Past Is Prologue a Watch, a Department and 160 Years of History
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Leider, Stephen G..Pdf
PROMOTION RECOMMENDATION The University of Michigan Stephen M. Ross School of Business Stephen G. Leider, associate professor of technology and operations, with tenure, Stephen M. Ross School of Business, is recommended for promotion to professor of technology and operations, with tenure, Stephen M. Ross School of Business. Academic Degrees Ph.D. 2009 Harvard Business School, Business Economics, Boston, MA M.A. 2006 Harvard Business School, Business Economics, Boston, MA B.A. 2003 Case Western Reserve University, Economics and Political Science, Cleveland, OH Professional Record: 2018 – Present Michael R. and Mary Kay Hallman Fellow, University of Michigan, Stephen M. Ross School of Business, Ann Arbor, MI 2017 – Present Associate Professor of Technology and Operations, University of Michigan, Stephen M. Ross School of Business, Ann Arbor, MI 2013 Sanford R. Robertson Assistant Professor of Business Administration, University of Michigan, Stephen M. Ross School of Business, Ann Arbor, MI 2009 – 2017 Assistant Professor of Technology and Operations, University of Michigan, Stephen M. Ross School of Business, Ann Arbor, MI Summary of Evaluation: Teaching: Professor Leider has taught BBA, MBA, and PhD classes. When teaching the undergraduate core class (OMS 311/TO 313), he got a teaching evaluation of 4.5/5.0. This is quite remarkable, as Professor Leider had never taken an Operations Management class before coming to Ross. He quickly transitioned to the role of course lead, where he mentored doctoral students and other faculty teaching the course. Taking advantage of his research background, Professor Leider improved the course materials by introducing behavioral operations into the class and further built on action‐based demonstrations. -
Strat-Ent-Org
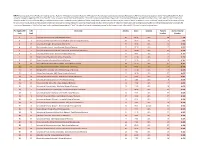
DATA: Data was pulled from UT Dallas for including journals: Academy of Management Journal, Academy of Management Review, Organization Science, Strategic Management, Administrative Science Quarterly Journal from 2015-2018 for the North American rankings in September 27th, 2019. The UTD "Score" in column E comes from the UTD Website. UTD counts number of papers those in top journals. For each paper UTD divides up credit among the authors. So if a paper has two authors, each school the author list as their affiliation will get .5 added to their UTD Score. In column H, Score / Number of faculty simply divides the UTD Score in column E by the number of faculty in column G. Please see the tab "Faculty Count" for the counts of faculty for each school. Faculty counts are from schools' websites and were pulled in Spring of 2018. If a school has fewer faculty now than reference period, it "helps" the school's per capita ranking because faculty who left contribute papers for numerator UTD Score but not denominator. If a school has more faculty now than reference period, it "hurts" the school's per capita ranking because new faculty's papers are not in the school's UTD score but are in the denominator. Per Capita UTD UTD University Articles Score Country Faculty Score / Faculty Rank Rank Number Number 1 1 University of Pennsylvania (The Wharton School) 80 46.71 USA 39 1.198 2 4 Pennsylvania State University at University Park (Smeal College of Business) 38 18.63 USA 17 1.096 3 15 University of Georgia (Terry College of Business) 32 13.02 USA 14 0.930 4 13 Rice University (Jesse H. -

U-M Ross School of Business Announces Speaker Lineup for Inaugural Positive Business Conference
U-M Ross School of Business Announces Speaker Lineup for Inaugural Positive Business Conference Convergence of business executives and academics offers first-of-its-kind conference experience Ann Arbor, Mich. – Feb. 18, 2014 – The University of Michigan’s Ross School of Business today unveiled the roster of high-profile speakers that will address attendees at its inaugural Positive Business Conference, which will take place May 15-17, 2014 at the Ross School of Business. C-level executives from companies including Whole Foods Market, Ford and Procter & Gamble will take the stage to share the most inspiring and practical positive business practices currently in place at their organizations. With a number of academics presenting and conducting workshops alongside world class business leaders, the breadth of business topics that will be addressed will make the conference a unique experience for all attendees. The three-day Positive Business Conference will bring together the diverse perspectives of business professionals, academics, students and industry luminaries. The conference will host sessions with both practical examples of positive business practices being implemented, as well as workshops based on the cutting-edge research underlying the practices. Select Ross faculty will lead interactive workshops on specific approaches to building positive businesses across a range of disciplines. Sample sessions include: • Alison Davis-Blake, Dean of Ross School of Business – What is Positive Business? In this opening session, Davis-Blake will lay out her vision for positive business, and why she made developing leaders who make a positive difference in the world the energizing mission of the Ross School of Business. -

Central Campus Medical Campus
D. R R LLE FU CENTRAL CAMPUS & MEDICAL CAMPUS MEDICAL 1 R DR. ENTE P BUILDING DIRECTORY SCHOOL L C A P CAMPUS F5 Alumni Center E5 Rackham Building OF NURSING IC D P D8 Angell Hall F8 Randall Laboratory (RAND) KKINGSLINGSLEY ST. E P . M UNIVERSITY HOSPITAL . T T E S C7 Betsy Barbour Residence (BBR) E11 Ross School of Business (ROSS) S W . 2 E5 Burton Memorial Tower G7 Ruthven Museums M E LLS H7 Central Campus Recreation Building (CCRB) F9 Shapiro Undergraduate Library (UGL) LLS D I C GA GA F6 Chemistry Building (CHEM) F10 School of Social Work A L E9 Clements Library (CL) D10 South Hall C N. IN N. IN E E9 Martha Cook Residence (COOK) C10 South Quad P N CATHERHERINE ST. T . TAUBMAN E E H4 Couzens Hall D5 202 S. Thayer Building (THAYER) E LIBRARY R R 3 V V D E A F7 Dana Building, School of Natural H6 Stockwell Hall A R H TAUBMAN MOLECULAR AND P . Resources & Environment (DANA) C8 Student Activities Building (SAB) C BIOMEDICAL SCIENCE BEHAVIORAL T I RESEARCH NEUROSCIENCE P GLEN GLEN G8 Dennison Building (DENN) D9 Tappan Hall (TAP) GRADUATE DETROIT A P Taubman Biomedical Science Research Building E. ANN ST. OBSERVATORY G6 School of Dentistry (DENT) G4 HOTEL N I I3 Detroit Observatory G3 Taubman Library Z COUZENS F7 Dow Laboratory (DOW) D8 Tisch Hall 4 G9 East Hall I9 Trotter Multicultural Center LL E. MEDMEDIICAL CENTERCENTER DR. E. HHUURON ST. P O ALMER FIELD P OWE G11 East Quad (Residential College) G5 Undergraduate Science Building (USB) Y D MARY F10 School of Education F5 University Health Service (UHS) RACKHKHAAM POWER P MARKLEY R A P CENTER LM F11 Executive Education J2 University Hospital NORTH L HALL A N QUAD E C8 Fleming Administration Building D11 Weill Hall (Ford School) R R E. -

New York Timescorrespondent Roger Cohen to Speak At
Washtenaw Jewish News Presort Standard In this issue… c/o Jewish Federation of Greater Ann Arbor U.S. Postage PAID 2939 Birch Hollow Drive Ann Arbor, MI Oh Jewish New Ann Arbor, MI 48108 Permit No. 85 Chanukah! Book Fair Cookbook Photo Album by Aviva and son Aric Page 12 Page 24 Page 31 December 2011/January 2012 Kislev/Tevet/Shevat 5772 Volume XXXVI: Number 4 FREE New York Times correspondent Roger Cohen to speak at U-M Hillel to honor incoming Kimberly Kunoff, special to the WJN director Tilly Shames n the evening of Sunday, February 5, your history, 2001, and foreign editor six months later. and outgoing director at 7 p.m., Roger Cohen, columnist end Jew ish Since 2004, he has written a column for The Michael Brooks O for the International Herald Tri- meekness and Times-owned International Herald Tribune, bune and New York Times, will speak at the humiliation, first for the news pages and then, since 2007, Michael Spitulnik, special to the WJN University of Michigan. His talk—“Israeli the acquies- for the Op-Ed page. In 2009 he was named The Ann Arbor Jewish Spring? The Enduring Jewish Question”— cence that took a columnist of The New York Times. community is invited to will ask how close, 63 years after the found- your forbears Cohen has written Hearts Grown Bru- a Chanukah celebration ing of the Jewish state, has Israel conformed to the ditches tal: Sagas of Sarajevo (Random House, to welcome Tilly Shames to its founding ideals. and the gas: 1998), an account of the wars of Yugosla- into her new role as ex- “Israel,” explains Cohen, “by giving Jews that was Israel’s via’s destruction, and Soldiers and Slaves: ecutive director of the at last a small piece of earth, was supposed message.” American POWs Trapped by the Nazis’ Final University of Michigan to create what Ben Gurion called ‘a self-suf- The lesson Gamble (Alfred A. -

An Operating Manual for the University of Michigan
An Operating Manual for the University of Michigan James and Anne Duderstadt © 2018 The Millennium Project, The University of Michigan All rights reserved. The Millennium Project The University of Michigan 2001 Duderstadt Center 2281 Bonisteel Boulevard Ann Arbor, MI 48109-2094 http://milproj.dc.umich.edu i Preface The University of Michigan clearly qualifies for on a firm belief that great things happen because of the inclusion in the small group of institutions that have ability, creativity, and commitment of great students, shaped American higher education. Michigan has faculty, and staff at the grassroots level. Put another long defined the model of the large, comprehensive, way, Michigan long ago discarded a top-down culture, public research university, with a serious commitment in which leaders tossed ideas out to be embraced and to scholarship and service. It has been distinguished implemented by the community. Instead, great ideas by unusual breadth, a rich diversity of academic and achievements at Michigan bubble up from the disciplines and professional schools, social and cultural academic programs at the department and school or activities, and intellectual pluralism. This unrelenting college level. commitment to academic excellence, broad student This ability to take risks, to experiment and access, and public service continues today. In virtually innovate, to explore various new directions in teaching, all national and international surveys, the university’s research, and service, defines Michigan’s unique role in programs rank among the very best, with most of its American higher education. In fact, beyond academic schools, colleges, and departments ranking in quality leadership, from time to time the University actually among the top ten nationally and with several regarded does something that changes the world! For example, as the leading programs in the nation. -
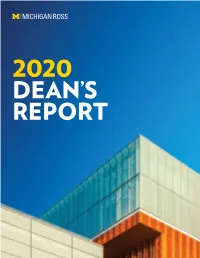
2020 Dean’S Report from the Dean
2020 DEAN’S REPORT FROM THE DEAN Greetings Michigan Ross Community, The year 2020 was an extraordinary year that not only tested our strength and resilience, but also that motivated us to work even harder to achieve our goals. Guided by our core values, we aimed for academic excellence and aspired to make a positive difference in the world during a global pandemic that impacted how we live, how we work, and of course, how we educate the next generation of business leaders. I am extremely proud of our Michigan Ross community of students, faculty, staff, alumni, and partners across the globe, and I am confident that after reviewing our 2020 Dean’s Report, you too will be proud to be a Wolverine! In fall 2019, we welcomed our inaugural Online MBA class and introduced a state-of-the-art digital education studio that is on the leading edge of innovation in educational technology. We also welcomed our most diverse and accomplished Full-Time MBA Class of 2021 with the highest percentage of women and underrepresented minority students in Ross School history. In addition to a stellar incoming MBA class, our 2019 MBA graduating class set a new record for the highest total salary package, and we were No. 1 in career placement across all U.S. business schools. Our 2019 BBA graduates also set their own records — for example with the highest-ever median salary package for undergraduates at the Ross School. The Ross School continues to be recognized as one of the leading business schools in the world. -
Walkingtour.Pdf
WELCOME Enter the Ross School of Business through the front entrance, 701 Tappan Street, Ann Arbor. ❙ The main Ross building opened in 2009. ❙ Stephen M. Ross graduated from the University of Michigan Business School in 1962 with a Bachelor of Business Administration degree. He went on to become founder and chairman of a large real-estate development firm in New York City. ❙ In 2004, Ross donated $100 million for reconstruction of the main building at the business school. ❙ In 2013, Ross donated an additional $200 million to be distributed between the Ross School of Business and the university’s athletic department. He remains the university’s largest donor. ❙ The Ross School of Business is LEED certified, recognized for using sustainable materials and numerous environmentally friendly features, including a “living roof” made of grass for insulation. ❙ Beyond the main building, the Ross campus also includes Wyly Hall, home to our Executive Education programs, and the Executive Learning & Conference Center, offering full-service hotel rooms and fine dining. Both buildings front on East University Avenue. ADMISSIONS INFORMATION Please visit michiganross.umich.edu/apply for more information on the admissions process and prerequisites. 1A 1B 1C SEIGLE CAFÉ 1D 1E TAPPAN STREET TAPPAN HILL STREET 1A. ROBERTSON ❙ Seats 500. AUDITORIUM ❙ Hosts business competitions, large From the Tappan Street conferences with national speakers, entrance, walk straight and major university speeches. down the main hall, past ❙ Home to student-organized events the stairs on the left. like the Michigan Sport Business Turn left at the Conference and the Women in “Butterfield Horses” Business speaker series. -

Ross Summer Connection
MAKING THE MOST OF MICHIGAN ROSS ROSS SUMMER CONNECTION For incoming first-year Ross students seeking early exposure to the rigor of Ross and U-M Ross Summer Connection (RSC) is an academic SUMMER PROGRAMMING learning community geared toward incoming Ross Students participating in RSC will join the program first-year students with a track record of success. the summer prior to their first semester. Participants attend RSC to accelerate their social, academic, and personal development through courses • 4-week residency on the University of and mentoring in an inclusive learning community. Michigan Central Campus in Ann Arbor RSC is a four-week, residential program that runs • Housing and meals are included July through August before a student’s first year at • Transportation throughout the program is provided Ross. However, students receive academic support through this program throughout their sophomore year. Participation in this program is by invitation-only. ACADEMIC YEAR PROGRAMMING Invitations are sent March-April. Programming continues throughout a student’s first and sophomore years, and includes: PROGRAM BENEFITS • Coaching Academic Exposure • Seminars Experience quantitative courses like Econ 101, • Mentorships Calc I, and Pre-Calc, as well as First-Year Writing, • Advising to familiarize yourself with Ross academics before • Social events your first term. Networking Surround yourself with peers with similar goals. From future study buddies to lifelong friends, you never know who you’ll meet at RSC. Personal Management Learn more about developing a personal and professional brand, managing time, balancing “Not only did RSC allow me to meet class schedules, and more. people who made me feel welcome, Community Service but it allowed me to get adjusted to Give back and engage with the local community by participating in RSC-hosted service projects. -
Insider's Guide: Stephen M. Ross School of Business
presents mbaMission’s Insider’s Guide Stephen M. Ross School of Business University of Michigan Ann Arbor, MI 2017–2018 mbaMission can help you stand apart from the thousands of other MBA applicants! Your Partner in the MBA Admissions Process Our dedicated, full-time admissions advisors work one-on-one with business school candidates, helping them showcase their most compelling attributes and craft the strongest possible applications. World’s Leading Admissions Consulting Firm With more five-star reviews on GMAT Club than any other firm, we are recommended exclusively by both leading GMAT prep companies, Manhattan Prep and Kaplan GMAT. Free 30-Minute Consultation Visit www.mbamission.com/consult to schedule your complimentary half-hour session and start getting answers to your most pressing MBA application and admissions questions! We look forward to being your partner throughout the application process and beyond. mbamission.com [email protected] THE ONLY MUST-READ BUSINESS SCHOOL WEBSITE Oering more articles, series and videos on MBA programs and business schools than any other media outlet in the world, Poets&Quants has established a reputation for well-reported and highly-creative stories on the things that matter most to graduate business education prospects, students and alumnus. MBA Admissions Consultant Directory Specialized Master’s Directory Poets&Quants’ MBA Admissions Consultant Directory For graduate business degree seekers looking for a offers future applicants the opportunity specialization along with or apart from an MBA, to find a coach or consultant to assist in their Poets&Quants' Specialized Master's Directory helps candidacy into a top business school. Search by cost, you narrow your results by program type, location, experience, education, language and more. -

University of Michigan, Ross School of Business
REQUEST FOR PROPOSAL RFP P 051214-01 KW Stephen M. Ross School of Business Brand Research RFP Release Date: May 12, 2014 Proposal Due Date: Monday, June 16, 2014 at 4:00 p.m. EST Submit Proposals To: Name: Kevin White Title: Procurement Agent Tele: 734-764-4432 Email: [email protected] Address: University of Michigan Procurement Services 3003 S. State Street 7071 Wolverine Tower Ann Arbor, MI 48109-1282 RFP P-051214-01KW TABLE OF CONTENTS RFP Section Topic Page # 1.0 Proposal Invitation 3 2.0 Planned Procurement Schedule 3 3.0 Background 4 4.0 Project Objectives 4 5.0 RFP Requirements 5 6.0 Submission Directions 6 Rights Reserved by the University and Restrictions on RFP 7.0 7 Process 8.0 Evaluation Criteria 8 9.0 Proposal Submission Format 8 RFP Attachments File Name Input Required (Separate Files) A Supplier’s Question Form For completion B Intent to Respond For completion C General and Professional Services Agreement For review D Signature Page For completion E Supplier Information & RFP Questionnaire For completion 380.03-12 Request for Proposal Template General and Professional Services Ver. 01.13 Page 2 of 12 RFP P-051214-01KW 1.0 PROPOSAL INVITATION The Stephen M. Ross School of Business at the University of Michigan seeks proposals from select suppliers that provide Brand Research Services. The Marketing and Communications department is looking to create a customized Ross Brand Tracking for the Business School that captures the brand associations that contribute the most to brand equity and the marketing activities supporting the brand. -
Download Our 2021 Virtual Commencement Program
THE STEPHEN M. ROSS SCHOOL OF BUSINESS AT THE UNIVERSITY OF MICHIGAN 20COMMENCEMENT 21 21 VIRTUAL COMMENCEMENT APRIL 30, 2021 10:00 AM 2 Letter from the Dean 4 Order of Exercises 6 Student Welcome and Name Readers 8 Student Speakers 10 Student Awards 14 Faculty Awards 16 Michigan Ross Faculty 20 PhD 22 Master of Business Administration 30 Master of Accounting 32 Master of Management 34 Master of Supply Chain Management 36 Bachelor of Business Administration 42 Welcome Alumni 46 Regents & Officers 1 LETTER FROM THE DEAN Dear Graduates, I am honored to celebrate our Michigan Ross Class of 2021. Congratulations on reaching this tremendous milestone. You have worked very hard to get to this moment, and I deeply admire your focus, determination, and unwavering commitment to your goals. The courage and fortitude you demonstrated, especially during this unprecedented year, are commendable. You are a true inspiration and shining example of what it means to be the Leaders and Best! Although we are not able to gather in person, we have put together an engaging and memorable virtual experience for you and your loved ones. We hope you enjoy this special day. As students, you have gained invaluable business skills, solved real-world challenges, and become the purpose-driven leaders that our world needs today more than ever before. This year in particular, you learned how to adapt and thrive amid uncertainty and ambiguity. Whether in person or virtually, you overcame challenges, bonded together in your greatest moments of need, and exceeded all expectations. You learned the importance of being open to and accepting of change, and you demonstrated exceptional teamwork as our students, faculty, staff, alumni, and partners across the globe came together to achieve our goals and support each other.