surface hydroph,obins - RodA • 30% of patients with asthma • 13% p.atients with COPD • 65% patients with CF MANCHl·.'>I ER J:-\2 I Alternar1a• ABPA •· .ABPA is an exagg·erated response ofthe imm1une system1 to AspergUlus • Com1pUcatio n of asthm1a and cystic f ibrosis (rarell·y TH2 driven COPD o r no identif ied p1 rior resp1 iratory d isease) • ABPA as a comp1 Ucation of asth ma affects around 2.5% of adullts. -

Obliterative Bronchiolitis, Cryptogenic Organising Pneumonitis and Bronchiolitis Obliterans Organizing Pneumonia: Three Names for Two Different Conditions
Eur Reaplr J EDITORIAL 1991, 4, 774-775 Obliterative bronchiolitis, cryptogenic organising pneumonitis and bronchiolitis obliterans organizing pneumonia: three names for two different conditions R.M. du Bois, O.M. Geddes Over the last five years, increasing confusion has has been applied to conditions in which airflow obstruc developed over the use of the terms "bronchiolitis tion is prominent and in which response to treatment is obliterans" and "bronchiolitis obliterans organizing poor. pneumonia". The confusion stems largely from the common use of the term "bronchiolitis obliterans" or "obliterative bronchiolitis" in the diagnostic labels applied "Cryptogenic organizing pneumonitis" or "bronchi· to two entities which are quite distinct clinically but which otitis obliterans organizing pneumonia" (BOOP) bear certain resemblances histologically. Cryptogenic organizing pneumonitis was first described by DAVISON et al. [7] in 1983. The clinical syndrome ObUterative bronchiolitis consisted of breathlessness, malaise, fever, high erythrocyte sedimentation rate (ESR), pneumonic In 1977, GEODES et al. [1] reported the case histories shadowing on chest radiograph with a restrictive of six patients whose clinical condition was characterized pulmonary function defect and low gas transfer coeffi by airways obliteration in association with rheumatoid cient. On histological examination of lung biopsy mate· arthritis. The striking clinical features were of rapidly rial, the typical and distinguishing feature was the progressive breathlessness and the fmding on examination presence of connective tissue within the alveoli, alveolar of a high-pitched mid-inspiratory squeak heard over the ducts and, occasionally, in respiratory bronchioles. This lung fields. Chest radiographs showed hyperinflated lungs connective tissue consisted of "loosely woven fibres of but were otherwise normal. -

Diseases of the Respiratory System (J00-J99) ICD-10-CM
Diseases of the Respiratory System (J00-J99) ICD-10-CM Coverage provided by Amerigroup Inc. This publication contains proprietary information. This material is for informational purposes only. Reference the Centers for Medicare and Medicaid Services (CMS) for more information on Risk Adjustment and the CMS-HCC Model. Redistribution or other use is strictly forbidden This publication is for informational purposes only and is not guaranteed to be without defect. Please reference the current version(s) of the ICD-10-CM codebook, CMS-HCC Risk Adjustment Model, and AHA Coding Clinic for complete code sets and official coding guidance. AGPCARE-0080-19 63321MUPENABS 10/05/16 Diseases of the respiratory system are located in chapter Intermittent asthma which is defined as less 10 of the ICD-10-CM code book; this chapter includes than or equal to two occurrences per week. conditions such as asthma, pneumonia, and chronic Persistent asthma which includes three levels obstructive pulmonary disease (COPD). of severity: Mild: more than two times per week Reporting respiratory conditions Moderate: daily and may restrict Codes for reporting diseases of the respiratory physical activity system in ICD-10-CM feature relatively minor Severe: throughout the day with changes from ICD-9-CM. Most of the changes recurrent severe attacks limiting the involve understanding the medical terminology that ability to breathe the more specific codes include, as well as, the new The fourth character indicates severity, and the general coding structure and rules. fifth identifies whether status asthmaticus or At the beginning of chapter 10 for “Diseases of exacerbation is present. the Respiratory System (J00-J99),” an instructional note states, “When a respiratory condition is Asthma ICD-10-CM description described as occurring in more than one site and Category J45 Asthma is not specifically indexed, it should be classified Includes: to the lower anatomic site.” For example, Allergic: tracheobronchitis is classified to bronchitis with Asthma code J40. -

To Honeycombing in Idiopathic Pulmonary Fibrosis
Piciucchi et al. BMC Pulmonary Medicine (2016) 16:87 DOI 10.1186/s12890-016-0245-x CORRESPONDENCE Open Access From “traction bronchiectasis” to honeycombing in idiopathic pulmonary fibrosis: A spectrum of bronchiolar remodeling also in radiology? Sara Piciucchi1*, Sara Tomassetti2, Claudia Ravaglia2, Christian Gurioli2, Carlo Gurioli2, Alessandra Dubini3, Angelo Carloni4, Marco Chilosi5, Thomas V Colby6 and Venerino Poletti2,7 Abstract Background: The diagnostic and prognostic impact of traction bronchiectasis on high resolution CT scan (HRCT) in patients suspected to have idiopathic pulmonary fibrosis (IPF) is increasing significantly. Main body: Recent data demonstrated that cysts in honeycombing areas are covered by epithelium expressing bronchiolar markers. In IPF bronchiolization is the final consequence of a variety of pathogenic events starting from alveolar stem cell exhaustion, and ending in a abnormal/dysplastic proliferation of bronchiolar epithelium. CT scan features of traction bronchiectasis and honeycombing should be interpreted under the light of these new pathogenetic and morphologic considerations. Short conclusion: We suggest that in IPF subjects traction bronchiectasis and honeycombing -now defined as distinct entities on HRCT scan- are actually diverse aspects of a continuous spectrum of lung remodeling. Keywords: Traction bronchiectasis, Honeycombing, Fibroblastic Foci, Bronchiolar dysplastic proliferation Background Mechanical stress may contribute to the subpleural Histologically, Usual Interstitial Pneumonia (UIP) is and usually basilar localization of UIP changes [10, 11]. characterized by a combination of “patchy fibrosis” and The final stage of this “bronchiolization” process cor- fibroblastic foci displaying a “patchwork pattern”. Disease responds radiologically to honeycombing, typically seen progression is characterized by the appearance of air- first in the subpleural regions of the lower lobes [2, 3]. -

Cough Hypersensitivity in Patients with Obstructive Sleep Apnea Hypopnea Syndrome
Sleep and Breathing (2019) 23:33–39 https://doi.org/10.1007/s11325-018-1641-7 SLEEP BREATHING PHYSIOLOGY AND DISORDERS • ORIGINAL ARTICLE Cough hypersensitivity in patients with obstructive sleep apnea hypopnea syndrome Cuiqin Shi1 & Siwei Liang1 & Xianghuai Xu1 & Qiang Chen1 & Lan Wang1 & Li Yu1 & Hanjing Lv 1 & Zhongmin Qiu1 Received: 24 May 2017 /Revised: 5 February 2018 /Accepted: 6 February 2018 /Published online: 16 February 2018 # Springer International Publishing AG, part of Springer Nature 2018 Abstract Purpose The purpose of this study was to investigate cough hypersensitivity and its potential mechanisms in patients with obstructive sleep apnea hypopnea syndrome (OSAHS). Methods Fifteen OSAHS patients, 12 simple snoring patients, and 15 healthy volunteers received cough sensitivity test and induced sputum cytology. Cough thresholds C2 and C5 (the minimum of capsaicin inducing ≥ 2and≥ 5 coughs, respectively), total cell count, cell differentials and the levels of bradykinin, histamine, prostaglandin E2, substance P, calcitonin gene-related peptide, pepsin, and interleukin-2 in the induced sputum detected by enzyme-linked immunosorbent assay were compared. The linear correlation between lgC2 and lgC5 and apnea hypopnea index, cell differentials, and inflammatory mediators in the induced sputum was calculated in OSAHS patients. Results OSAHS patients presented with a significant lower C2 and C5 (P < 0.01), increased lymphocyte but decreased macro- phage and neutrophil proportions in the induced sputum (P < 0.01), and higher contents of substance P, calcitonin gene-related peptide and interleukin-2 (P < 0.01) but similar levels of bradykinin, pepsin, prostaglandin E2, and histamine (P > 0.05) in the supernatant of induced sputum, when compared with simple snoring patients and healthy volunteers.