EPPPIC) Individual Participant Data (IPD) Meta-Analysis : Protocol
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Endocrine Disrupting Compounds and Prostate Cell Proliferation
Review Article Clinics in Oncology Published: 18 Oct, 2016 Endocrine Disrupting Compounds and Prostate Cell Proliferation Joubert Banjop Kharlyngdoh and Per-Erik Olsson* Department of Biology, Örebro University, Sweden Abstract Epidemiological, in vitro and animal studies have indicated that Endocrine Disrupting Compounds (EDCs) influence the normal growth and development of the prostate as well as development and progression of prostate cancer. This has been linked to an increased presence of environmental chemicals that interfere with hormonal signaling. Many of these effects appear to be associated with interferences with steroid hormone receptor signaling or by affecting steroidogenesis. Currently, there is abundant evidence from epidemiological studies linking pesticides and EDCs with elevated prostate cancer risk. Bisphenol-A, a known EDC, has been shown to promote induction of Prostate Specific Antigen (PSA), which is a biomarker for prostate cancer, in the LNCaP human prostate carcinoma cells, and to increase prostate carcinogenesis in animal models. Our research has focused on AR signaling and identification of novel androgenic and anti-androgenic EDCs. Using prostate cancer cell lines we have shown that the AR agonist, TBECH, and antagonist ATE, which is also a partial ART877A agonist, induce PSA expression. With the increasing presence of these EDCs in indoor and outdoor air, follows an increased risk of disturbed prostate development, regulation and function. Hence, identification of the contribution of EDCs to prostate cancer -

Pharmacy and Poisons (Third and Fourth Schedule Amendment) Order 2017
Q UO N T FA R U T A F E BERMUDA PHARMACY AND POISONS (THIRD AND FOURTH SCHEDULE AMENDMENT) ORDER 2017 BR 111 / 2017 The Minister responsible for health, in exercise of the power conferred by section 48A(1) of the Pharmacy and Poisons Act 1979, makes the following Order: Citation 1 This Order may be cited as the Pharmacy and Poisons (Third and Fourth Schedule Amendment) Order 2017. Repeals and replaces the Third and Fourth Schedule of the Pharmacy and Poisons Act 1979 2 The Third and Fourth Schedules to the Pharmacy and Poisons Act 1979 are repealed and replaced with— “THIRD SCHEDULE (Sections 25(6); 27(1))) DRUGS OBTAINABLE ONLY ON PRESCRIPTION EXCEPT WHERE SPECIFIED IN THE FOURTH SCHEDULE (PART I AND PART II) Note: The following annotations used in this Schedule have the following meanings: md (maximum dose) i.e. the maximum quantity of the substance contained in the amount of a medicinal product which is recommended to be taken or administered at any one time. 1 PHARMACY AND POISONS (THIRD AND FOURTH SCHEDULE AMENDMENT) ORDER 2017 mdd (maximum daily dose) i.e. the maximum quantity of the substance that is contained in the amount of a medicinal product which is recommended to be taken or administered in any period of 24 hours. mg milligram ms (maximum strength) i.e. either or, if so specified, both of the following: (a) the maximum quantity of the substance by weight or volume that is contained in the dosage unit of a medicinal product; or (b) the maximum percentage of the substance contained in a medicinal product calculated in terms of w/w, w/v, v/w, or v/v, as appropriate. -

PHARMACEUTICAL APPENDIX to the TARIFF SCHEDULE 2 Table 1
Harmonized Tariff Schedule of the United States (2020) Revision 19 Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2020) Revision 19 Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 2 Table 1. This table enumerates products described by International Non-proprietary Names INN which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service CAS registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. -

The Inhaled Steroid Ciclesonide Blocks SARS-Cov-2 RNA Replication by Targeting Viral
bioRxiv preprint doi: https://doi.org/10.1101/2020.08.22.258459; this version posted August 24, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 1 The inhaled steroid ciclesonide blocks SARS-CoV-2 RNA replication by targeting viral 2 replication-transcription complex in culture cells 3 4 Shutoku Matsuyamaa#, Miyuki Kawasea, Naganori Naoa, Kazuya Shiratoa, Makoto Ujikeb, Wataru 5 Kamitanic, Masayuki Shimojimad, and Shuetsu Fukushid 6 7 aDepartment of Virology III, National Institute of Infectious Diseases, Tokyo, Japan 8 bFaculty of Veterinary Medicine, Nippon Veterinary and Life Science University, Tokyo, Japan 9 cDepartment of Infectious Diseases and Host Defense, Gunma University Graduate School of 10 Medicine, Gunma, Japan 11 dDepartment of Virology I, National Institute of Infectious Diseases, Tokyo, Japan. 12 13 Running Head: Ciclesonide blocks SARS-CoV-2 replication 14 15 #Address correspondence to Shutoku Matsuyama, [email protected] 16 17 Word count: Abstract 149, Text 3,016 bioRxiv preprint doi: https://doi.org/10.1101/2020.08.22.258459; this version posted August 24, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 18 Abstract 19 We screened steroid compounds to obtain a drug expected to block host inflammatory responses and 20 MERS-CoV replication. Ciclesonide, an inhaled corticosteroid, suppressed replication of MERS-CoV 21 and other coronaviruses, including SARS-CoV-2, the cause of COVID-19, in cultured cells. The 22 effective concentration (EC90) of ciclesonide for SARS-CoV-2 in differentiated human bronchial 23 tracheal epithelial cells was 0.55 μM. -

Pharmacology on Your Palms CLASSIFICATION of the DRUGS
Pharmacology on your palms CLASSIFICATION OF THE DRUGS DRUGS FROM DRUGS AFFECTING THE ORGANS CHEMOTHERAPEUTIC DIFFERENT DRUGS AFFECTING THE NERVOUS SYSTEM AND TISSUES DRUGS PHARMACOLOGICAL GROUPS Drugs affecting peripheral Antitumor drugs Drugs affecting the cardiovascular Antimicrobial, antiviral, Drugs affecting the nervous system Antiallergic drugs system antiparasitic drugs central nervous system Drugs affecting the sensory Antidotes nerve endings Cardiac glycosides Antibiotics CNS DEPRESSANTS (AFFECTING THE Antihypertensive drugs Sulfonamides Analgesics (opioid, AFFERENT INNERVATION) Antianginal drugs Antituberculous drugs analgesics-antipyretics, Antiarrhythmic drugs Antihelminthic drugs NSAIDs) Local anaesthetics Antihyperlipidemic drugs Antifungal drugs Sedative and hypnotic Coating drugs Spasmolytics Antiviral drugs drugs Adsorbents Drugs affecting the excretory system Antimalarial drugs Tranquilizers Astringents Diuretics Antisyphilitic drugs Neuroleptics Expectorants Drugs affecting the hemopoietic system Antiseptics Anticonvulsants Irritant drugs Drugs affecting blood coagulation Disinfectants Antiparkinsonian drugs Drugs affecting peripheral Drugs affecting erythro- and leukopoiesis General anaesthetics neurotransmitter processes Drugs affecting the digestive system CNS STIMULANTS (AFFECTING THE Anorectic drugs Psychomotor stimulants EFFERENT PART OF THE Bitter stuffs. Drugs for replacement therapy Analeptics NERVOUS SYSTEM) Antiacid drugs Antidepressants Direct-acting-cholinomimetics Antiulcer drugs Nootropics (Cognitive -

Andréia Gomes Bezerra ANÁLISES SOBRE a RELAÇÃO DO USO DE
Andréia Gomes Bezerra ANÁLISES SOBRE A RELAÇÃO DO USO DE CONTRACEPTIVOS HORMONAIS E PADRÃO DE SONO EM MULHERES EM IDADE FÉRTIL Tese apresentada à Universidade Federal de São Paulo – Escola Paulista de Medicina, para obtenção do Título de Doutora em Ciências São Paulo 2019 Andréia Gomes Bezerra ANÁLISES SOBRE A RELAÇÃO DO USO DE CONTRACEPTIVOS HORMONAIS E PADRÃO DE SONO EM MULHERES EM IDADE FÉRTIL Tese apresentada à Universidade Federal de São Paulo – Escola Paulista de Medicina, para obtenção do Título de Doutora em Ciências Orientadora: Profa. Dra. Helena Hachul Coorientadora: Prof. Dra. Monica Levy Andersen São Paulo 2019 Bezerra, Andréia Gomes Análises sobre a relação do uso de contraceptivos hormonais e padrão de sono em mulheres em idade fértil/Andréia Gomes Bezerra – São Paulo, 2019. 179 pp. Tese (Doutorado) – Universidade Federal de São Paulo. Escola Paulista de Medicina. Programa de Pós-Graduação em Psicobiologia. Título em inglês: Analysis of the use of hormonal contraceptives and sleep pattern in women at reproductive age. 1. Sono. 2. Mulher. 3. Contraceptivo hormonal. 4. Hormônios esteroides. 5. Meta-análise UNIVERSIDADE FEDERAL DE SÃO PAULO ESCOLA PAULISTA DE MEDICINA DEPARTAMENTO DE PSICOBIOLOGIA Chefe do Departamento: Profa. Dr. José Carlos F. Galduróz Coordenadora do Curso de Pós-Graduação Profa. Dra. Vânia D’Almeida iii Andréia Gomes Bezerra ANÁLISES SOBRE A RELAÇÃO DO USO DE CONTRACEPTIVOS HORMONAIS E PADRÃO DE SONO EM MULHERES EM IDADE FÉRTIL PRESIDENTE DA BANCA Profa. Dra. Helena Hachul BANCA EXAMINADORA Profa. Dra. Ligia Lucchesi Profa. Dra. Márcia Barbieri Profa. Dra. Renata Mazaro e Costa Profa. Dra. Sonia Tamanaha SUPLENTES Profa. Dr. -

2012 Harmonized Tariff Schedule Pharmaceuticals Appendix
Harmonized Tariff Schedule of the United States (2014) (Rev. 1) Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2014) (Rev. 1) Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 2 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. ABACAVIR 136470-78-5 ACEVALTRATE 25161-41-5 ABAFUNGIN 129639-79-8 ACEXAMIC ACID 57-08-9 ABAGOVOMAB 792921-10-9 ACICLOVIR 59277-89-3 ABAMECTIN 65195-55-3 ACIFRAN 72420-38-3 ABANOQUIL 90402-40-7 ACIPIMOX 51037-30-0 ABAPERIDONE 183849-43-6 ACITAZANOLAST 114607-46-4 ABARELIX 183552-38-7 ACITEMATE 101197-99-3 ABATACEPT 332348-12-6 ACITRETIN 55079-83-9 ABCIXIMAB 143653-53-6 ACIVICIN 42228-92-2 ABECARNIL 111841-85-1 ACLANTATE 39633-62-0 ABETIMUS 167362-48-3 ACLARUBICIN 57576-44-0 ABIRATERONE 154229-19-3 ACLATONIUM NAPADISILATE 55077-30-0 ABITESARTAN 137882-98-5 ACLIDINIUM BROMIDE 320345-99-1 ABLUKAST 96566-25-5 ACODAZOLE 79152-85-5 ABRINEURIN 178535-93-8 ACOLBIFENE 182167-02-8 ABUNIDAZOLE 91017-58-2 ACONIAZIDE 13410-86-1 ACADESINE 2627-69-2 ACOTIAMIDE 185106-16-5 -

WO 2012/055840 Al
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date _ . _ . 3 May 2012 (03.05.2012) WO 2012/055840 Al (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/00 (2006.01) A61P 5/30 (2006.01) kind of national protection available): AE, AG, AL, AM, A61K 31/565 (2006.01) A61P 5/34 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, A61K 31/57 (2006.01) A61P 15/00 (2006.01) CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, A61K 33/30 (2006.01) A61P 15/18 (2006.01) DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, (21) International Application Number: KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, PCT/EP201 1/068596 ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, (22) International Filing Date: NO, NZ, OM, PE, PG, PH, PL, PT, QA, RO, RS, RU, 25 October 201 1 (25.10.201 1) RW, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, (25) Filing Language: English ZM, ZW. (26) Publication Langi English (84) Designated States (unless otherwise indicated, for every (30) Priority Data: kind of regional protection available): ARIPO (BW, GH, 61/407,570 28 October 2010 (28.10.2010) US GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, (71) Applicant (for all designated States except US): BAYER RU, TJ, TM), European (AL, AT, BE, BG, CH, CY, CZ, PHARMA AKTIENGESELLSCHAFT [DE/DE]; DE, DK, EE, ES, FI, FR, GB, GR, HR, HU, IE, IS, ΓΓ, Muller Strasse 178, 13353 Berlin (DE). -
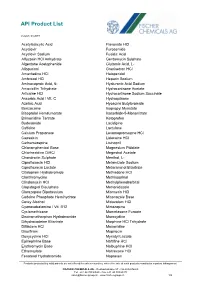
API Product List
API Product List Version: 03.2019 Acetylsalicylic Acid Flavoxate HCl Acyclovir Furosemide Acyclovir Sodium Fusidic Acid Alfuzosin HCl Anhydrate Gentamycin Sulphate Algestone Acetophenide Glutamic Acid, L- Allopurinol Granisetron HCl Amantadine HCl Haloperidol Ambroxol HCl Heparin Sodium Aminocaproic Acid, 6- Hyaluronic Acid Sodium Amoxicillin Trihydrate Hydrocortisone Acetate Articaine HCl Hydrocortisone Sodium Succinate Ascorbic Acid / Vit. C Hydroquinone Azelaic Acid Hyoscine Butylbromide Benzocaine Isopropyl Myristate Bisoprolol Hemifumarate Isosorbide-5-Mononitrate Brimonidine Tartrate Ketoprofen Budesonide Lacidipine Caffeine Lactulose Calcium Propionate Levomepromazine HCl Capsaicin Lidocaine HCl Carbamazepine Lisinopril Chloramphenicol Base Magnesium Pidolate Chlorhexidine DiHCl Megestrol Acetate Chondroitin Sulphate Menthol, L- Ciprofloxacin HCl Metamizole Sodium Ciprofloxacin Lactate Metaraminol Bitartrate Citalopram Hydrobromide Methadone HCl Clarithromycine Methisoprinol Clindamycin HCl Methylphenobarbital Clopidogrel Bisulphate Metronidazole Clorazepate Dipotassium Mianserin HCl Codeine Phosphate Hemihydrate Miconazole Base Corey Alcohol Midazolam HCl Cyanocobalamine / Vit. B12 Mirtazapine Cyclomethicone Mometasone Furoate Dextromethorphan Hydrobromide Moroxydine Dihydrocodeine Bitartrate Morphine HCl Trihydrate Diltiazem HCl Moxonidine Disulfiram Mupirocin Doxycycline HCl Myristyl Lactate Epinephrine Base Naftifine HCl Erythromycin Base Nalbuphine HCl Ethamsylate Naltrexone HCl Fenoterol Hydrobromide Naproxen Products protected -
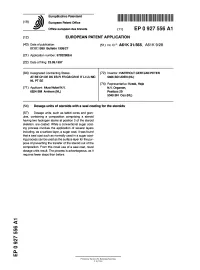
Dosage Units of Steroids with a Seal Coating for the Steroids
~™ iiiiiii nun iiiiiiii inn mil mil inn iiiii inn urn mill mi mi m (19) J European Patent Office Office europeen des brevets (11) EP 0 927 556 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication:ation: (51) |nt. ci.6: A61 K 31/565, A61 K 9/28 07.07.1999 Bulletin 1999/27 (21) Application number: 97202908.6 (22) Date of filing: 23.09.1997 (84) Designated Contracting States: (72) Inventor: HARTHOLT GERTJAN PETER AT BE CH DE DK ES Fl FR GB GR IE IT LI LU MC 5406 BD UDEN (NL) NL PT SE (74) Representative: Kraak, Hajo (71) Applicant: Akzo Nobel N.V. N.V. Organon, 6824 BM Arnhem (NL) Postbus 20 5340 BH OSS (NL) (54) Dosage units of steroids with a seal coating for the steroids (57) Dosage units, such as tablet cores and gran- ules, containing a composition comprising a steroid having two hydrogen atoms at position 3 of the steroid skeleton, are coated. While a conventional sugar coat- ing process involves the application of several layers including, as a surface layer, a sugar coat, it was found that a seal coat such as normally used in a sugar coat- ing process can be used as the surface layer for the pur- pose of preventing the transfer of the steroid out of the composition. From this novel use of a seal coat, novel dosage units result. The process is advantageous, as it requires fewer steps than before. < CO LO LO r»- Csl o Q_ LU Printed by Xerox (UK) Business Services 2.16.7/3.6 1 EP 0 927 556 A1 Description ing the dosage unit to coating steps comprising the application of a seal coat. -

Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DIX to the HTSUS—Continued
20558 Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DEPARMENT OF THE TREASURY Services, U.S. Customs Service, 1301 TABLE 1.ÐPHARMACEUTICAL APPEN- Constitution Avenue NW, Washington, DIX TO THE HTSUSÐContinued Customs Service D.C. 20229 at (202) 927±1060. CAS No. Pharmaceutical [T.D. 95±33] Dated: April 14, 1995. 52±78±8 ..................... NORETHANDROLONE. A. W. Tennant, 52±86±8 ..................... HALOPERIDOL. Pharmaceutical Tables 1 and 3 of the Director, Office of Laboratories and Scientific 52±88±0 ..................... ATROPINE METHONITRATE. HTSUS 52±90±4 ..................... CYSTEINE. Services. 53±03±2 ..................... PREDNISONE. 53±06±5 ..................... CORTISONE. AGENCY: Customs Service, Department TABLE 1.ÐPHARMACEUTICAL 53±10±1 ..................... HYDROXYDIONE SODIUM SUCCI- of the Treasury. NATE. APPENDIX TO THE HTSUS 53±16±7 ..................... ESTRONE. ACTION: Listing of the products found in 53±18±9 ..................... BIETASERPINE. Table 1 and Table 3 of the CAS No. Pharmaceutical 53±19±0 ..................... MITOTANE. 53±31±6 ..................... MEDIBAZINE. Pharmaceutical Appendix to the N/A ............................. ACTAGARDIN. 53±33±8 ..................... PARAMETHASONE. Harmonized Tariff Schedule of the N/A ............................. ARDACIN. 53±34±9 ..................... FLUPREDNISOLONE. N/A ............................. BICIROMAB. 53±39±4 ..................... OXANDROLONE. United States of America in Chemical N/A ............................. CELUCLORAL. 53±43±0 -
Pharmacology Cito
Pharmacology Cito 5 Read: it is important! Dear future physicians and pharmaceutists! The scientific and pedagogical staff of the Pharmacology department of the National University of Pharmacy (Kharkiv) presents a new textbook "Pharmacology – Cito!" to you. We want to change the myth that it is impossible to learn pharmacology quickly and qualitatively. The textbook "Pharmacology – Cito!" is published for those, who have decided to connect his or her profession with medicines, but think that a great amount of the information in pharmacology is hard to learn. Taking this fact into account we have decided to help those, who wish to master pharmacology in logical, fast - "Cito!"- version. Not be afraid of pharmacology! The 40-year experience of teaching pharmacology testifies that for the last 10-15 years a tendency of reducing the amount of classroom hours in pharmacology because of increasing the amount of the individual work is being observed. However, because of the lack of time and the constant increasing volume of information in pharmacology, everyone has not enough time to master it soundly and qualitatively. This textbook trains future pharmaceutists and physicians in the pharmacological logic, i.e. knowing the mechanisms of drug action one can understand their pharmacodynamics, naturally, on the basis of pharmacodynamics one can find logically the indications to their application and from their side effects the contraindications can be seen. The information about the peculiarities of medicines has been generalized and given as a pharmacological ―face‖ in tables. The volume of this textbook in pharmacology is sufficient for acquiring the confidence in the opportunity of the further improving of knowledge in this discipline, which is important for a physician and a pharmaceutist.