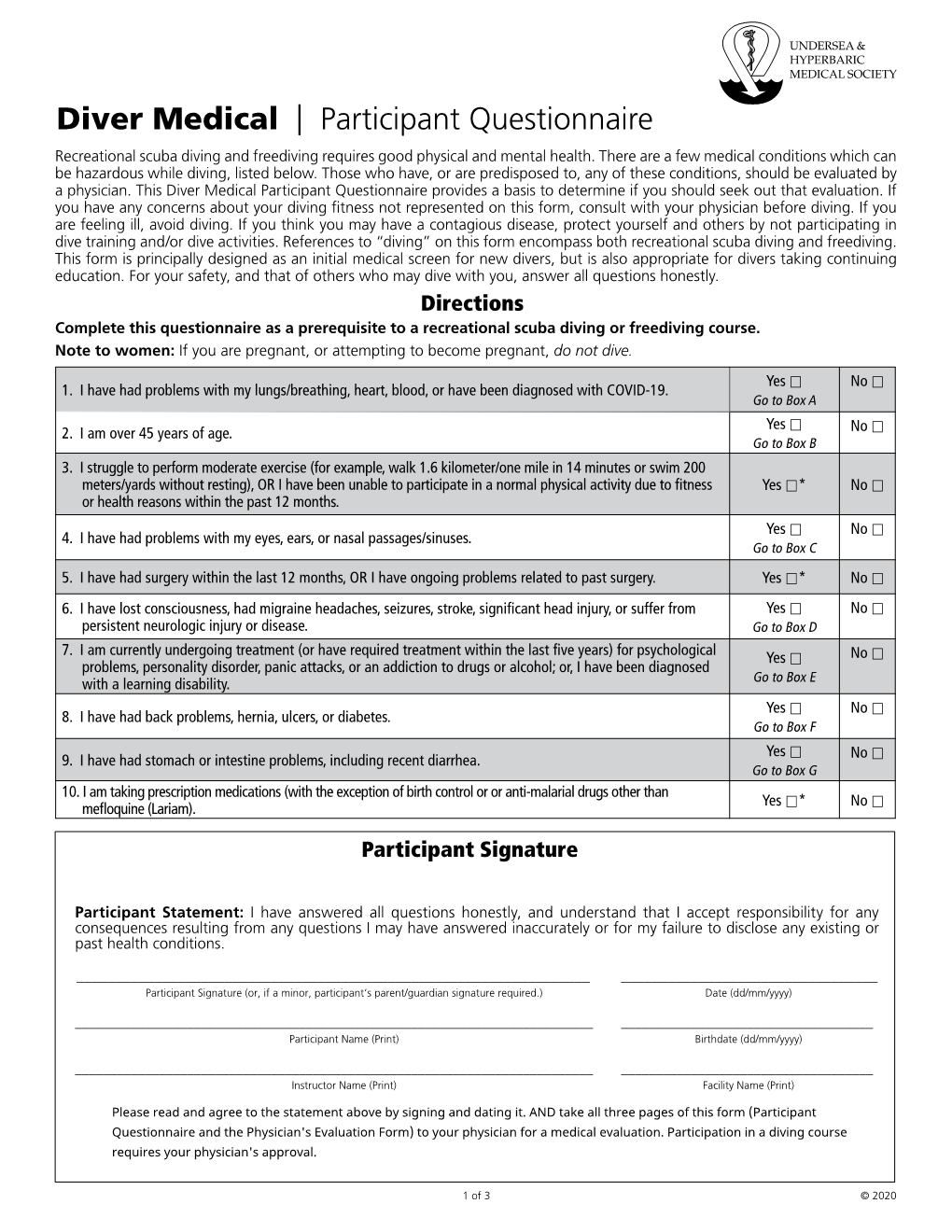
Diver Medical Participant Questionnaire Provides a Basis to Determine If You Should Seek out That Evaluation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nasal Septum Deviation by Age and Sex in a Study Population of Poles
Journal of Rhinolaryngo-Otologies, 2019, 7, 1-6 1 Nasal Septum Deviation by Age and Sex in a Study Population of Poles O. Wojas, P. Szczęsnowicz-Dąbrowska, A. Grzanka, E. Krzych-Fałta* and B . Samoliński Unit of Environmental Hazard Prevention and Allergology, Medical University of Warsaw, Poland Abstract: Introduction: Nasal septum deviation is found in nearly 79% of all autopsies. A displacement of the nasal septum is caused by developmental disorders, which result in growth disproportions between different skeletal structures, as well as hereditary factors, and injuries to the nose and the facial skeleton. Aims: This study aims is to estimate the incidence of nasal septum deviation in a study population of Poles, with a breakdown by age and sex. Subjects and method(s): The people involved in the study were a group of 950 randomly selected residents of a large city. The subjects were aged between 6 and 76 years. The method used in the study was anterior rhinoscopy in combination with clinical history taking. Results: The investigation revealed that the number of cases of nasal septum deviation diagnosed on the basis of anterior rhinoscopy increases steadily with age, from 15% in children aged 7-8 years to 39.7% in adults (p<0.05). The results of the study show that men are more frequently diagnosed with nasal septum deviations than women are (p<0.05). Conclusions: A relatively large percentage of nasal septum deviations was observed in a population of Poles, with a breakdown by age and sex. Keywords: Nasal cavity, nasal septum deviation. INTRODUCTION accompanies and contributes to diseases such as snoring, obstructive sleep apnea syndrome (OSAS) or The nasal cavity, enclosed by the inner surface of the chronic inflammatory paranasal sinus disease [5]. -
Guidance for Divers on Medical Certificates of Fitness to Dive
Guidance for Divers on Medical Certificates of Fitness to Dive Guidance for Divers on Medical Certificates Our Vision: of Fitness to Dive Healthy, safe and productive lives and enterprises May 2019 Cyan 100% Magenta 76% Yellow 0 Black 27% Guidance for Divers on TABLE OF CONTENTS Medical Certificates of Fitness to Dive May 2019 1.0 Introduction .............................................................................2 2.0 Legal Requirements .....................................................................3 3.0 Procedure for Applying for a Medical.....................................................5 4.0 Criteria for Conducting Medicals ........................................................ 6 5.0 Frequency of Medical Assessments, Conditions and Limitations......................... 7 Appendix 1 - Medical Questionnaire .......................................................... 8 Published in November 2019 by the Health and Safety Authority, The Metropolitan Building, James Joyce Street, Dublin 1. ©All rights reserved. r fo Guidance ers on on ers Div es tificat r Ce Medical 1.0 INTRODUCTION e Div to Fitness of May 2019 May 1.1 Under the Safety, Health and Welfare at Work (Diving) Regulations 2018 and 2019 (S.I. No. 254 of 2018 as amended by S.I. No. 180 of 2019), hereafter referred to as the Diving Regulations, a diver must not dive in a diving project unless they hold a valid certificate of medical fitness to dive issued by a medical examiner of divers. These guidelines provide information on the process and the certificates. The guidelines are aimed at divers who dive for work purposes, but the information will also be of interest to diving contractors and diving supervisors. 1.2 Working underwater can be a hostile work environment so fitness to dive is vital. It is important that the diver does not suffer from any medical condition that could affect the safety of themselves or other members of the dive team. -

Respiratory Examination Cardiac Examination Is an Essential Part of the Respiratory Assessment and Vice Versa
Respiratory examination Cardiac examination is an essential part of the respiratory assessment and vice versa. # Subject steps Pictures Notes Preparation: Pre-exam Checklist: A Very important. WIPE Be the one. 1 Wash your hands. Wash your hands in Introduce yourself to the patient, confirm front of the examiner or bring a sanitizer with 2 patient’s ID, explain the examination & you. take consent. Positioning of the patient and his/her (Position the patient in a 3 1 2 Privacy. 90 degree sitting position) and uncover Exposure. full exposure of the trunk. his/her upper body. 4 (if you could not, tell the examiner from the beginning). 3 4 Examination: General appearance: B (ABC2DEVs) Appearance: young, middle aged, or old, Begin by observing the and looks generally ill or well. patient's general health from the end of the bed. Observe the patient's general appearance (age, Around the bed I can't state of health, nutritional status and any other see any medications, obvious signs e.g. jaundice, cyanosis, O2 mask, or chest dyspnea). 1 tube(look at the lateral sides of chest wall), metered dose inhalers, and the presence of a sputum mug. 2 Body built: normal, thin, or obese The patient looks comfortable and he doesn't appear short of breath and he doesn't obviously use accessory muscles or any heard Connections: such as nasal cannula wheezes. To determine this, check for: (mention the medications), nasogastric Dyspnea: Assess the rate, depth, and regularity of the patient's 3 tube, oxygen mask, canals or nebulizer, breathing by counting the respiratory rate, range (16–25 breaths Holter monitor, I.V. -

ECHM-EDTC Educational and Training Standards for Diving and Hyperbaric Medicine 2011
ECHM-EDTC Educational and Training Standards for Diving and Hyperbaric Medicine 2011 EDUCATIONAL AND TRAINING STANDARDS FOR PHYSICIANS IN DIVING AND HYPERBARIC MEDICINE Written by Joint Educational Subcommittee of the European Committee for Hyperbaric Medicine (ECHM) and the European Diving Technical Committee (EDTC) List of content: Foreword ..................................................................................................................................................2 1. Introduction...........................................................................................................................................3 2. Definition of jobs...................................................................................................................................4 3. Training programs ................................................................................................................................6 4. Content of modules ..............................................................................................................................7 5. Standards for course organisation and certification.............................................................................9 5.1. Teaching courses..........................................................................................................................9 5.2. Modules and course organisation.................................................................................................9 5.3. Recognition of an expert.............................................................................................................10 -

DIVING MEDICAL EXAM OVERVIEW for the EXAMINING PHYSICIAN to the EXAMINING PHYSICIAN This Person Requires a Medical Examination T
University of Maine. Department: Safety and Environmental Management Department Page: Appendix 1 Title: Standards for Scientific Diving Certification and Operation of Scientific Revision: 8 Diving Programs Procedure: MP07420 Date Issued: 01/15/2013 DIVING MEDICAL EXAM OVERVIEW FOR THE EXAMINING PHYSICIAN TO THE EXAMINING PHYSICIAN This person requires a medical examination to assess his/her fitness for participation in Scientific Diving activities at the University of Maine. Your evaluation is requested on the attached Medical Evaluation of Fitness for Scuba Diving Report (Appendix 2). The medical exam should be conducted in conjunction with a review of the applicant’s Diving Medical History Form (Appendix 3). If you have questions about diving medicine, you may wish to consult one of the Recommended Physicians with Expertise in Diving Medicine or Selected References in Diving Medicine (Appendix 4). Please contact the UMaine Diving Safety Officer if you have any questions or concerns about diving medicine or the University of Maine standards. Thank you for your assistance. Christopher M. Rigaud, University of Maine Diving Operations Manager/ Diving Safety Officer Department of Safety and Environmental Management Darling Marine Center 193 Clarks Cove Road Walpole, ME 04573 207-563-8273 CONDITIONS WHICH MAY DISQUALIFY CANDIDATES FROM DIVING (Adapted from Bove, 1998) Scuba and other modes of compressed-gas diving can be strenuous and hazardous. A special risk is present if the middle ear, sinuses or lung segments do not readily equalize air pressure changes. The most common cause of distress is eustachian insufficiency. Recent deaths in the scientific diving community have been attributed to cardiovascular disease. -

Training Objectives for a Diving Medical Physician
The Diving Medical Advisory Committee Training Objectives for a Diving Medicine Physician This guidance includes all the training objectives agreed by the Diving Medical Advisory Committee, the European Diving Technology Committee and the European Committee for Hyperbaric Medicine in 2011. Rev 1 - 2013 INTRODUCTION The purpose of this document is to define more closely the training objectives in diving physiology and medicine that need to be met by doctors already fully accredited or board-certified in a clinical speciality to national standards. It is based on topic headings that were originally prepared for a working group of European Diving Technology Committee (EDTC) and the European Committee of Hyperbaric Medicine (ECHM) as a guide for diving medicine some 20 years ago by J.Desola (Spain), T.Nome (Norway) & D.H.Elliott (U.K.). The training now required for medical examiners of working divers and for specialist diving medicine physicians was based on a EDTC/ECHM standard 1999 and subsequently has been enhanced by the Diving Medical Advisory Committee (DMAC), revised and agreed in principle by DMAC, EDTC and ECHM in 2010 and then ratified by EDTC and ECHM in 2011. The requirements now relate to an assessment of competence, the need for some training in occupational medicine, the need for maintenance of those skills by individual ‘refresher training’. Formal recognition of all this includes the need to involve a national authority for medical education. These objectives have been applied internationally to doctors who provide medical support to working divers. (Most recreational instructors and dive guides are, by their employment, working divers and so the guidance includes the relevant aspects of recreational diving. -

Septal Deviation Operation Informed Consent Form
SEPTAL DEVIATION OPERATION INFORMED CONSENT FORM FIRST DOCUMEN RB.FR. PUBLIS REVISION REVISION PAGE 01.02.2010 09.12.2015 1 1/6 T NO 15 HING DATE NO NO DATE Revision Cause: PATIENT’S Name Surname:……………………………………………... Birthdate :…………………………………………. Hospital Admission Date:………………………………. Hospitalization Date:…………………………………… Protocol Number:…………………………………….. Telephone Number:……………………………………… Address:………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… Please read this form carefully and answer the questions. As a result of the examinations, it has been decided that you should undergo surgical intervention because of “septal deviation”. Before the procedure, your doctor will give you information about the course and the different forms of the procedure and the risks involved. Accordingly, you will be free to decide on the interventions. This written form is intended to provide you with basic information about the intervention and associated complications (problems that may occur during or after the procedure). What you should know about your disease: The nasal septum deviation (see figure) occurs due to the development of deformities of the facial bones, as well as fractures of the nasal bone that may occur during birth. If the deviation is causing the following problems, surgery is required: 1. Difficulty in nasal respiration 2. Drying, burning sensation, feeling of foreign body in the throat due to continuous oral breathing 3. Snoring, sleep acnea (occasionally) 4. Head/face ache 5. Recurrent sinusitis, 6. Laryngitis and bronchi inflammation 7. İnfection of the Eustachian tube and tendency to middle ear infections . In some sinus operations and certain types of nasal bleeding, nasal septum deviation surgery may be necessary. SEPTAL DEVIATION OPERATION INFORMED CONSENT FORM FIRST DOCUMEN RB.FR. -

Nasal Endoscopy Findings in Acute and Chronic Rhinosinusitis Patients
420 AMJ September 2017 AMJ. 2017;4(3):420–5 Nasal Endoscopy Findings in Acute and Chronic Rhinosinusitis Patients Stephanie Dharmaputri,1 Lina Lasminingrum,2 Yulia Sofiatin3 1Faculty of Medicine Universitas Padjadjaran, 2Department of Otorhinolaryngology–Head and Neck Surgery Faculty of Medicine Universitas Padjadjaran/Dr. Hasan Sadikin General Hospital Bandung, 3Department of Public Health Faculty of Medicine Universitas Padjadjaran Abstract Background: According to European Position Paper on Rhinosinusitis and Nasal Polyps (EPOS) 2012, rhinosinusitis is diagnosed based on symptoms, nasal endoscopy, and CT scan. The CT scan is the gold standard to diagnose rhinosinusitis, but its high cost and lack of availability become the problems in Indonesia. Hence, nasal endoscopy is a choice to diagnose rhinosinusitis. This study was aimed to describe Methods: This cross-sectional descriptive study was performed using medical record of acute and chronic therhinosinusitis findings of patients.nasal endoscopyin The samples in acute were and chosen chronic with rhinosinusitis. consecutive sampling. Inclusion criteria of this study were patients that underwent nasal endoscopy examination in Otorhinolaryngology–Head and Neck Surgery Clinic Dr. Hasan Sadikin General Hospital Bandung in 2014.The collected data were analyzed in the form of tables. Results: Among 138 patients, the number of female patients (55.1%) was higher than male patients. Majority of the patients (37.5%) were 25–44 years old. Majority of the chief complaint was nasal obstruction (48.6%). The patients with allergic history (48.6%) were higher than patients without allergic history (19.6%). According to nasal endoscopy results, nasal discharge and edema were found in most of the patients (68.8% or nasal septum deviation, were also found on 87.7% patients. -

HANDOUT #1 CONCEPT INTRODUCTION PRESENTATION: PERFUSION Topic Description Definition of Perfusion the Passage of Oxygenated Capi
HANDOUT #1 CONCEPT INTRODUCTION PRESENTATION: PERFUSION Topic Description Definition of Perfusion The passage of oxygenated capillary blood through body tissues. Peripheral perfusion is passage (flow) of blood to the extremities of the body. Central perfusion is passage (flow) of blood to major body organs, including the heart and lungs. Scope of Perfusion Perfusion can be viewed on a continuum as adequate on one end and inadequate, decreased, or impaired on the other. Decreased Perfusion can range from minimal to severe. Ischemia refers to decreased Perfusion, while infarction is complete tissue death due to severe decreased Perfusion. Risk Factors/Populations at Risk for Examples of risk factors or populations at risk Impaired Perfusion for impaired Perfusion can be categorized as modifiable (can be changed) and nonmodifiable (cannot be changed) Modifiable factors include: • Obesity • Lack of physical activity/sedentary lifestyle • Smoking Nonmodifiable factors include age, gender, and race/ethnicity. Groups at risk for impaired Perfusion include those who are of advanced age (due to less elastic arterial vessels as a result of aging) and those who are African American and Hispanic. These racial/ethnic groups are most at risk for chronic diseases that can affect Perfusion such as diabetes mellitus, hypertension, hyperlipidemia, and peripheral vascular disease. The cause of these variations is not known, but dietary and environmental factors may contribute to the higher incidence of chronic disease in these groups. Newborns and infants who have congenital heart anomalies are also at risk for impaired central Perfusion. Many of these defects can be surgically repaired to regain adequate Perfusion. Physiologic Consequences of Impaired Consequences of impaired Perfusion vary Perfusion depending on the degree of impairment. -

Dive Physical Requirements
Dive Physical Requirements Dive physical must be complete and submitted to the school prior to enrollment in the program. • Schedule and complete ADCI Medical History and Examination Forms (included in this packet), ensuring the following tests are conducted: § Audiogram § Visual Acuity § Color Blindness § Complete Blood Count (CBC) § Routine Urinalysis § Spirometry / Pulmonary Function Test (PFT) § Chest X-Ray Results § Ten (10) Panel Drug Test (includes marijuana) • Submit completed ADCI Medical History and Examination Forms, signed by the physician. • Dive physical documents can be scanned and emailed to [email protected], faxed to (858) 309-3510, or mailed to: National University Polytechnic Institute 3570 Aero Court San Diego, CA 92123 Recommended Dive Physicians San Diego Sports Medicine – Sorrento Valley VA San Diego Healthcare System 4010 Sorrento Valley Blvd #300 3350 La Jolla Village Dr. San Diego, CA 92121 San Diego, CA 92161 (858) 793-7860 (858) 552-8585 (800) 331-8387 San Diego Sports Medicine – College Area 6699 Alvarado Road Ste 2100 San Diego, CA 92120 (619) 229-3909 The Dive Physical can be administered by any licensed physician qualified to perform Commercial Diver Medical Examinations. Please call (800) 432-3483 for any questions related to the dive physical or other required documents. International Consensus Standards For Commercial Diving And Underwater Operations 2.4 2.4.3 ADCI MEDICAL HISTORY AND EXAMINATION FORMS Association of Diving Contractors International MEDICAL HISTORY FORM Employer Job Title Date 1. Last Name First Name Middle Name 2. Email Address 3. Date of Birth 4. Gender 5. Last 4 No. of SSN 6. Address (Number, Street) 7. -

What Are the Health Effects from Exposure to Carbon Monoxide?
CO Lesson 2 CARBON MONOXIDE: LESSON TWO What are the Health Effects from Exposure to Carbon Monoxide? LESSON SUMMARY Carbon monoxide (CO) is an odorless, tasteless, colorless and nonirritating Grade Level: 9 – 12 gas that is impossible to detect by an exposed person. CO is produced by the Subject(s) Addressed: incomplete combustion of carbon-based fuels, including gas, wood, oil and Science, Biology coal. Exposure to CO is the leading cause of fatal poisonings in the United Class Time: 1 Period States and many other countries. When inhaled, CO is readily absorbed from the lungs into the bloodstream, where it binds tightly to hemoglobin in the Inquiry Category: Guided place of oxygen. CORE UNDERSTANDING/OBJECTIVES By the end of this lesson, students will have a basic understanding of the physiological mechanisms underlying CO toxicity. For specific learning and standards addressed, please see pages 30 and 31. MATERIALS INCORPORATION OF TECHNOLOGY Computer and/or projector with video capabilities INDIAN EDUCATION FOR ALL Fires utilizing carbon-based fuels, such as wood, produce carbon monoxide as a dangerous byproduct when the combustion is incomplete. Fire was important for the survival of early Native American tribes. The traditional teepees were well designed with sophisticated airflow patterns, enabling fires to be contained within the shelter while minimizing carbon monoxide exposure. However, fire was used for purposes other than just heat and cooking. According to the historian Henry Lewis, Native Americans used fire to aid in hunting, crop management, insect collection, warfare and many other activities. Today, fire is used to heat rocks used in sweat lodges. -

Overview on Deviated Nasal Septum: Simple Review
Review Article Overview on Deviated Nasal Septum: Simple Review Yahia Abdelgawad Elsayed Elboraei1, Asmaa Enad S. Alenazy2*, Alwaleed Oqab N Altimyat2, Abdulaziz Inad S Alanazi3, Najd Mujawwil A Alanazi2, Nouf Abdullah S Alanazi2 1 MBBCh., MSc. & ENT Assistant Professor, Northern Border University, KSA. 2 Faculty of Medicine, Northern Border University, KSA. 3 Emergency Medicine Resident, King Abdulaziz Medical City of National guard, Riyadh, KSA. Abstract Background: Nasal septum deviation (NSD) is a common problem in otolaryngology clinics and constitutes one of the healthy adults' most common anatomical variations. NSD may result in a deviation of either the bony or cartilaginous septum or both, leading to a disruption of the nose's physiological function and a distortion of its shape. Aim: In this review, we will look into the etiology, classification, management, and complications of nasal septum deviation. Methodology: Medline, Google Scholar, EMBASE, and PubMed database searches were performed for articles about the most significant recent developments in classification, etiology, and management updates of the deviated nasal septum, published in English around the world. Conclusion: NDS's have a critical role in functional and effective nasal breathing. Diagnostic modalities as rhinomanometry, acoustic rhinometry, as well as nasal spectral sound analysis can come in handy in identifying DNS. Though common, there are concerns that the benefits of nasal septal surgery might be mainly cosmetic. However, there is a debate on the effectiveness of adult septoplasty for nasal obstruction. Keywords: Nasal septum deviation, classification, complications, Septoplasty, Management, Nasal septal surgery airflow dynamics. These changes have been reported on INTRODUCTION both sides; however, they are more extreme on the concave [10] The nasal airway acts as the primary path for inspired air to side .