Overview of Cardiac Anatomy Relevant to Catheter Ablation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
CT Cardiac Anatomy
CT cardiac anatomy M.Todorova Tokuda Hospital Sofia 1 MDCT vs US 2 Position of the heart • Position in the thoracic cavity • Cardiac apex • Cardiac base 3 Systematic approach Cardiac CT • Right atrium • Aorta • Right ventricle • Coronaries • PA • Cardiac Veins • PV • Valves • Left atrium • Pericardium • Left ventricle 4 Right atrium 5 Right atrium • RA appendage – Pectinate muscles >2mm – 20 sc.cm normal size on 4 ch.view • Crista terminalis • Sulcus terminalis • Coronary sinus • Thebesian valve • Eustachian valve • Internal septum • Fossa ovalis 6 Tricuspid valve • Tricuspid valve- separates RA from RV • Trileflet valve- anterior,posterior, septal • Structure- leflet,annulus,commi ssures 7 Right ventricle 8 RV-anatomy inflow tract 4 chamber view outflow tract 9 Volumetric parameters of RV • Normal quantitative RV Values • EF = 61+/-6 • End diastolic volume = 173+/-39 • End systolic volume = 69+/-22 • Strike volume = 104+/=21 • Mass = 35-45 10 RV-anatomic structure • Tricuspid valve • RV wall • Pulmonary valve • Intrventricular septum • Anterior longitudinal sulcus • Posterior longitudinal sulcus • Moderator band 11 • Interventricular septum – Separates ventricles – Thin wall – Convexity toward the right ventricle – Muscular ventricular septum – Membrannous ventricular septum • Anterior and posterior longitudinal sulcus – Ventricles separeted externally by grooves – Anterior longitudinal sulcus – Posterior longitudinal sulcus – Moderator band 12 Pulmonary valve • Three leaflet • Semilunar morphology 13 PA anatomy 14 Left atrium and pulmonary veins 15 • Pulmonry veins – Two inferior and two superior into either side of LA 16 LA - anatomy • LA • LA appendage – Arises from the superiorlateral aspect of the LA – Projects anteriorly over the proximal LCX artery – Pectinate muscles >1mm 17 Mitral valve • represent inflow tract of LV • bicuspid • fibrous ring mitral valve-annulus • triangular leaflets 18 Left ventricle 19 LV - anatomy • Inflow tract • Outflow tract • Chordae tendinae • Papillary muscles 20 LV wall Normal Anterior MI LV papillary muscles Ferencik et al. -
Morphological Classification of the Moderator Band and Its Relationship with the Anterior Papillary Muscle
Original Article https://doi.org/10.5115/acb.2019.52.1.38 pISSN 2093-3665 eISSN 2093-3673 Morphological classification of the moderator band and its relationship with the anterior papillary muscle Ju-Young Lee1, Mi-Sun Hur2 1Department of Biomedical Engineering, College of Medical Convergence, Catholic Kwandong University, Gangneung, 2Department of Anatomy, Catholic Kwandong University College of Medicine, Gangneung, Korea Abstract: This study investigated and classified the various types of moderator band (MB) in relation to the anterior papillary muscle, with the aim of providing anatomical reference information and fundamental knowledge for use when repairing the congenital defects and understanding the conduction system. The study investigated 38 formalin-fixed human hearts of both sexes obtained from donors aged 38–90 years. The MB was evident in 36 of the 38 specimens (94.7%). The morphology of the MB and its connection with the APM took various forms. The MBs that had a distinct shape were classified into three types according to their shape: cylindrical column, long and thin column, and wide and flat column. Types 2 and 3 were the most common, appearing in 15 (41.7%) and 14 (38.9%) of the 36 specimens, respectively, while type 1 was observed in seven specimens (19.4%). Type 3 was divided into subtypes based on their length. The MB usually originated from a single root (91.7%), with the remainder exhibiting double roots. The pairs of roots in the latter cases had different shapes. The originating point of the MB ranged from the supraventricular crest to the apex of the ventricle. -

Chapter Xi the Circulatory System and Blood
CHAPTER XI THE CIRCULATORY SYSTEM AND BLOOD Page General characterlstlcs______ __ __ _ __ __ __ __ __ __ _ 239 of these organs are independent of the beating of The pericardium ___ __ __ __ 239 the principal heart, and their primary function is The heart. _____ __ __ 240 Physiology of the heart.______________________________________________ 242 to oscillate the blood within the pallial sinuses. Automatism of heart beat. _ 242 The pacemaker system_ 245 THE PERICARDIUM Methods of study of heart beat_____________________________________ 247 Frequency of beat___ __ __ _ 248 Extracardlac regulatlon____ __ __ _ 250 The heart is located in the pericardium, a thin Effects of mineral salts and drugs___________________________________ 251 Blood vessels_ __ ___ _ 253 walled chamber between the visceral mass and the The arterial system______ __ __ ___ __ __ __ __ __ 253 adductor muscle (fig. 71). In a live oyster the The venous system_________________________________________________ 254 location of the heart is indicated by the throbbing The accessory heart._____________ 258 The blood______ __ __ __ __ __ __ __ 259 of the wall of the pericardium on the left side. Color of blood_ __ __ 261 Here the pericardium wall lies directly under the The hyaline cells___________________________________________________ 261 The granular cells .______________________________________ 262 shell. On the right side the promyal chamber Specific gravity of blood____________________________________________ 265 extends down over the heart region and the mantle Serology ___ __________ __________________ ____ __ ______________________ 265 Bibliography __ __ __ __ __ __ __ 266 separates the pericardium wall from the shell. The cavity in which the heart is lodged is slightly A heart, arteries, veins, and open sinuses form asymmetrical; on the right side it extends farther the circulatory system of oysters and other bi along the anterior part of the adductor muscle valves. -

Distance Learning Program Anatomy of the Human Heart/Pig Heart Dissection Middle School/ High School
Distance Learning Program Anatomy of the Human Heart/Pig Heart Dissection Middle School/ High School This guide is for middle and high school students participating in AIMS Anatomy of the Human Heart and Pig Heart Dissections. Programs will be presented by an AIMS Anatomy Specialist. In this activity students will become more familiar with the anatomical structures of the human heart by observing, studying, and examining human specimens. The primary focus is on the anatomy and flow of blood through the heart. Those students participating in Pig Heart Dissections will have the opportunity to dissect and compare anatomical structures. At the end of this document, you will find anatomical diagrams, vocabulary review, and pre/post tests for your students. National Science Education (NSES) Content Standards for grades 9-12 • Content Standard:K-12 Unifying Concepts and Processes :Systems order and organization; Evidence, models and explanation; Form and function • Content Standard F, Science in Personal and Social Perspectives: Personal and community health • Content Standard C, Life Science: Matter, energy and organization of living systems • Content Standard A Science as Inquiry National Science Education (NSES) Content Standards for grades 5-8 • Content Standard A Science as Inquiry • Content Standard C, Life Science: Structure and function in living systems; Diversity and adaptations of organisms • Content Standard F, Science in Personal and Social Perspectives: Personal Health Show Me Standards (Science and Health/Physical Education) • Science 3. Characteristics and interactions of living organisms • Health/Physical Education 1. Structures of, functions of and relationships among human body systems Objectives: The student will be able to: 1. -

Readingsample
Integrating Cardiology for Nuclear Medicine Physicians A Guide to Nuclear Medicine Physicians Bearbeitet von Assad Movahed, Gopinath Gnanasegaran, John Buscombe, Margaret Hall 1. Auflage 2008. Buch. xiv, 544 S. Hardcover ISBN 978 3 540 78673 3 Format (B x L): 21 x 27,9 cm Weitere Fachgebiete > Medizin > Sonstige Medizinische Fachgebiete > Nuklearmedizin, Radiotherapie Zu Inhaltsverzeichnis schnell und portofrei erhältlich bei Die Online-Fachbuchhandlung beck-shop.de ist spezialisiert auf Fachbücher, insbesondere Recht, Steuern und Wirtschaft. Im Sortiment finden Sie alle Medien (Bücher, Zeitschriften, CDs, eBooks, etc.) aller Verlage. Ergänzt wird das Programm durch Services wie Neuerscheinungsdienst oder Zusammenstellungen von Büchern zu Sonderpreisen. Der Shop führt mehr als 8 Millionen Produkte. Chapter The Heart: Anatomy, Physiology and 1 Exercise Physiology Syed Shah, Gopinath Gnanasegaran, Jeanette Sundberg-Cohon, and John R Buscombe Contents 1.1 Introduction 1.1 Introduction . 3 1.2 Anatomy of the Heart . 3 The impact of anatomy on medicine was first recognised 1.2.1 Chamber and Valves . 4 by Andreas Vesalius during the 16th century [1] and 1.2.2 Cardiac Cell and Cardiac Muscle ......... 4 from birth to death, the heart is the most talked about 1.2.3 Coronary Arteries and Cardiac Veins . 6 organ of the human body. It is the centre of attraction 1.2.4 Venous Circulation ..................... 6 for people from many lifestyles, such as philosophers, 1.2.5 Nerve Supply of the Heart ............... 9 artists, poets and physicians/surgeons. The heart is one 1.2.6 Conduction System of the Heart . 10 of the most efficient organs in the human body and 1.3 Physiology of the Heart . -

4B. the Heart (Cor) 1
Henry Gray (1821–1865). Anatomy of the Human Body. 1918. 4b. The Heart (Cor) 1 The heart is a hollow muscular organ of a somewhat conical form; it lies between the lungs in the middle mediastinum and is enclosed in the pericardium (Fig. 490). It is placed obliquely in the chest behind the body of the sternum and adjoining parts of the rib cartilages, and projects farther into the left than into the right half of the thoracic cavity, so that about one-third of it is situated on the right and two-thirds on the left of the median plane. Size.—The heart, in the adult, measures about 12 cm. in length, 8 to 9 cm. in breadth at the 2 broadest part, and 6 cm. in thickness. Its weight, in the male, varies from 280 to 340 grams; in the female, from 230 to 280 grams. The heart continues to increase in weight and size up to an advanced period of life; this increase is more marked in men than in women. Component Parts.—As has already been stated (page 497), the heart is subdivided by 3 septa into right and left halves, and a constriction subdivides each half of the organ into two cavities, the upper cavity being called the atrium, the lower the ventricle. The heart therefore consists of four chambers, viz., right and left atria, and right and left ventricles. The division of the heart into four cavities is indicated on its surface by grooves. The atria 4 are separated from the ventricles by the coronary sulcus (auriculoventricular groove); this contains the trunks of the nutrient vessels of the heart, and is deficient in front, where it is crossed by the root of the pulmonary artery. -

Anomalous Middle Cardiac Vein Draining Into the Left Atrium
IMAGES IN THIS ISSUE Cardiovascular Disorders http://dx.doi.org/10.3346/jkms.2016.31.8.1179 • J Korean Med Sci 2016; 31: 1179-1180 Anomalous Middle Cardiac Vein Draining into the Left Atrium Jihyun Sohn,1 Young Soo Lee,2 Seung Pyo Hong,2 and Sung Hee Mun3 1Department of Cardiology, Kyungpook National University Hospital, Daegu, Korea; 2Department of Cardiology, Catholic University of Daegu, Daegu, Korea; 3Department of Radiology, Catholic University of Daegu, Daegu, Korea RV LV RA LA A B C LA CS RA PVLV LA MCV MCV LV D E Fig. 1. Cardiac computed tomography demonstrates the middle cardiac vein draining into the left atrium (yellow arrows). (A-C) Axial serial scan images of cardiac computed to- mography after contrast dye injection. (D) The 3-dimensional volume rendering image of cardiac computed tomography. (E) The curved planar reformation image of cardiac computed tomography. A 67-year-old woman was admitted for radiofrequency catheter oxygen supplement. Her electrocardiogram, chest X-ray, and ablation (RFCA) of paroxysmal atrial fibrillation. She had un- echocardiogram were within normal limits. She underwent derwent patch closure of atrial septal defect 7 years before. Her cardiac computed tomography for the left atrial reconstruction arterial blood oxygen saturation level was 94.6% without any before the RFCA. It revealed abnormal drainage of the middle © 2016 The Korean Academy of Medical Sciences. pISSN 1011-8934 This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. -

Blood Vessels
BLOOD VESSELS Blood vessels are how blood travels through the body. Whole blood is a fluid made up of red blood cells (erythrocytes), white blood cells (leukocytes), platelets (thrombocytes), and plasma. It supplies the body with oxygen. SUPERIOR AORTA (AORTIC ARCH) VEINS & VENA CAVA ARTERIES There are two basic types of blood vessels: veins and arteries. Veins carry blood back to the heart and arteries carry blood from the heart out to the rest of the body. Factoid! The smallest blood vessel is five micrometers wide. To put into perspective how small that is, a strand of hair is 17 micrometers wide! 2 BASIC (ARTERY) BLOOD VESSEL TUNICA EXTERNA TUNICA MEDIA (ELASTIC MEMBRANE) STRUCTURE TUNICA MEDIA (SMOOTH MUSCLE) Blood vessels have walls composed of TUNICA INTIMA three layers. (SUBENDOTHELIAL LAYER) The tunica externa is the outermost layer, primarily composed of stretchy collagen fibers. It also contains nerves. The tunica media is the middle layer. It contains smooth muscle and elastic fiber. TUNICA INTIMA (ELASTIC The tunica intima is the innermost layer. MEMBRANE) It contains endothelial cells, which TUNICA INTIMA manage substances passing in and out (ENDOTHELIUM) of the bloodstream. 3 VEINS Blood carries CO2 and waste into venules (super tiny veins). The venules empty into larger veins and these eventually empty into the heart. The walls of veins are not as thick as those of arteries. Some veins have flaps of tissue called valves in order to prevent backflow. Factoid! Valves are found mainly in veins of the limbs where gravity and blood pressure VALVE combine to make venous return more 4 difficult. -

MORPHOMETRIC and MORPHOLOGICAL STUDY on the SEPTO- MARGINAL TRABECULA Shrikanya M Shet *1, Kuldeep M D 2, Sheela G Nayak 3, V S Pare 4, Jyothi S R 5 , M P Shenoy 6
International Journal of Anatomy and Research, Int J Anat Res 2018, Vol 6(3.1):5458-63. ISSN 2321-4287 Original Research Article DOI: https://dx.doi.org/10.16965/ijar.2018.238 MORPHOMETRIC AND MORPHOLOGICAL STUDY ON THE SEPTO- MARGINAL TRABECULA Shrikanya M Shet *1, Kuldeep M D 2, Sheela G Nayak 3, V S Pare 4, Jyothi S R 5 , M P Shenoy 6. *1 Student, 1st MBBS, K V G Medical College, Sullia, Rajiv Gandhi University Of Health Sciences, Karnataka. 2 Student, 1st MBBS, K V G Medical College, Sullia, Rajiv Gandhi University Of Health Sciences, Karnataka. 3 Dean Academics, K V G Medical College, Sullia, Rajiv Gandhi University Of Health Sciences, Karnataka. 4 Professor and HOD, Department Of Anatomy, K V G Medical College, Sullia, Rajiv Gandhi Univer- sity Of Health Sciences, Karnataka. 5,6 Assistant Professor, Department Of Anatomy, K V G Medical College, Sullia, Rajiv Gandhi University Of Health Sciences, Karnataka. ABSTRACT Background and objectives: Moderator band is a specialized bridge present between the base of the anterior papillary muscle and interventricular septum. It carries the right branch of the bundle of HIS with it. The band is known to prevent the over distension of the right ventricle during the diastolic phase. There is a need of lot of research and studies on the septomarginal trabecula as it proves to be important clinically. Here we measured the length, breadth, height, angle with the interventricular septum, and the superficial marking of Moderator band on the sternocostal surface of the right ventricle is done. This paper describes the morphological variations found in its origin and insertion. -
Chapter 12 the Cardiovascular System: the Heart Pages
CHAPTER 12 THE CARDIOVASCULAR SYSTEM: THE HEART PAGES 388 - 411 LOCATION & GENERAL FEATURES OF THE HEART TWO CIRCUIT CIRCULATORY SYSTEM DIVISIONS OF THE HEART FOUR CHAMBERS Right Atrium Left Atrium Receives blood from Receives blood from the systemic circuit the pulmonary circuit FOUR CHAMBERS Right Ventricle Left Ventricle Ejects blood into the Ejects blood into the pulmonary circuit systemic circuit FOUR VALVES –ATRIOVENTRICULAR VALVES Right Atrioventricular Left Atrioventricular Valve (AV) Valve (AV) Tricuspid Valve Bicuspid Valve and Mitral Valve FOUR VALVES –SEMILUNAR VALVES Pulmonary valve Aortic Valve Guards entrance to Guards entrance to the pulmonary trunk the aorta FLOW OF BLOOD MAJOR VEINS AND ARTERIES AROUND THE HEART • Arteries carry blood AWAY from the heart • Veins allow blood to VISIT the heart MAJOR VEINS AND ARTERIES ON THE HEART Coronary Circulation – Supplies blood to the muscle tissue of the heart ARTERIES Elastic artery: Large, resilient vessels. pulmonary trunk and aorta Muscular artery: Medium-sized arteries. They distribute blood to skeletal muscles and internal organs. external carotid artery of the neck Arteriole: Smallest of arteries. Lead into capillaries VEINS Large veins: Largest of the veins. Superior and Inferior Vena Cava Medium-sized veins: Medium sized veins. Pulmonary veins Venules: the smallest type of vein. Lead into capillaries CAPILLARIES Exchange of molecules between blood and interstitial fluid. FLOW OF BLOOD THROUGH HEART TISSUES OF THE HEART THE HEART WALL Pericardium Outermost layer Serous membrane Myocardium Middle layer Thick muscle layer Endocardium Inner lining of pumping chambers Continuous with endothelium CARDIAC MUSCLE Depend on oxygen to obtain energy Abundant in mitochondria In contact with several other cardiac muscles Intercalated disks – interlocking membranes of adjacent cells Desmosomes Gap junctions CONNECTIVE TISSUE Wrap around each cardiac muscle cell and tie together adjacent cells. -
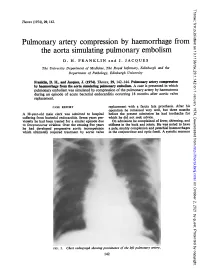
The Aorta Simulating Pulmonary Embolism D
Thorax: first published as 10.1136/thx.29.1.142 on 1 January 1974. Downloaded from Thorax (1974), 29, 142. Pulmonary artery compression by haemorrhage from the aorta simulating pulmonary embolism D. H. FRANKLIN and J. JACQUES The University Department of Medicine, The Royal Infirmary, Edinburgh and the Department of Pathology, Edinburgh University Franklin, D. H., and Jacques, J. (1974). Thorax, 29, 142-144. Pulmonary artery compression by haemorrhage from the aorta simulating pulmonary embolism. A case is presented in which pulmonary embolism was simulated by compression of the pulmonary artery by haematoma during an episode of acute bacterial endocarditis occurring 18 months after aortic valve replacement. CASE REPORT replacement with a fascia lata prosthesis. After his operation he remained very well, but three months A 38-year-old male clerk was admitted to hospital before the present admission he had toothache for suffering from bacterial efndocarditis. Seven years pre- which he did not seek advice. viomly he had been treated for a similar episode due On admission he complained of fever, shivering, and to Streptococcus viridans. Over the ensuing five years stiffness in the back and joints. He was noted to have he had developed progressive aortic incompetence a pale, muddy complexion and petechial haemorrhages which ultimately required treatment by aortic valve in the conjunctivae and optic fundi. A systolic murmur http://thorax.bmj.com/ on October 2, 2021 by guest. Protected copyright. FIG. 1. Chesvt radiograph showing prominence of the left pulmonary artery. 142 Thorax: first published as 10.1136/thx.29.1.142 on 1 January 1974. -

Arrhythmia Study Guide – 2 – Sinus and Atrial Rhythms
Arrhythmia Study Guide – 2 – Sinus and Atrial Rhythms Review of Conduction System: SA Node initiates electrical impulses at a rate of 60 – 100 BPM and is the primary pacemaker of the heart. The AV node recieves the impulse from the SA Node through the internodal pathways. The AV Node then delays relay ofthe impulse to the Bundle of His to allow the atria to empty into the ventricles before the ventricular contraction starts. The Bundle of His relays the impulse to the right and left bundle branches. The bundle branches relay to the Purkinje Fibers and the Purkinje Fibers deliver the impulse to the ventricular myocardium to trigger the ventricular contraction. If the SA Node fails to fire, or fires at a much slower rate, the AV node may take over as pacemaker at a rate of 40 - 60 BPM. If the AV Node fails or fires at a much slower rate, the Perkinjie fibers may act as pacemaker at a rate of 20 – 40 BPM. The ECG is a graph of the electrical activity of the heart. Knowing how the heart conducts the electrical impulses provides a strong basis for understanding the ECG strip – and figuring out what is or is not working correctly. SINUS RHYTHMS Rhythms that originate from the SA Node are characterized by upright uniform P-waves followed by a QRS complex. The P-R interval is constant, and the atrial (P-waves) and ventricular (QRS Complex) rhythms are regular. A rate less than 60 is bradycardic, 60 to 100 is normal, over 100 is tachycardic.