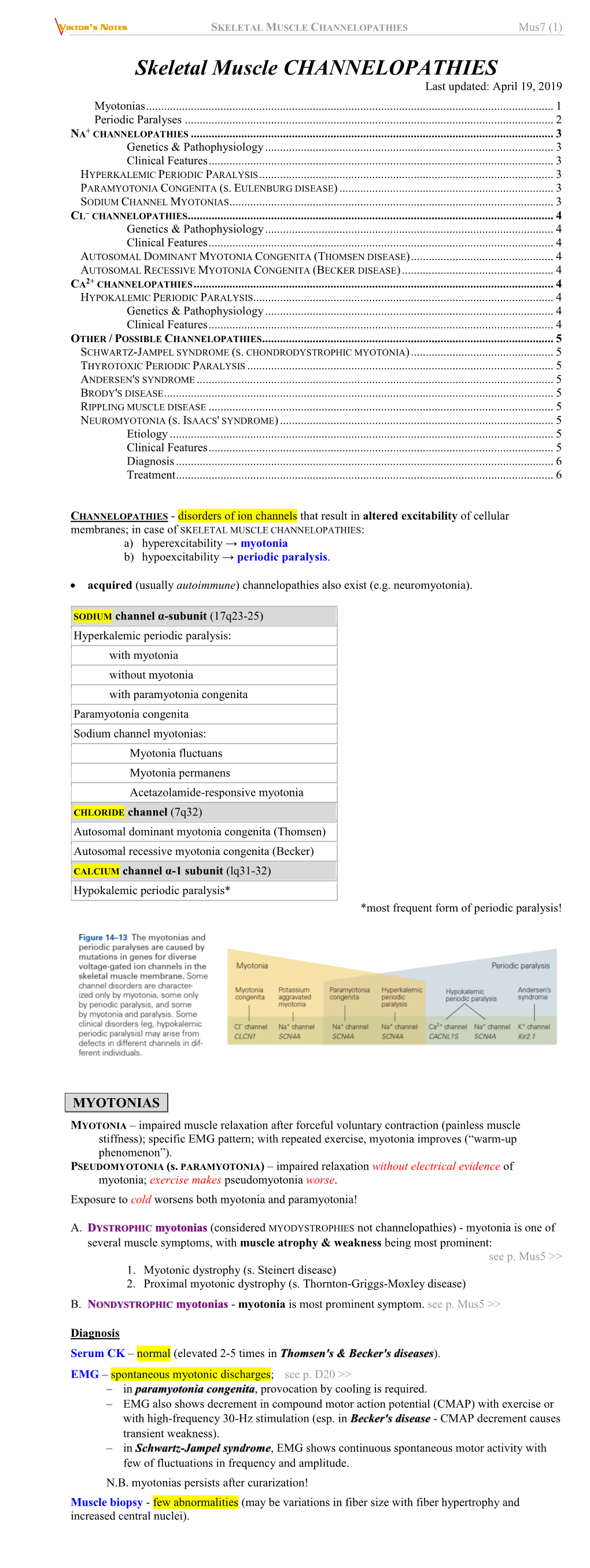
SKELETAL MUSCLE CHANNELOPATHIES Mus7 (1)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Spectrum of CLCN1 Mutations in Patients with Myotonia Congenita in Northern Scandinavia
European Journal of Human Genetics (2001) 9, 903 ± 909 ã 2001 Nature Publishing Group All rights reserved 1018-4813/01 $15.00 www.nature.com/ejhg ARTICLE Spectrum of CLCN1 mutations in patients with myotonia congenita in Northern Scandinavia Chen Sun*,1, Lisbeth Tranebjñrg*,1, Torberg Torbergsen2,GoÈsta Holmgren3 and Marijke Van Ghelue1,4 1Department of Medical Genetics, University Hospital of Tromsù, Tromsù, Norway; 2Department of Neurology, University Hospital of Tromsù, Tromsù, Norway; 3Department of Clinical Genetics, University Hospital of UmeaÊ, UmeaÊ,Sweden;4Department of Biochemistry, Section Molecular Biology, University of Tromsù, Tromsù, Norway Myotonia congenita is a non-dystrophic muscle disorder affecting the excitability of the skeletal muscle membrane. It can be inherited either as an autosomal dominant (Thomsen's myotonia) or an autosomal recessive (Becker's myotonia) trait. Both types are characterised by myotonia (muscle stiffness) and muscular hypertrophy, and are caused by mutations in the muscle chloride channel gene, CLCN1. At least 50 different CLCN1 mutations have been described worldwide, but in many studies only about half of the patients showed mutations in CLCN1. Limitations in the mutation detection methods and genetic heterogeneity might be explanations. In the current study, we sequenced the entire CLCN1 gene in 15 Northern Norwegian and three Northern Swedish MC families. Our data show a high prevalence of myotonia congenita in Northern Norway similar to Northern Finland, but with a much higher degree of mutation heterogeneity. In total, eight different mutations and three polymorphisms (T87T, D718D, and P727L) were detected. Three mutations (F287S, A331T, and 2284+5C4T) were novel while the others (IVS1+3A4T, 979G4A, F413C, A531V, and R894X) have been reported previously. -

Paramyotonia Congenita
Paramyotonia congenita Description Paramyotonia congenita is a disorder that affects muscles used for movement (skeletal muscles). Beginning in infancy or early childhood, people with this condition experience bouts of sustained muscle tensing (myotonia) that prevent muscles from relaxing normally. Myotonia causes muscle stiffness that typically appears after exercise and can be induced by muscle cooling. This stiffness chiefly affects muscles in the face, neck, arms, and hands, although it can also affect muscles used for breathing and muscles in the lower body. Unlike many other forms of myotonia, the muscle stiffness associated with paramyotonia congenita tends to worsen with repeated movements. Most people—even those without muscle disease—feel that their muscles do not work as well when they are cold. This effect is dramatic in people with paramyotonia congenita. Exposure to cold initially causes muscle stiffness in these individuals, and prolonged cold exposure leads to temporary episodes of mild to severe muscle weakness that may last for several hours at a time. Some older people with paramyotonia congenita develop permanent muscle weakness that can be disabling. Frequency Paramyotonia congenita is an uncommon disorder; it is estimated to affect fewer than 1 in 100,000 people. Causes Mutations in the SCN4A gene cause paramyotonia congenita. This gene provides instructions for making a protein that is critical for the normal function of skeletal muscle cells. For the body to move normally, skeletal muscles must tense (contract) and relax in a coordinated way. Muscle contractions are triggered by the flow of positively charged atoms (ions), including sodium, into skeletal muscle cells. The SCN4A protein forms channels that control the flow of sodium ions into these cells. -

Inherited Neuropathies
407 Inherited Neuropathies Vera Fridman, MD1 M. M. Reilly, MD, FRCP, FRCPI2 1 Department of Neurology, Neuromuscular Diagnostic Center, Address for correspondence Vera Fridman, MD, Neuromuscular Massachusetts General Hospital, Boston, Massachusetts Diagnostic Center, Massachusetts General Hospital, Boston, 2 MRC Centre for Neuromuscular Diseases, UCL Institute of Neurology Massachusetts, 165 Cambridge St. Boston, MA 02114 and The National Hospital for Neurology and Neurosurgery, Queen (e-mail: [email protected]). Square, London, United Kingdom Semin Neurol 2015;35:407–423. Abstract Hereditary neuropathies (HNs) are among the most common inherited neurologic Keywords disorders and are diverse both clinically and genetically. Recent genetic advances have ► hereditary contributed to a rapid expansion of identifiable causes of HN and have broadened the neuropathy phenotypic spectrum associated with many of the causative mutations. The underlying ► Charcot-Marie-Tooth molecular pathways of disease have also been better delineated, leading to the promise disease for potential treatments. This chapter reviews the clinical and biological aspects of the ► hereditary sensory common causes of HN and addresses the challenges of approaching the diagnostic and motor workup of these conditions in a rapidly evolving genetic landscape. neuropathy ► hereditary sensory and autonomic neuropathy Hereditary neuropathies (HN) are among the most common Select forms of HN also involve cranial nerves and respiratory inherited neurologic diseases, with a prevalence of 1 in 2,500 function. Nevertheless, in the majority of patients with HN individuals.1,2 They encompass a clinically heterogeneous set there is no shortening of life expectancy. of disorders and vary greatly in severity, spanning a spectrum Historically, hereditary neuropathies have been classified from mildly symptomatic forms to those resulting in severe based on the primary site of nerve pathology (myelin vs. -

Congenital Chloride Diarrhea in a Bartter Syndrome Misdiagnosed
Case Report iMedPub Journals Journal of Rare Disorders: Diagnosis & Therapy 2019 www.imedpub.com ISSN 2380-7245 Vol.5 No.2:4 DOI: 10.36648/2380-7245.5.2.196 Congenital Chloride Diarrhea in a Bartter Maria Helena Vaisbich*, Juliana Caires de Oliveira Syndrome Misdiagnosed Brazilian Patient Achili Ferreira, Ana Carola Hebbia Lobo Messa and Abstract Fernando Kok The differential diagnosis in children with hypokalemic hypochloremic alkalosis Department of Pediatric Nephrology, include a group of an inherited tubulopathies, such as Bartter Syndrome (BS) Instituto da Criança, University of São Paulo, and Gitelman Syndrome (GS). However, some of the clinically diagnosed São Paulo, Brasil patients present no pathogenic mutation in BS/GS known genes. Therefore, one can conclude that a similar clinical picture may be caused by PseudoBartter Syndrome (PBS) conditions. PBS include acquired renal problems (ex.: use of diuretics) as well as genetic or acquired extrarenal problems such as cystic *Corresponding author: fibrosis or cyclic vomiting, respectively. The accurate diagnosis of BS/GS needs Maria Helena Vaisbich a rational investigation. First step is to rule out PBS and confirm the primary renal tubular defect. However, it is not easy in some situations. In this sense, Department of Pediatric Nephrology, we reported a patient that was referred to our service with the diagnosis Instituto da Criança, University of São Paulo, of BS, but presented no mutation in BS/GS known genes. The whole-exome São Paulo, Brasil. sequencing detected a SCL26A3 likely pathogenic mutation leading to the final diagnosis of Congenital Chloride Diarrhea (CCD). Reviewing the records, the [email protected] authors noticed that liquid stools were mistaken for urine. -

Experiences of Rare Diseases: an Insight from Patients and Families
Experiences of Rare Diseases: An Insight from Patients and Families Unit 4D, Leroy House 436 Essex Road London N1 3QP tel: 02077043141 fax: 02073591447 [email protected] www.raredisease.org.uk By Lauren Limb, Stephen Nutt and Alev Sen - December 2010 Web and press design www.raredisease.org.uk WordsAndPeople.com About Rare Disease UK Rare Disease UK (RDUK) is the national alliance for people with rare diseases and all who support them. Our membership is open to all and includes patient organisations, clinicians, researchers, academics, industry and individuals with an interest in rare diseases. RDUK was established by Genetic RDUK is campaigning for a Alliance UK, the national charity strategy for integrated service of over 130 patient organisations delivery for rare diseases. This supporting all those affected by would coordinate: genetic conditions, in conjunction with other key stakeholders | Research in November 2008 following the European Commission’s | Prevention and diagnosis Communication on Rare Diseases: | Treatment and care Europe’s Challenges. | Information Subsequently RDUK successfully | Commissioning and planning campaigned for the adoption of the Council of the European into one cohesive strategy for all Union’s Recommendation on patients affected by rare disease in an action in the field of rare the UK. As well as securing better diseases. The Recommendation outcomes for patients, a strategy was adopted unanimously by each would enable the most effective Member State of the EU (including use of NHS resources. the -

Pseudo-Bartter Syndrome As the Initial Presentation of Cystic Fibrosis in Infants: a Paediatrics Section Paediatrics Series of Three Cases and Review of Literature
DOI: 10.7860/JCDR/2018/36189.11965 Case Series Pseudo-bartter Syndrome as the Initial Presentation of Cystic Fibrosis in Infants: A Paediatrics Section Paediatrics Series of Three cases and Review of Literature PRAWIN KUMAR1, NEERAJ GUPTA2, DAISY KHERA3, KULDEEP SINGH4 ABSTRACT Cystic Fibrosis (CF) is predominantly a disease of Caucasians, but it is increasingly being recognised in India. The typical presentations of CF are recurrent pneumonia and malabsorption. Atypical presentations are also increasingly being reported from India due to the differences in genotype and environmental factors. Pseudo-Bartter syndrome (PBS) is one of these atypical presentations which can present at any time after the diagnosis of CF but its presentation as an initial manifestation is rare. We hereby report three infants who presented with dehydration without obvious external losses. The investigations revealed metabolic alkalosis with hypochloraemia. A stepwise approach towards metabolic alkalosis revealed possibility of cystic fibrosis which was confirmed by sweat chloride test. All infants completely recovered with initial fluid and electrolyte therapy, following which supportive therapy for CF was started and subsequently they were discharged from the hospital. Keywords: Hypochloraemia, Metabolic alkalosis, Pseudo-Bartter Syndrome CASE SERIES sweat chloride test was not available at our centre so they were sent In this case series, we have described three infants in the age group to paediatric pulmonology division, AIIMS, New Delhi where sweat of 5-10 months from western Rajasthan, India, who presented with chloride test was performed (pilocarpine iontophoresis method), features of dehydration, without any evidence of obvious external which turned out to be positive (sweat chloride >60 mEq/L) in all fluid loss. -

Hypokalemic Periodic Paralysis - an Owner's Manual
Hypokalemic periodic paralysis - an owner's manual Michael M. Segal MD PhD1, Karin Jurkat-Rott MD PhD2, Jacob Levitt MD3, Frank Lehmann-Horn MD PhD2 1 SimulConsult Inc., USA 2 University of Ulm, Germany 3 Mt. Sinai Medical Center, New York, USA 5 June 2009 This article focuses on questions that arise about diagnosis and treatment for people with hypokalemic periodic paralysis. We will focus on the familial form of hypokalemic periodic paralysis that is due to mutations in one of various genes for ion channels. We will only briefly mention other �secondary� forms such as those due to hormone abnormalities or due to kidney disorders that result in chronically low potassium levels in the blood. One can be the only one in a family known to have familial hypokalemic periodic paralysis if there has been a new mutation or if others in the family are not aware of their illness. For more general background about hypokalemic periodic paralysis, a variety of descriptions of the disease are available, aimed at physicians or patients. Diagnosis What tests are used to diagnose hypokalemic periodic paralysis? The best tests to diagnose hypokalemic periodic paralysis are measuring the blood potassium level during an attack of paralysis and checking for known gene mutations. Other tests sometimes used in diagnosing periodic paralysis patients are the Compound Muscle Action Potential (CMAP) and Exercise EMG; further details are here. The most definitive way to make the diagnosis is to identify one of the calcium channel gene mutations or sodium channel gene mutations known to cause the disease. However, known mutations are found in only 70% of people with hypokalemic periodic paralysis (60% have known calcium channel mutations and 10% have known sodium channel mutations). -

Difference in Allelic Expression of the CLCN1 Gene and the Possible Influence on the Myotonia Congenita Phenotype
European Journal of Human Genetics (2004) 12, 738–743 & 2004 Nature Publishing Group All rights reserved 1018-4813/04 $30.00 www.nature.com/ejhg ARTICLE Difference in allelic expression of the CLCN1 gene and the possible influence on the myotonia congenita phenotype Morten Dun1*, Eskild Colding-Jrgensen2, Morten Grunnet3,5, Thomas Jespersen3, John Vissing4 and Marianne Schwartz1 1Department of Clinical Genetics, 4062, University Hospital, Rigshospitalet, Blegdamsvej 9, DK-2100 Copenhagen, Denmark; 2Department of Clinical Neurophysiology 3063,University Hospital, Rigshospitalet, Blegdamsvej 9, DK- 2100 Copenhagen, Denmark; 3Department of Medical Physiology, The Panum Institute, University of Copenhagen, Blegdamsvej 3, DK-2200 Copenhagen N, Denmark; 4Department of Neurology and The Copenhagen Muscle Research Center, University Hospital, Rigshospitalet, Blegdamsvej 9, DK-2100 Copenhagen, Denmark Mutations in the CLCN1 gene, encoding a muscle-specific chloride channel, can cause either recessive or dominant myotonia congenita (MC). The recessive form, Becker’s myotonia, is believed to be caused by two loss-of-function mutations, whereas the dominant form, Thomsen’s myotonia, is assumed to be a consequence of a dominant-negative effect. However, a subset of CLCN1 mutations can cause both recessive and dominant MC. We have identified two recessive and two dominant MC families segregating the common R894X mutation. Real-time quantitative RT-PCR did not reveal any obvious association between the total CLCN1 mRNA level in muscle and the mode of inheritance, but the dominant family with the most severe phenotype expressed twice the expected amount of the R894X mRNA allele. Variation in allelic expression has not previously been described for CLCN1, and our finding suggests that allelic variation may be an important modifier of disease progression in myotonia congenita. -

Inherited Renal Tubulopathies—Challenges and Controversies
G C A T T A C G G C A T genes Review Inherited Renal Tubulopathies—Challenges and Controversies Daniela Iancu 1,* and Emma Ashton 2 1 UCL-Centre for Nephrology, Royal Free Campus, University College London, Rowland Hill Street, London NW3 2PF, UK 2 Rare & Inherited Disease Laboratory, London North Genomic Laboratory Hub, Great Ormond Street Hospital for Children National Health Service Foundation Trust, Levels 4-6 Barclay House 37, Queen Square, London WC1N 3BH, UK; [email protected] * Correspondence: [email protected]; Tel.: +44-2381204172; Fax: +44-020-74726476 Received: 11 February 2020; Accepted: 29 February 2020; Published: 5 March 2020 Abstract: Electrolyte homeostasis is maintained by the kidney through a complex transport function mostly performed by specialized proteins distributed along the renal tubules. Pathogenic variants in the genes encoding these proteins impair this function and have consequences on the whole organism. Establishing a genetic diagnosis in patients with renal tubular dysfunction is a challenging task given the genetic and phenotypic heterogeneity, functional characteristics of the genes involved and the number of yet unknown causes. Part of these difficulties can be overcome by gathering large patient cohorts and applying high-throughput sequencing techniques combined with experimental work to prove functional impact. This approach has led to the identification of a number of genes but also generated controversies about proper interpretation of variants. In this article, we will highlight these challenges and controversies. Keywords: inherited tubulopathies; next generation sequencing; genetic heterogeneity; variant classification. 1. Introduction Mutations in genes that encode transporter proteins in the renal tubule alter kidney capacity to maintain homeostasis and cause diseases recognized under the generic name of inherited tubulopathies. -
Neuromuscular Disorders Neurology in Practice: Series Editors: Robert A
Neuromuscular Disorders neurology in practice: series editors: robert a. gross, department of neurology, university of rochester medical center, rochester, ny, usa jonathan w. mink, department of neurology, university of rochester medical center,rochester, ny, usa Neuromuscular Disorders edited by Rabi N. Tawil, MD Professor of Neurology University of Rochester Medical Center Rochester, NY, USA Shannon Venance, MD, PhD, FRCPCP Associate Professor of Neurology The University of Western Ontario London, Ontario, Canada A John Wiley & Sons, Ltd., Publication This edition fi rst published 2011, ® 2011 by Blackwell Publishing Ltd Blackwell Publishing was acquired by John Wiley & Sons in February 2007. Blackwell’s publishing program has been merged with Wiley’s global Scientifi c, Technical and Medical business to form Wiley-Blackwell. Registered offi ce: John Wiley & Sons Ltd, The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK Editorial offi ces: 9600 Garsington Road, Oxford, OX4 2DQ, UK The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK 111 River Street, Hoboken, NJ 07030-5774, USA For details of our global editorial offi ces, for customer services and for information about how to apply for permission to reuse the copyright material in this book please see our website at www.wiley.com/wiley-blackwell The right of the author to be identifi ed as the author of this work has been asserted in accordance with the UK Copyright, Designs and Patents Act 1988. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, except as permitted by the UK Copyright, Designs and Patents Act 1988, without the prior permission of the publisher. -
THE NON-DYSTROPHIC MYOPATHIES JOHN PEARCE, M.B., M.R.C.P., Department of Neurology, the General Infirmary, Leeds
Postgrad Med J: first published as 10.1136/pgmj.41.476.347 on 1 June 1965. Downloaded from POSTGRAD. MED. J. (1965), 41, 347 THE NON-DYSTROPHIC MYOPATHIES JOHN PEARCE, M.B., M.R.C.P., Department of Neurology, The General Infirmary, Leeds. THE TERM 'myopathy' is applied to any disorder Polymyositis may affect people of any age, of the muscle fibre, the muscle fibre membrane, but the age of onset is from 30 to 60 in 60% the myoneural junction, or the muscle connect- of cases. The chief symptom is weakness of ive tissue. 'Non-dystrophic myopathy' includes proximal muscles of the arms and/or legs all diseases of muscle excluding those genetically in every case. Distal muscles are affected in determined primary degenerative myopathies, one third, and the neck muscles in two thirds collectively known as Muscular Dystrophy. of patients. Fever, muscular pain and tenderness TABLE 1 are seen most often in the more acute forms, CLASSIFICATION OF NON-DYSTROPHIC MYOPATHIES and their absence should not lead to neglecting 1. Inflammatory Polymyositis as a Myopathy Connective tissue disorders polymyositis possible diagnosis. Other inflammatory mvopathies Acute polymyositis is not common, but may 2. Metabolic Familial periodic paralysis progress rapidly and involve the respiratory Myopathy Muscle glycogenoses muscles, sometimes with a fatal termination Myoglobinuric myopathies within a few weeks or months. Myopathies associated with Subacute and electrolyte imbalance chronic forms are more frequent, and present Unclassified myopathies with a progressive weakness and moderate of shoulder 3. Endocrine Thyrotoxicosis wasting and pelvic girdle muscles. Myopathy Cushing's Syndrome There is sometimes no systemic disturbance, Steroid myopathy and pain and tenderness are lacking. -

Periodic Paralysis
Periodic Paralysis In Focus Dear Readers Fast Facts This “In Focus” report is the third in a series of MDA’s three-year commitment for all Hypokalemic periodic paralysis MDA comprehensive reports about the latest in periodic paralysis research as of March Hypokalemic PP can begin anywhere from neuromuscular disease research and manage- 2009 is $1,938,367. The Association’s early childhood to the 30s, with periodic ment. allocation for research on hyperkalemic attacks of severe weakness lasting hours This report focuses on the periodic and hypokalemic periodic paralysis to days. The frequency of attacks gener- paralyses, a group of disorders that result from research since 1950 is $8,125,341. ally lessens in the 40s or 50s. Permanent malfunctions in so-called ion channels, micro- MDA’s allocation for the recently weakness may persist between attacks, scopic tunnels that make possible high-speed identified Andersen-Tawil syndrome usually beginning in middle age and pro- movement of electrically charged particles is $515,430 since 2001. MDA is cur- gressing slowly over years. across barriers inside cells and between cells rently funding 11 grants in the periodic The most common underlying cause and their surroundings. paralyses. is any of several genetic mutations in When ion channels fail to open or close The periodic paralyses are gener- a gene on chromosome 1 that carries according to an exquisitely fine-tuned program, ally divided into hyperkalemic periodic instructions for a calcium channel protein episodes of paralysis of the skeletal muscles paralysis, hypokalemic periodic paralysis in skeletal muscle fibers. When this chan- and even temporary irregularities in the heart- and Andersen-Tawil syndrome.