Pittsburgh Journal of Anesthesiology, 2016
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Incremental Costs of Introducing Jet Injection Technology for Delivery of Routine Childhood Vaccinations: Comparative Analysis from Brazil, India, and South Africa
Vaccine 29 (2011) 969–975 Contents lists available at ScienceDirect Vaccine journal homepage: www.elsevier.com/locate/vaccine Incremental costs of introducing jet injection technology for delivery of routine childhood vaccinations: Comparative analysis from Brazil, India, and South Africa Ulla K. Griffiths a,∗, Andreia C. Santos a, Neeti Nundy b, Erica Jacoby b, Dipika Matthias b a London School of Hygiene and Tropical Medicine, Tavistock Place, London WC1H 9SH, UK b PATH, 2201 Westlake Avenue, Suite 200, Seattle, WA 98121, USA article info abstract Article history: Background: Disposable-syringe jet injectors (DSJIs) have the potential to deliver vaccines safely and Received 14 May 2010 affordably to millions of children around the world. We estimated the incremental costs of transitioning Received in revised form 9 November 2010 from needles and syringes to delivering childhood vaccines with DSJIs in Brazil, India, and South Africa. Accepted 15 November 2010 Methods: Two scenarios were assessed: (1) DSJI delivery of all vaccines at current dose and depth; (2) a Available online 27 November 2010 change to intradermal (ID) delivery with DSJIs for hepatitis B and yellow fever vaccines, while the other vaccines are delivered by DSJIs at current dose and depth. The main advantage of ID delivery is that only Keywords: a small fraction of the standard dose may be needed to obtain an immune response similar to that of Vaccine Jet injector subcutaneous or intramuscular injection. Cost categories included were vaccines, injection equipment, Costs waste management, and vaccine transport. Some delivery cost items, such as training and personnel Brazil were excluded as were treatment cost savings caused by a reduction in diseases transmitted due to India unsafe injections. -

Curriculum Vitae
Curriculum Vitae Name: Kenneth Darren Katz, M.D., FAAEM, FACMT Business Address: Department of Emergency Medicine Lehigh Valley Health Network 1240 South Cedar Crest Suite 214 Allentown PA 18103 Education and Training Undergraduate: 08/1988 – 05/1992 Yale University BA - Biology New Haven, CT Graduate: 06/1992 – 06/1996 State University of New York MD Stony Brook School of Medicine Post-Graduate: 07/1996 – 06/2001 Christiana Care Health Systems Resident in Emergency and Newark, DE Internal Medicine 07/2001 – 06/2003 Good Samaritan Regional Medical Toxicology Fellowship Medical Center Phoenix, AZ 07/1997 – 08/1997 Dr. Phillip Heinegg Family practice externship Yonkers, NY Appointments and Positions Academic: 01/2015-present Philadelphia College Osteopathic Medicine Clinical Assistant Professor 07/2013- present Lehigh Valley Health Network Core Faculty Department of Emergency Medicine 07/2010- 6/2013 Department of Internal Medicine Adjunct Asst. Professor West Virginia University School of Medicine 06/2007- 6/2013 University of Pittsburgh Division Chief Department of Emergency Medicine Division of Medical Toxicology 06/2005- 12/2012 Pittsburgh Poison Center Medical Director 10/2012 – 6/2013 University of Pittsburgh Associate Professor Department of Emergency Medicine School of Medicine 07/2004 - 10/2012 University of Pittsburgh Assistant Professor Department of Emergency Medicine School of Medicine 07/2004 -01/2009 University of Pittsburgh Fellowship Director Department of Emergency Medicine Division of Medical Toxicology 7/2003 – 6/2004 University of Pittsburgh Clinical Instructor Department of Emergency Medicine School of Medicine Non-Academic: 06/2007 - present St. Margaret’s Hospital Staff Physician Emergency Department UPMC Health System Pittsburgh, PA 07/2004 – present University of Pittsburgh Staff Physician Department of Emergency Medicine 07/2003 – present University of Pittsburgh Medical Toxicologist 2 Curriculum Vitae Kenneth D. -
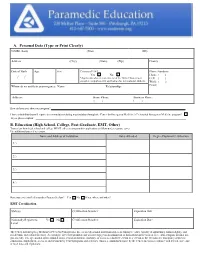
Application Packet
A. Personal Data (Type or Print Clearly) NAME (Last) (First) (MI) Address (City) (State) (Zip) County Date of Birth Age Sex Citizen of US* Phone Numbers: Yes No Home: ( ) / / *Applicants who are not citizens of the United States must Cell: ( ) complete a supplemental application for international students. Work: ( ) Whom do we notify in an emergency: Name: Relationship: Email: Address: Home Phone: Business Phone: ( ) ( ) How did you hear about our program? I have a disability that will require accommodations during matriculation through the Center for Emergency Medicine’s Prehospital Emergency Medicine program? If yes, please explain: B. Education (High School, College, Post-Graduate, EMT, Other) Transcripts from high school and college MUST either accompany this application or follow under separate cover. Use additional paper if necessary. Name and Address of Institution Dates Attended Degree/Diploma/Certification 1.) 2.) 3.) 4.) Have you ever enrolled in another Paramedic class? Yes No If yes, where and when? EMT Certification State(s): Certification Number: Expiration Date: Nationally Registered: Yes No Certification Number: Expiration Date: Level: The Center for Emergency Medicine of Western Pennsylvania, Inc., as an educational institution and as an employer, values equality of opportunity, human dignity, and racial/ethnic and cultural diversity. Accordingly, the Center prohibits and will not engage in discrimination or harassment on the basis of race, color, religion, national ori- gin, ancestry, sex, age, martial status, familial status, sexual orientation, disability, or status as a disabled veteran or a veteran of the Vietnam era. This policy applies to admissions, employment, access to and treatment by Center programs and activities. -
ANNNNNNNNNNNNNNNNNNNN 100A 006 Left Eye Input Right Eye Input
US 20190175049A1 ( 19) United States (12 ) Patent Application Publication (10 ) Pub. No. : US 2019 /0175049 A1 Welling ( 43 ) Pub . Date : Jun . 13 , 2019 ( 54 ) TECHNIQUES FOR ANALYZING (52 ) U . S . CI. NON -VERBAL MARKERS OF CONDITIONS CPC . .. A61B 5 /04842 (2013 . 01 ) ; A61B 5 / 7289 USING ELECTROPHYSIOLOGICAL DATA (2013 . 01) ; A61B 5 /0478 ( 2013 .01 ) ; A61B 5 /7225 ( 2013. 01 ) ; G06N 20 / 10 (2019 .01 ) (71 ) Applicant: Massachusetts Institute of Technology , Cambridge , MA (US ) ( 57 ) ABSTRACT (72 ) Inventor : Caroline Welling, Hanover, NH (US ) Embodiments related to analyzing brain activity of a subject to identify signs associated with binocular rivalry . Sensed ( 21 ) Appl. No. : 16 / 206, 639 electrical activity of a subject' s brain is received over a time period while the subject is exposed to a visual stimulus. The ( 22 ) Filed : Nov. 30 , 2018 sensed electrical activity comprises a first frequency band Related U . S . Application Data associated with a first frequency of a first image presented to the subject ' s left eye , a second frequency band associated (60 ) Provisional application No .62 / 593 , 535, filed on Dec . with a second frequency of a second image presented to the 1 , 2017 subject ' s right eye . A set of events in the time period is determined based on the frequency bands, wherein an event Publication Classification is associated with a change from a previous perceptual event (51 ) Int. Ci. to a new perceptual event. A metric for the subject is A61B 5 /0484 ( 2006 .01 ) determined based on the set of events . The metric is ana A61B 5 /00 ( 2006 .01 ) lyzed to determine whether the subject exhibits signs asso GO6N 20 / 10 (2006 .01 ) ciated with a condition that is associated with binocular A61B 5 /0478 ( 2006 .01 ) rivalry . -

Effect of Repeated Gaboxadol Administration on Night Sleep and Next-Day Performance in Healthy Elderly Subjects
Neuropsychopharmacology (2005) 30, 833–841 & 2005 Nature Publishing Group All rights reserved 0893-133X/05 $30.00 www.neuropsychopharmacology.org Effect of Repeated Gaboxadol Administration on Night Sleep and Next-Day Performance in Healthy Elderly Subjects 1 2 ,3 1 Stefan Mathias , Josef Zihl , Axel Steiger* and Marike Lancel 1Section of Sleep Pharmacology, Max-Planck-Institute of Psychiatry, Munich, Germany; 2Section of Neuropsychology, Max-Planck-Institute of Psychiatry, Munich, Germany; 3Department of Psychiatry, Max-Planck-Institute of Psychiatry, Munich, Germany Aging is associated with dramatic reductions in sleep continuity and sleep intensity. Since gaboxadol, a selective GABAA receptor agonist, has been demonstrated to improve sleep consolidation and promote deep sleep, it may be an effective hypnotic, particularly for elderly patients with insomnia. In the present study, we investigated the effects of subchronic gaboxadol administration on nocturnal sleep and its residual effects during the next days in elderly subjects. This was a randomized, double-blind, placebo-controlled, balanced crossover study in 10 healthy elderly subjects without sleep complaints. The subjects were administered either placebo or 15 mg gaboxadol hydrochloride at bedtime on three consecutive nights. Sleep was recorded during each night from 2300 to 0700 h and tests assessing attention (target detection, stroop test) and memory function (visual form recognition, immediate word recall, digit span) were applied at 0900, 1400, and 1700 h during the following days. Compared with placebo, gaboxadol significantly shortened subjective sleep onset latency and increased self-rated sleep intensity and quality. Polysomnographic recordings showed that it significantly decreased the number of awakenings, the amount of intermittent wakefulness, and stage 1, and increased slow wave sleep and stage 2. -

GABA Receptors
D Reviews • BIOTREND Reviews • BIOTREND Reviews • BIOTREND Reviews • BIOTREND Reviews Review No.7 / 1-2011 GABA receptors Wolfgang Froestl , CNS & Chemistry Expert, AC Immune SA, PSE Building B - EPFL, CH-1015 Lausanne, Phone: +41 21 693 91 43, FAX: +41 21 693 91 20, E-mail: [email protected] GABA Activation of the GABA A receptor leads to an influx of chloride GABA ( -aminobutyric acid; Figure 1) is the most important and ions and to a hyperpolarization of the membrane. 16 subunits with γ most abundant inhibitory neurotransmitter in the mammalian molecular weights between 50 and 65 kD have been identified brain 1,2 , where it was first discovered in 1950 3-5 . It is a small achiral so far, 6 subunits, 3 subunits, 3 subunits, and the , , α β γ δ ε θ molecule with molecular weight of 103 g/mol and high water solu - and subunits 8,9 . π bility. At 25°C one gram of water can dissolve 1.3 grams of GABA. 2 Such a hydrophilic molecule (log P = -2.13, PSA = 63.3 Å ) cannot In the meantime all GABA A receptor binding sites have been eluci - cross the blood brain barrier. It is produced in the brain by decarb- dated in great detail. The GABA site is located at the interface oxylation of L-glutamic acid by the enzyme glutamic acid decarb- between and subunits. Benzodiazepines interact with subunit α β oxylase (GAD, EC 4.1.1.15). It is a neutral amino acid with pK = combinations ( ) ( ) , which is the most abundant combi - 1 α1 2 β2 2 γ2 4.23 and pK = 10.43. -

Gaboxadol Normalizes Behavioral Abnormalities in a Mouse Model of Fragile X Syndrome
ORIGINAL RESEARCH published: 25 June 2019 doi: 10.3389/fnbeh.2019.00141 Gaboxadol Normalizes Behavioral Abnormalities in a Mouse Model of Fragile X Syndrome Patricia Cogram 1,2,3,4, Robert M. J. Deacon 1,2,3,4, Jennifer L. Warner-Schmidt 5, Melanie J. von Schimmelmann 6, Brett S. Abrahams 6,7 and Matthew J. During 6,8* 1FRAXA-DVI, FRAXA Research Foundation, Boston, MA, United States, 2Centre for Systems Biotechnology, Biomedicine Division, Fraunhofer-Gesellschaft, Santiago, Chile, 3GEN.DDI Limited, London, United Kingdom, 4Institute of Ecology and Biodiversity (IEB), University of Chile, Santiago, Chile, 5NeuroJenic Consulting, LLC, Garden City, NY, United States, 6Ovid Therapeutics, New York, NY, United States, 7Department of Genetics and Neuroscience, Albert Einstein College of Medicine, Bronx, NY, United States, 8Department of Neurological Surgery and Molecular Virology, Immunology and Medical Genetics, Ohio State University College of Medicine, Columbus, OH, United States Fragile X syndrome (FXS) is the most common inherited form of intellectual disability and autism. FXS is also accompanied by attention problems, hyperactivity, anxiety, aggression, poor sleep, repetitive behaviors, and self-injury. Recent work supports the role of g-aminobutyric-acid (GABA), the primary inhibitory neurotransmitter in the brain, in mediating symptoms of FXS. Deficits in GABA machinery have been observed in a mouse model of FXS, including a loss of tonic inhibition in the amygdala, which is Edited by: Martine Ammassari-Teule, mediated by extrasynaptic GABAA receptors. Humans with FXS also show reduced Italian National Research Council GABAA receptor availability. Here, we sought to evaluate the potential of gaboxadol (CNR), Italy (also called OV101 and THIP), a selective and potent agonist for delta-subunit-containing Reviewed by: extrasynaptic GABA receptors (dSEGA), as a therapeutic agent for FXS by assessing Giulia Poggi, A University of Zurich, Switzerland its ability to normalize aberrant behaviors in a relatively uncharacterized mouse model Valerie J. -

Ligand-Gated Ion Channels' British Journal of Pharmacology, Vol
Edinburgh Research Explorer The Concise Guide to PHARMACOLOGY 2015/16 Citation for published version: Alexander, SP, Peters, JA, Kelly, E, Marrion, N, Benson, HE, Faccenda, E, Pawson, AJ, Sharman, JL, Southan, C, Davies, JA & CGTP Collaborators 2015, 'The Concise Guide to PHARMACOLOGY 2015/16: Ligand-gated ion channels' British Journal of Pharmacology, vol. 172, no. 24, pp. 5870-5903. DOI: 10.1111/bph.13350 Digital Object Identifier (DOI): 10.1111/bph.13350 Link: Link to publication record in Edinburgh Research Explorer Document Version: Publisher's PDF, also known as Version of record Published In: British Journal of Pharmacology General rights Copyright for the publications made accessible via the Edinburgh Research Explorer is retained by the author(s) and / or other copyright owners and it is a condition of accessing these publications that users recognise and abide by the legal requirements associated with these rights. Take down policy The University of Edinburgh has made every reasonable effort to ensure that Edinburgh Research Explorer content complies with UK legislation. If you believe that the public display of this file breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. Download date: 05. Apr. 2019 S.P.H. Alexander et al. The Concise Guide to PHARMACOLOGY 2015/16: Ligand-gated ion channels. British Journal of Pharmacology (2015) 172, 5870–5903 THE CONCISE GUIDE TO PHARMACOLOGY 2015/16: Ligand-gated ion channels Stephen PH Alexander1, -

For Nexplanon® Insertion and Removal G
Wilson et al. Contraception and Reproductive Medicine (2020) 5:1 Contraception and https://doi.org/10.1186/s40834-020-00104-x Reproductive Medicine RESEARCH Open Access Comparison of traditional anesthesia method and jet injector anesthesia method (MadaJet XL®) for Nexplanon® insertion and removal G. Anthony Wilson* , Julie W. Jeter, William S. Dabbs, Amy Barger Stevens, Robert E. Heidel and Shaunta’ M. Chamberlin Abstract Background: This study compared a needle-free anesthesia method with traditional local anesthesia for insertion and removal of Nexplanon® long-acting removable contraceptive device. In our clinic, patients often avoid this highly effective form of contraception due to fear of needles. We sought to determine if patients perceived a difference in pain with the injection, anxiety level or pain with the procedure when local anesthesia was given with a needle v/s a needle-free jet injector device. Methods: Patients were randomly assigned to one of two groups: jet injector or needle lidocaine delivery. Outcomes were ease of use, patient anxiety level, painfulness, and efficacy of anesthesia method. Results: Patient pain perception with administration of jet injector lidocaine was statistically lower than traditional needle with no difference in anxiety or ease of use, or efficacy of the anesthesia. Conclusion: The jet injector device is a reasonable alternative to needle injection delivery of anesthesia prior to insertion/removal of Nexplanon® device. Further studies may determine whether this needle-free alternative for administration of local anesthetic would result in more women choosing Nexplanon® as a contraceptive method. Keywords: Local anesthetic, Nexplanon®, Patient anxiety Background injection of lidocaine differed between the methods of As with many procedures [1, 2], patients often cite a fear delivery, and whether the presence or absence of needles of needles as a major reason to decline Nexplanon® in the anesthesia method affected patient anxiety level. -
Technical Considerations for Pen, Jet, and Related Injectors Intended for Use with Drugs and Biological Products
Guidance for Industry and FDA Staff: Technical Considerations for Pen, Jet, and Related Injectors Intended for Use with Drugs and Biological Products Additional copies are available from: Office of Combination Products Office of Special Medical Programs Office of the Commissioner Food and Drug Administration 10903 New Hampshire Avenue, WO-32 Hub 5129 Silver Spring, MD 20993 (Tel) 301-796-8930 (Fax) 301-796-8619 http://www.fda.gov/CombinationProducts/default.htm This document finalizes the draft guidance issued in April 2009. For questions regarding this document, contact the Office of Combination Products at [email protected] or Patricia Y. Love, MD at 301-796-8933 or [email protected] U.S. Department of Health and Human Services Food and Drug Administration Center for Devices and Radiological Health, Center for Drug Evaluation Research, Center for Biologics Evaluation and Research, and Office of Combination Products in the Office of the Commissioner June 2013 Contains Nonbinding Recommendations Table of Contents INTRODUCTION.....................................................................................................................3 BACKGROUND .......................................................................................................................4 SECTION I: SCIENTIFIC AND TECHNICAL CONSIDERATIONS.............................5 A. INJECTOR DESCRIPTION .............................................................................................5 B. DESIGN FEATURES.........................................................................................................9 -

A Comprehensive Guide Ram Roth Elizabeth A.M. Frost Clifford Gevirtz
The Role of Anesthesiology in Global Health A Comprehensive Guide Ram Roth Elizabeth A.M. Frost Cli ord Gevirtz Editors Carrie L.H. Atcheson Associate Editor 123 The Role of Anesthesiology in Global Health Ram Roth • Elizabeth A.M. Frost Clifford Gevirtz Editors Carrie L.H. Atcheson Associate Editor The Role of Anesthesiology in Global Health A Comprehensive Guide Editors Ram Roth Elizabeth A.M. Frost Department of Anesthesiology Department of Anesthesiology Icahn School of Medicine at Mount Sinai Icahn School of Medicine at Mount Sinai New York , NY , USA New York , NY , USA Clifford Gevirtz Department of Anesthesiology LSU Health Sciences Center New Orleans , LA , USA Associate Editor Carrie L.H. Atcheson Oregon Anesthesiology Group Department of Anesthesiology Adventist Medical Center Portland , OR , USA ISBN 978-3-319-09422-9 ISBN 978-3-319-09423-6 (eBook) DOI 10.1007/978-3-319-09423-6 Springer Cham Heidelberg New York Dordrecht London Library of Congress Control Number: 2014956567 © Springer International Publishing Switzerland 2015 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifi cally the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfi lms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. Exempted from this legal reservation are brief excerpts in connection with reviews or scholarly analysis or material supplied specifi cally for the purpose of being entered and executed on a computer system, for exclusive use by the purchaser of the work. -

Growth Hormone Treatment Without a Needle Using the Preci-Jet 50
Archives of Disease in Childhood 1997;76:65–67 65 Growth hormone treatment without a needle Arch Dis Child: first published as 10.1136/adc.76.1.65 on 1 January 1997. Downloaded from using the Preci-Jet 50 transjector P Bareille, M MacSwiney, A Albanese, C De Vile, R Stanhope Abstract Patients and methods A new delivery system (Preci-Jet 50) Twenty eight patients (11 girls, 17 boys) were which administers growth hormone randomly selected from the endocrine clinic at through the skin using high pressure and Great Ormond Street Hospital for Children. without a needle was evaluated. This All patients were receiving growth hormone device was inconvenient and painful com- treatment, 19 through an autoinjector and nine pared with a pen injection system. The with needles and syringes. None was using a conclusion is that the Preci-Jet is not the pen injector system at that time but nine had used one previously. The exclusion criteria panacea for solving the problem of com- were bleeding disorders and diseases of colla- pliance with subcutaneous growth hor- gen synthesis. Mean age was 10.1 (range mone injections. 5.7–16.7) years. The growth hormone dose ( 1997;76:65–67) Arch Dis Child range was from 15 to 30 IU/m2 body surface area/week. The subjects were randomly subdi- Keywords: growth hormone treatment; transcutaneous high pressure administration (jet); needle phobia. vided into two groups, A and B. Sex distribu- tion was similar in both groups but mean age diVered, with values of 8.7 and 11.2 years in groups A and B respectively.