Disease Mechanisms in Inherited Neuropathies
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supplemental Material Table of Contents
Supplemental material Table of Contents Detailed Materials and Methods ......................................................................................................... 2 Perioperative period ........................................................................................................................... 2 Ethical aspects ................................................................................................................................... 4 Evaluation of heart failure ................................................................................................................. 4 Sample preparation for ANP mRNA expression .................................................................................. 5 Sample preparation for validative qRT-PCR (Postn, Myh7, Gpx3, Tgm2) ............................................ 6 Tissue fibrosis .................................................................................................................................... 7 Ventricular remodeling and histological tissue preservation ................................................................ 8 Evaluation of the histological preservation of cardiac tissue ................................................................ 9 Sample preparation and quantitative label-free proteomics analyses .................................................. 10 Statistical methods ........................................................................................................................... 12 References ........................................................................................................................................ -

The National Economic Burden of Rare Disease Study February 2021
Acknowledgements This study was sponsored by the EveryLife Foundation for Rare Diseases and made possible through the collaborative efforts of the national rare disease community and key stakeholders. The EveryLife Foundation thanks all those who shared their expertise and insights to provide invaluable input to the study including: the Lewin Group, the EveryLife Community Congress membership, the Technical Advisory Group for this study, leadership from the National Center for Advancing Translational Sciences (NCATS) at the National Institutes of Health (NIH), the Undiagnosed Diseases Network (UDN), the Little Hercules Foundation, the Rare Disease Legislative Advocates (RDLA) Advisory Committee, SmithSolve, and our study funders. Most especially, we thank the members of our rare disease patient and caregiver community who participated in this effort and have helped to transform their lived experience into quantifiable data. LEWIN GROUP PROJECT STAFF Grace Yang, MPA, MA, Vice President Inna Cintina, PhD, Senior Consultant Matt Zhou, BS, Research Consultant Daniel Emont, MPH, Research Consultant Janice Lin, BS, Consultant Samuel Kallman, BA, BS, Research Consultant EVERYLIFE FOUNDATION PROJECT STAFF Annie Kennedy, BS, Chief of Policy and Advocacy Julia Jenkins, BA, Executive Director Jamie Sullivan, MPH, Director of Policy TECHNICAL ADVISORY GROUP Annie Kennedy, BS, Chief of Policy & Advocacy, EveryLife Foundation for Rare Diseases Anne Pariser, MD, Director, Office of Rare Diseases Research, National Center for Advancing Translational Sciences (NCATS), National Institutes of Health Elisabeth M. Oehrlein, PhD, MS, Senior Director, Research and Programs, National Health Council Christina Hartman, Senior Director of Advocacy, The Assistance Fund Kathleen Stratton, National Academies of Science, Engineering and Medicine (NASEM) Steve Silvestri, Director, Government Affairs, Neurocrine Biosciences Inc. -
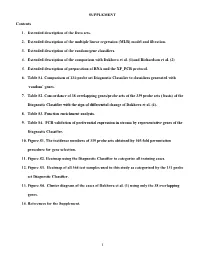
MLR) Model and Filtration
SUPPLEMENT Contents 1. Extended description of the Data sets. 2. Extended description of the multiple linear regression (MLR) model and filtration. 3. Extended description of the random-gene classifiers. 4. Extended description of the comparison with Dakhova et al. (1)and Richardson et al. (2) 5. Extended description of preparation of RNA and the XP_PCR protocol. 6. Table S1. Comparison of 131-probe set Diagnostic Classifier to classifiers generated with ‘random’ genes. 7. Table S2. Concordance of 38 overlapping genes/probe sets of the 339 probe sets ( basis) of the Diagnostic Classifier with the sign of differential change of Dakhova et al. (1). 8. Table S3. Function enrichment analysis. 9. Table S4. PCR validation of preferential expression in stroma by representative genes of the Diagnostic Classifier. 10. Figure S1. The incidence numbers of 339 probe sets obtained by 105-fold permutation procedure for gene selection. 11. Figure S2. Heatmap using the Diagnostic Classifier to categorize all training cases. 12. Figure S3. Heatmap of all 364 test samples used in this study as categorized by the 131 probe set Diagnostic Classifier. 13. Figure S4. Cluster diagram of the cases of Dakhova et al. (1) using only the 38 overlapping genes. 14. References for the Supplement. 1 1. Extended description of the Data Sets. Datasets 1 and 2 (Table 1) are based on post-prostatectomy frozen tissue samples obtained by informed consent using IRB-approved and HIPPA-compliant protocols. All tissues, except where noted, were collected at surgery and escorted to pathology for expedited review, dissection, and snap freezing in liquid nitrogen. -

Genome-Wide Analyses Identify KIF5A As a Novel ALS Gene
This is a repository copy of Genome-wide Analyses Identify KIF5A as a Novel ALS Gene.. White Rose Research Online URL for this paper: http://eprints.whiterose.ac.uk/129590/ Version: Accepted Version Article: Nicolas, A, Kenna, KP, Renton, AE et al. (210 more authors) (2018) Genome-wide Analyses Identify KIF5A as a Novel ALS Gene. Neuron, 97 (6). 1268-1283.e6. https://doi.org/10.1016/j.neuron.2018.02.027 Reuse This article is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs (CC BY-NC-ND) licence. This licence only allows you to download this work and share it with others as long as you credit the authors, but you can’t change the article in any way or use it commercially. More information and the full terms of the licence here: https://creativecommons.org/licenses/ Takedown If you consider content in White Rose Research Online to be in breach of UK law, please notify us by emailing [email protected] including the URL of the record and the reason for the withdrawal request. [email protected] https://eprints.whiterose.ac.uk/ Genome-wide Analyses Identify KIF5A as a Novel ALS Gene Aude Nicolas1,2, Kevin P. Kenna2,3, Alan E. Renton2,4,5, Nicola Ticozzi2,6,7, Faraz Faghri2,8,9, Ruth Chia1,2, Janice A. Dominov10, Brendan J. Kenna3, Mike A. Nalls8,11, Pamela Keagle3, Alberto M. Rivera1, Wouter van Rheenen12, Natalie A. Murphy1, Joke J.F.A. van Vugt13, Joshua T. Geiger14, Rick A. Van der Spek13, Hannah A. Pliner1, Shankaracharya3, Bradley N. -

Inherited Neuropathies
407 Inherited Neuropathies Vera Fridman, MD1 M. M. Reilly, MD, FRCP, FRCPI2 1 Department of Neurology, Neuromuscular Diagnostic Center, Address for correspondence Vera Fridman, MD, Neuromuscular Massachusetts General Hospital, Boston, Massachusetts Diagnostic Center, Massachusetts General Hospital, Boston, 2 MRC Centre for Neuromuscular Diseases, UCL Institute of Neurology Massachusetts, 165 Cambridge St. Boston, MA 02114 and The National Hospital for Neurology and Neurosurgery, Queen (e-mail: [email protected]). Square, London, United Kingdom Semin Neurol 2015;35:407–423. Abstract Hereditary neuropathies (HNs) are among the most common inherited neurologic Keywords disorders and are diverse both clinically and genetically. Recent genetic advances have ► hereditary contributed to a rapid expansion of identifiable causes of HN and have broadened the neuropathy phenotypic spectrum associated with many of the causative mutations. The underlying ► Charcot-Marie-Tooth molecular pathways of disease have also been better delineated, leading to the promise disease for potential treatments. This chapter reviews the clinical and biological aspects of the ► hereditary sensory common causes of HN and addresses the challenges of approaching the diagnostic and motor workup of these conditions in a rapidly evolving genetic landscape. neuropathy ► hereditary sensory and autonomic neuropathy Hereditary neuropathies (HN) are among the most common Select forms of HN also involve cranial nerves and respiratory inherited neurologic diseases, with a prevalence of 1 in 2,500 function. Nevertheless, in the majority of patients with HN individuals.1,2 They encompass a clinically heterogeneous set there is no shortening of life expectancy. of disorders and vary greatly in severity, spanning a spectrum Historically, hereditary neuropathies have been classified from mildly symptomatic forms to those resulting in severe based on the primary site of nerve pathology (myelin vs. -

The Intrinsically Disordered Proteins of Myelin in Health and Disease
cells Review Flexible Players within the Sheaths: The Intrinsically Disordered Proteins of Myelin in Health and Disease Arne Raasakka 1 and Petri Kursula 1,2,* 1 Department of Biomedicine, University of Bergen, Jonas Lies vei 91, NO-5009 Bergen, Norway; [email protected] 2 Faculty of Biochemistry and Molecular Medicine & Biocenter Oulu, University of Oulu, Aapistie 7A, FI-90220 Oulu, Finland * Correspondence: [email protected] Received: 30 January 2020; Accepted: 16 February 2020; Published: 18 February 2020 Abstract: Myelin ensheathes selected axonal segments within the nervous system, resulting primarily in nerve impulse acceleration, as well as mechanical and trophic support for neurons. In the central and peripheral nervous systems, various proteins that contribute to the formation and stability of myelin are present, which also harbor pathophysiological roles in myelin disease. Many myelin proteins have common attributes, including small size, hydrophobic segments, multifunctionality, longevity, and regions of intrinsic disorder. With recent advances in protein biophysical characterization and bioinformatics, it has become evident that intrinsically disordered proteins (IDPs) are abundant in myelin, and their flexible nature enables multifunctionality. Here, we review known myelin IDPs, their conservation, molecular characteristics and functions, and their disease relevance, along with open questions and speculations. We place emphasis on classifying the molecular details of IDPs in myelin, and we correlate these with their various functions, including susceptibility to post-translational modifications, function in protein–protein and protein–membrane interactions, as well as their role as extended entropic chains. We discuss how myelin pathology can relate to IDPs and which molecular factors are potentially involved. Keywords: myelin; intrinsically disordered protein; multiple sclerosis; peripheral neuropathies; myelination; protein folding; protein–membrane interaction; protein–protein interaction 1. -

Ɑ6ß1 Andɑ7ß1 Integrins Are Required in Schwann Cells to Sort
The Journal of Neuroscience, November 13, 2013 • 33(46):17995–18007 • 17995 Cellular/Molecular ␣61 and ␣71 Integrins Are Required in Schwann Cells to Sort Axons Marta Pellegatta,1,2 Ade`le De Arcangelis,3 Alessandra D’Urso,1 Alessandro Nodari,1 Desire´e Zambroni,1 Monica Ghidinelli,1,2 Vittoria Matafora,1 Courtney Williamson,2 Elisabeth Georges-Labouesse,3† Jordan Kreidberg,4 Ulrike Mayer,5 Karen K. McKee,6 Peter D. Yurchenco,6 Angelo Quattrini,1 Lawrence Wrabetz,1,2 and Maria Laura Feltri1,2 1San Raffaele Scientific Institute, Milano 20132, Italy, 2Hunter James Kelly Research Institute, University at Buffalo, State University of New York, New York 14203, 3Development and Stem Cells Program, Institut de Ge´ne´tique et de Biologie Mole´culaire et Cellulaire, Centre National de la Recherche Scientifique, Unite´ Mixte de Recherche 7104, Institut National de la Sante´ et de la Recherche Me´dicale U964, Universite´ de Strasbourg, Illkirch 67404, France, 4Department of Medicine, Children’s Hospital Boston and Department of Pediatrics, Harvard Medical School, Boston, Massachusetts 02115, 5Biomedical Research Centre, School of Biological Sciences, University of East Anglia, Norwich NR4 7TJ, United Kingdom, and 6Robert Wood Johnson Medical School, Piscataway, New Jersey, New Jersey 08854 During development, Schwann cells extend lamellipodia-like processes to segregate large- and small-caliber axons during the process of radial sorting. Radial sorting is a prerequisite for myelination and is arrested in human neuropathies because of laminin deficiency. Experiments in mice using targeted mutagenesis have confirmed that laminins 211, 411, and receptors containing the 1 integrin subunit are required for radial sorting; however, which of the 11 ␣ integrins that can pair with 1 forms the functional receptor is unknown. -

Peripheral Neuropathy in Complex Inherited Diseases: an Approach To
PERIPHERAL NEUROPATHY IN COMPLEX INHERITED DISEASES: AN APPROACH TO DIAGNOSIS Rossor AM1*, Carr AS1*, Devine H1, Chandrashekar H2, Pelayo-Negro AL1, Pareyson D3, Shy ME4, Scherer SS5, Reilly MM1. 1. MRC Centre for Neuromuscular Diseases, UCL Institute of Neurology and National Hospital for Neurology and Neurosurgery, London, WC1N 3BG, UK. 2. Lysholm Department of Neuroradiology, National Hospital for Neurology and Neurosurgery, London, WC1N 3BG, UK. 3. Unit of Neurological Rare Diseases of Adulthood, Carlo Besta Neurological Institute IRCCS Foundation, Milan, Italy. 4. Department of Neurology, University of Iowa, 200 Hawkins Drive, Iowa City, IA 52242, USA 5. Department of Neurology, University of Pennsylvania, Philadelphia, PA 19014, USA. * These authors contributed equally to this work Corresponding author: Mary M Reilly Address: MRC Centre for Neuromuscular Diseases, 8-11 Queen Square, London, WC1N 3BG, UK. Email: [email protected] Telephone: 0044 (0) 203 456 7890 Word count: 4825 ABSTRACT Peripheral neuropathy is a common finding in patients with complex inherited neurological diseases and may be subclinical or a major component of the phenotype. This review aims to provide a clinical approach to the diagnosis of this complex group of patients by addressing key questions including the predominant neurological syndrome associated with the neuropathy e.g. spasticity, the type of neuropathy, and the other neurological and non- neurological features of the syndrome. Priority is given to the diagnosis of treatable conditions. Using this approach, we associated neuropathy with one of three major syndromic categories - 1) ataxia, 2) spasticity, and 3) global neurodevelopmental impairment. Syndromes that do not fall easily into one of these three categories can be grouped according to the predominant system involved in addition to the neuropathy e.g. -

Open Full Page
Published OnlineFirst December 17, 2015; DOI: 10.1158/0008-5472.CAN-15-0884 Cancer Tumor and Stem Cell Biology Research Eva1 Maintains the Stem-like Character of Glioblastoma-Initiating Cells by Activating the Noncanonical NF-kB Signaling Pathway Naoki Ohtsu1, Yuka Nakatani2, Daisuke Yamashita3, Shiro Ohue3, Takanori Ohnishi3,and Toru Kondo1,2 Abstract Glioblastoma (GBM)–initiating cells (GIC) are a tumorigenic as Eva1 overexpression enhanced these properties. Eva1 deficien- subpopulation that are resistant to radio- and chemotherapies cy was also associated with decreased expression of stemness- and are the source of disease recurrence. Therefore, the identifi- related genes, indicating a requirement for Eva1 in maintaining cation and characterization of GIC-specific factors is critical GIC pluripotency. We further demonstrate that Eva1 induced GIC toward the generation of effective GBM therapeutics. In this study, proliferation through the activation of the RelB-dependent non- we investigated the role of epithelial V-like antigen 1 (Eva1, also canonical NF-kB pathway by recruiting TRAF2 to the cytoplasmic known as myelin protein zero-like 2) in stemness and GBM tail. Taken together, our findings highlight Eva1 as a novel tumorigenesis. Eva1 was prominently expressed in GICs in vitro regulator of GIC function and also provide new mechanistic and in stem cell marker (Sox2, CD15, CD49f)-expressing cells insight into the role of noncanonical NF-kB activation in GIC, derived from human GBM tissues. Eva1 knockdown in GICs thus offering multiple potential therapeutic targets for preclinical reduced their self-renewal and tumor-forming capabilities, where- investigation in GBM. Cancer Res; 76(1); 171–81. Ó2015 AACR. -

How Does Protein Zero Assemble Compact Myelin?
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 13 May 2020 doi:10.20944/preprints202005.0222.v1 Peer-reviewed version available at Cells 2020, 9, 1832; doi:10.3390/cells9081832 Perspective How Does Protein Zero Assemble Compact Myelin? Arne Raasakka 1,* and Petri Kursula 1,2 1 Department of Biomedicine, University of Bergen, Jonas Lies vei 91, NO-5009 Bergen, Norway 2 Faculty of Biochemistry and Molecular Medicine & Biocenter Oulu, University of Oulu, Aapistie 7A, FI-90220 Oulu, Finland; [email protected] * Correspondence: [email protected] Abstract: Myelin protein zero (P0), a type I transmembrane protein, is the most abundant protein in peripheral nervous system (PNS) myelin – the lipid-rich, periodic structure that concentrically encloses long axonal segments. Schwann cells, the myelinating glia of the PNS, express P0 throughout their development until the formation of mature myelin. In the intramyelinic compartment, the immunoglobulin-like domain of P0 bridges apposing membranes together via homophilic adhesion, forming a dense, macroscopic ultrastructure known as the intraperiod line. The C-terminal tail of P0 adheres apposing membranes together in the narrow cytoplasmic compartment of compact myelin, much like myelin basic protein (MBP). In mouse models, the absence of P0, unlike that of MBP or P2, severely disturbs the formation of myelin. Therefore, P0 is the executive molecule of PNS myelin maturation. How and when is P0 trafficked and modified to enable myelin compaction, and how disease mutations that give rise to incurable peripheral neuropathies alter the function of P0, are currently open questions. The potential mechanisms of P0 function in myelination are discussed, providing a foundation for the understanding of mature myelin development and how it derails in peripheral neuropathies. -

Supplemental Data
MOLECULAR PHARMACOLOGY Supplemental Data Regulation of M3 Muscarinic Receptor Expression and Function by Transmembrane Protein 147 Erica Rosemond, Mario Rossi, Sara M. McMillin, Marco Scarselli, Julie G. Donaldson, and Jürgen Wess Supplemental Table 1 M3R-interacting proteins identified in a membrane-based yeast two-hybrid screen Accession Protein No. Tetraspanin family CD82 AAB23825 CD9 P21926 CD63 AAV38940 Ubiquitin-associated proteins Small ubiquitin-related modifier 2 precursor (SUMO-1) AAC50996 Small ubiquitin-related modifier 2 precursor (SUMO-2) P61956 UBC protein AAH08955 Ubiquitin C NP_066289 Receptor proteins/Transmembrane proteins AAH01118 / Transmembrane protein 147 BC001118 G protein-coupled receptor 37 NP_005293 NM_016235 / Homo sapiens G protein-coupled receptor, family C, group 5, member B (GPRC5B) AAF05331 Rhodopsin NP_000530 Aquaporin-4 (AQP-4) P55087 Glutamate receptor, ionotropic, N-methyl D-aspartate-associated protein 1 NP_001009184 Sodium channel, voltage gated, type VIII, alpha NP_055006 Transmembrane 9 superfamily member 2 CAH71381 Transmembrane protein 14A AAH19328 Signaling molecules Phosphatidic acid phosphatase type 2C AAP35667 Calmodulin 2 AAH08437 Protein kinase Njmu-R1 AAH54035 2',3'-Cyclic nucleotide 3' phosphodiesterase (CNP) AAH06392 Solute carrier proteins Solute carrier family 39 (zinc transporter), member 3 isoform a NP_653165 Solute carrier family 22 (organic cation transporter), member 17 isoform b NP_057693 Solute carrier family 31 (copper transporters), member 2 NP_001851 Solute carrier family -

Cellular and Molecular Signatures in the Disease Tissue of Early
Cellular and Molecular Signatures in the Disease Tissue of Early Rheumatoid Arthritis Stratify Clinical Response to csDMARD-Therapy and Predict Radiographic Progression Frances Humby1,* Myles Lewis1,* Nandhini Ramamoorthi2, Jason Hackney3, Michael Barnes1, Michele Bombardieri1, Francesca Setiadi2, Stephen Kelly1, Fabiola Bene1, Maria di Cicco1, Sudeh Riahi1, Vidalba Rocher-Ros1, Nora Ng1, Ilias Lazorou1, Rebecca E. Hands1, Desiree van der Heijde4, Robert Landewé5, Annette van der Helm-van Mil4, Alberto Cauli6, Iain B. McInnes7, Christopher D. Buckley8, Ernest Choy9, Peter Taylor10, Michael J. Townsend2 & Costantino Pitzalis1 1Centre for Experimental Medicine and Rheumatology, William Harvey Research Institute, Barts and The London School of Medicine and Dentistry, Queen Mary University of London, Charterhouse Square, London EC1M 6BQ, UK. Departments of 2Biomarker Discovery OMNI, 3Bioinformatics and Computational Biology, Genentech Research and Early Development, South San Francisco, California 94080 USA 4Department of Rheumatology, Leiden University Medical Center, The Netherlands 5Department of Clinical Immunology & Rheumatology, Amsterdam Rheumatology & Immunology Center, Amsterdam, The Netherlands 6Rheumatology Unit, Department of Medical Sciences, Policlinico of the University of Cagliari, Cagliari, Italy 7Institute of Infection, Immunity and Inflammation, University of Glasgow, Glasgow G12 8TA, UK 8Rheumatology Research Group, Institute of Inflammation and Ageing (IIA), University of Birmingham, Birmingham B15 2WB, UK 9Institute of