Development of a District Cord Blood Bank: a Model for Cord Blood Banking in the National Health Service
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Green Space in Horfield and Lockleaze
Horfield Lockleaze_new_Covers 16/06/2010 13:58 Page 1 Horfield and Lockleaze Draft Area Green Space Plan Ideas and Options Paper Horfield and Lockleaze Area Green Space Plan A spatial and investment plan for the next 20 years Horfield Lockleaze_new_Covers 09/06/2010 11:29 Page 2 Horfield and Lockleaze Draft Area Green Space Plan If you would like this Vision for Green Space in informationBristol in a different format, for example, Braille, audio CD, large print, electronic disc, BSL Henbury & Southmead DVD or community Avonmouth & Kingsweston languages, please contact Horfield & Lockleaze us on 0117 922 3719 Henleaze, Westbury-on-Trym & Stoke Bishop Redland, Frome Vale, Cotham & Hillfields & Eastville Bishopston Ashley, Easton & Lawrence Hill St George East & West Cabot, Clifton & Clifton East Bedminster & Brislington Southville East & West Knowle, Filwood & Windmill Hill Hartcliffe, Hengrove & Stockwood Bishopsworth & Whitchurch Park N © Crown Copyright. All rights reserved. Bristol City Council. Licence No. 100023406 2008. 0 1km • raising quality • setting standards • providing variety • encouraging use • Horfield Lockleaze_new_text 09/06/2010 11:42 Page 1 Ideas and Options Paper Horfield and Lockleaze Area Green Space Plan Contents Vision for Green Space in Bristol Section Page Park Page Gainsborough Square Park 8 1. Introduction 2 A city with good quality, Monks Park 9 2. Background 3 Horfield Common, including the Ardagh 10-11 attractive, enjoyable and Blake Road Open Space and 12 Rowlandson Gardens Open Space accessible green spaces which 3. Investment ideas and options to 7 Bonnington Walk Playing Fields 13 improve each open space within the area meet the diverse needs of all Dorian Road Playing Fields 14 4. -

Bristol Local Plan Review: Policies and Site Allocations Proposed to Be
Bristol Local Plan Review: Policies and site allocations proposed to be retained The following Bristol Local Plan policies and site allocations were proposed to be retained in the Bristol Local Plan Review consultation (March 2019). Core Strategy (July 2011) Policies • BCS7: Centres and retailing • BCS9: Green Infrastructure • BCS12: Community facilities • BCS16: Flood risk and water management • BCS21: Quality urban design • BCS22: Conservation and the historic environment Site Allocations and Development Management Policies (June 2014) Community Facilities policies • DM5: Protection of Community Facilities • DM6: Public Houses Centres and Retailing policies • DM7: Town Centre Uses • DM8: Shopping areas and frontages • DM9: Local centres • DM10: Food and drink uses and the evening economy • DM11: Markets Health policies • DM14: The Health Impacts of Development Green Infrastructure policies • DM15: Green Infrastructure Provision • DM16: Open Space for Recreation Bristol Local Plan Review: Policies and site allocations proposed to be retained • DM17: Development involving existing green infrastructure (Trees and Urban Landscape) • DM19: Development and Nature Conservation • DM20: Regionally Important Geological Sites • DM21: Private Gardens • DM22: Development Adjacent to Waterways Transport and Movement policies • DM23: Transport Development Management • DM25: Greenways Design and Conservation policies • DM27: Layout and form • DM28: Public Realm • DM29: Design of New Buildings • DM30: Alterations to Existing Buildings • DM31: Heritage -

Local Resident Submissions to the Bristol City Council Electoral Review
Local resident submissions to the Bristol City Council electoral review This PDF document contains local resident submissions with surnames B. Some versions of Adobe allow the viewer to move quickly between bookmarks. 13 February 2015 I have lived in Westbury on Trym village since 1991 first with my parents and then more recently with my own family. I have always valued the community which flows out from the historical village centre, under the new boundaries my home would no longer be part of this community and I would consider this a great personal loss. Surely the history and heritage of Westbury Village should carry some weight and significance when considering new ward boundaries. I fail to understand how it can be seen as acceptable to have the heart of Westbury on Trym Village boundaries moved to fall under the ward of Henleaze, which does not have the historic significance and village community. Also why it is acceptable for the downsized remaning part of Westbury Village to have only one councillor but this is not ok for any other ward. I therefore support the proposal to have a partnership ward with Henleaze and to share 3 councillors between us. I understand this is the only way to maintain the historical identity and preserve the integrity of the whole village. If other proposed changes were to go ahead I have concern for the value of my property as it would be separated from the historic village centre and fear that at some future date could be absorbed onto other wards. I would also like to include the following good reasons -

Green Space in Ashley, Easton and Lawrence Hill
Ashley Easton Lawrence Hill AGSP_new_Covers 09/06/2010 11:24 Page 1 Ideas and Options Paper Ashley, Easton and Lawrence Hill Area Green Space Plan Ideas and Options Paper Ashley, Easton and Lawrence Hill Area Green Space Plan A spatial and investment plan for the next 20 years • raising quality • setting standards • providing variety • encouraging use • 1 Ashley Easton Lawrence Hill AGSP_new_Covers 09/06/2010 11:24 Page 2 Ideas and Options Paper Ashley, Easton and Lawrence Hill Area Green Space Plan If you would like this Vision for Green Space in informationBristol in a different format, for example, Braille, audio CD, large print, electronic disc, BSL Henbury & Southmead DVD or community Avonmouth & Kingsweston languages, please contact Horfield & Lockleaze us on 0117 922 3719 Henleaze, Westbury-on-Trym & Stoke Bishop Redland, Frome Vale, Cotham & Hillfields & Eastville Bishopston Ashley, Easton & Lawrence Hill St George East & West Cabot, Clifton & Clifton East Bedminster & Brislington Southville East & West Knowle, Filwood & Windmill Hill Hartcliffe, Hengrove & Stockwood Bishopsworth & Whitchurch Park N © Crown Copyright. All rights reserved. Bristol City Council. Licence No. 100023406 2008. 0 1km • raising quality • setting standards • providing variety • encouraging use • Ashley Easton Lawrence Hill AGSP_new_text 09/06/2010 11:18 Page 1 Ideas and Options Paper Ashley, Easton and Lawrence Hill Area Green Space Plan Contents Vision for Green Space in Bristol Section Page Park Page A city with good quality, 1. Introduction 2 Riverside Park and Peel Street Green Space 9 Rawnsley Park 10-12 attractive, enjoyable and 2. Background 3 Mina Road Park 13 accessible green spaces which Hassell Drive Open Space 14-15 meet the diverse needs of all 3. -

Auctions 22 Richmond Hill, Clifton, Bristol BS8 1BA
0117 973 4940 Auctions 22 Richmond Hill, Clifton, Bristol BS8 1BA LOT 999 - 20 Burnell Drive, St Pauls, Bristol, BS2 9JU For auction Guide Price £85,000 + A substantial 3 bedroom maisonette arranged over the first and second floors of a purpose built block of flats in St Pauls. The property is situated in a central location with easy access provided to the City Centre, Cabot Circus and the M32. A fantastic buy to let investment. LOT 999 - 20 Burnell Drive, St Pauls, Bristol, BS2 9JU FOR SALE BY AUCTION TENURE This property is due to be auctioned on the 26th November 2019 at The Grace We understand the property is to be sold on the residue of a 125 year lease Room, The Bristol Pavilion, County Ground, Nevil Road, Bishopston, Bristol at from 30 June 2003. Please refer to legal pack for further details. 7pm. TENANCY DETAILS VIEWING We understand the flat is currently let producing £700 per calendar month By appointment (£8,400 per annum) although we have not been provided with a copy of the tenancy agreement. SUMMARY SPACIOUS 3 BEDROOM MAISONETTE IN A CENTRAL LOCATION ENERGY PERFORMANCE CERTIFICATE Rating: D. DESCRIPTION A purpose- built first and second floor maisonette, situated in a central location SOLICITOR in St Pauls. The spacious accommodation (approx. 879 sq ft) is arranged to Ms A Taylor, Priority Law Limited provide a lounge, kitchen/diner, 3 bedrooms and a bathroom. We are informed Tel: 0161 249 9501 that the flat is currently let producing £700 pcm although we have not yet been Email: [email protected] provided with a copy of the tenancy agreement. -

38 Henleaze Gardens HENLEAZE • BRISTOL a Handsome Period Family Home in Need of Full Refurbishment
38 Henleaze Gardens HENLEAZE • BRISTOL A handsome period family home in need of full refurbishment Accommodation in excess of 4,000 sq ft • Flexible accommodation • Potential for up to 7 bedrooms 3 reception rooms • 2 bath/shower rooms • Garden • Extensive cellar Henleaze shops 0.2 miles • Clifton Village 2.6 miles • Bristol City Centre 2.6 miles Temple Meads Railway Station 3.8 miles • Bristol Airport 11.1 miles Situation Henleaze is a sought-after suburb of Bristol, adjacent to some 400 acres of bedroom. Each room is generously proportioned but requires modernising. public open space known as The Downs. As a family home this building could present 7 bedrooms, three reception rooms and three bathrooms/shower rooms. Badminton School, Redmaids, Clifton College, Clifton High, Bristol Grammar are all nearby Please note this building aff ords extensive cellars. Delightful walks are at Ashton Court and The Downs Outside Henleaze with a Waitrose, fi shmonger and butchers 38 Henleaze Gardens off ers a walled private rear garden M4 J19, M5 J17 or J19, Bristol Temple Meads to London Fixtures and fi ttings Paddington (approximately 90 minutes) Bristol Airport 11.1 miles, All those items regarded as tenant’s fi xtures and fi ttings, together with the London Heathrow 103 miles fi tted carpets, curtains and light fi ttings are included in the sale. The property - Freehold Tenure 38 Henleaze Gardens is a handsome period family home found on one Freehold of Henleaze’s most prestigious residential tree-lined streets. It is close to Local authority Henleaze Road with a wide variety of shops, a host of excellent local schools Bristol City Council Telephone: 0117 922 2000 and Bristol’s iconic Durdham Downs. -

Professor Philip Alston United Nations Special Rapporteur on Extreme Poverty and Human Rights
Professor Philip Alston United Nations Special Rapporteur on Extreme Poverty and Human Rights By email Our Ref: ZA37220 7 November 2018 Dear Professor Alston I am writing regarding your inquiry into poverty in the United Kingdom and in particular the challenges facing so-called peripheral estates in large cities. This week you have been in Bristol, one of the wealthiest cites in the United Kingdom and the only one of the ten Core Cities which is a net contributor to the UK Treasury. However, Bristol is also an unequal city and I am convinced that the actions of central government since 2010 have made this worse. The constituency which I am proud to represent, Bristol South, has the highest number of social security claimants in the city, the poorest health outcomes and the lowest educational attainment. The southern part of my constituency also suffers from extremely poor transport links to the rest of the city and higher crime than most areas. Thousands of people depend on national or local government for financial and other support, support which has been dramatically reduced since 2010. They have been hit disproportionately by the austerity imposed by the Conservative/Liberal Democrat coalition government 2010-15 and the Conservative government since 2015. The electoral ward of Hartcliffe and Withywood is the most south-eastern part of the city where it meets the countryside of North Somerset. It contains five of the ten most deprived communities in Bristol as defined by the Bristol City Council Local Super Output Area (LSOAs) Indices of Multiple Deprivation 2015. Nearby Filwood ward has a further three of these ten most deprived LSOAs. -

Schedule 1 Updated Jan 22
SCHEDULE 1 Sites 1 – 226 below are those where nuisance behaviour that relates to the byelaws had been reported (2013). These are the original sites proposed to be covered by the byelaws in the earlier consultation 2013. 1 Albany Green Park, Lower Cheltenham Place, Ashley, Bristol 2 Allison Avenue Amenity Area, Allison Avenue, Brislington East, Bristol 3 Argyle Place Park, Argyle Place, Clifton, Bristol 4 Arnall Drive Open Space, Arnall Drive, Henbury, Bristol 5 Arnos Court Park, Bath Road, , Bristol 6 Ashley Street Park, Conduit Place, Ashley, Bristol 7 Ashton Court Estate, Clanage Road, , Bristol 8 Ashton Vale Playing Fields, Ashton Drive, Bedminster, Bristol 9 Avonmouth Park, Avonmouth Road, Avonmouth, Bristol 10 Badocks Wood, Doncaster Road, , Bristol 11 Barnard Park, Crow Lane, Henbury, Bristol 12 Barton Hill Road A/A, Barton Hill Road, Lawrence Hill, Bristol 13 Bedminster Common Open Space, Bishopsworth, Bristol 14 Begbrook Green Park, Frenchay Park Road, Frome Val e, Bristol 15 Blaise Castle Estate, Bristol 16 Bonnington Walk Playing Fields, Bonnington Walk, , Bristol 17 Bower Ashton Playing Field, Clanage Road, Southville, Bristol 18 Bradeston Grove & Sterncourt Road, Sterncourt Road, Frome Vale, Bristol 19 Brandon Hill Park, Charlotte Street, Cabot, Bristol 20 Bridgwater Road Amenity Area, Bridgwater Road, Bishopsworth, Bristol 21 Briery Leaze Road Open Space, Briery Leaze Road, Hengrove, Bristol 22 Bristol/Bath Cycle Path (Central), Barrow Road, Bristol 23 Bristol/Bath Cycle Path (East), New Station Way, , Bristol 24 Broadwalk -
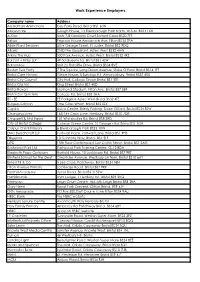
Work Experience Employers
Work Experience Employers Company name Address Aaardman Animations Gas Ferry Road. Bristol BS1 6UN Abbeycare Gough House, 13 Ellenborough Park North. W-S-M. BS23 1XH A-Gas Units 7-8 Gordano Court,Serbert Close.BS20 7FS Airbus Pegasus House.Aerospace Ave, Filton BS34 7PA Alide Plant Services Little George Street, St Judes. Bristol BS2 9DQ Allianz 2530 The Quadrant, Aztec West BS32 4AW Atkins The Hub 500 Park Avenue, Aztec West. Bristol BS32 4RZ Barcan + Kirby LLP 49-50 Queens Sq. Bristol BS1 4LW Barnardo's Unit 2a Ratcliffe Drive. Bristol BS34 8VE Boston Tea Party 7 The Square, Long Down Avenue. Stoke Gifford. Bristol BS16 1FT Bristol Care Homes Glebe House, 5 Sundays Hill. Almondsbury. Bristol BS32 4DS Bristol City Council City Hall, College Green Bristol BS1 5TR Bristol Old Vic King Street Bristol BS1 4ED Bristol Rovers Memorial Stadium. Filton Ave. Bristol BS7 0BF Bristol Zoo Gardens College Rd, Bristol BS8 3HA BT - EE EE Parkgate Aztec West Bristol BS32 4TE Burgess-Salmon One Glass Wharf, Bristol BS2 0ZX Capita Aviva Centre, Brierly Furlong. Stoke Gifford. Bristol BS34 8SW Changing Lives 163-165 Crow Lane, Henbury. Bristol BS10 7DR Chappell & Matthews 151 Whiteladies Rd. Bristol BS8 2RD City of Bristol College College Green Centre, St George's Rd. Bristol BS1 5UA Corpus Christi Primary 6 Ellenborough Park BS23 1XW DAC Beachcroft LLP Portwall Place. Portwall Lane. Bristol BS1 9HS Diligenta 10 Cannons Way, Bristol. BS1 5LF DPD 15th Floor Castlemead. Lwr Castle Street. Bristol BS1 3AG Eastwood Park Ltd Eastwood Park Training Centre. GL12 8DA Elizabeth Pope Opticians Horfield House, 10 Lockleaze Rd. -

FOI 114/11 Crimes in Schools September 2010 – February 2011
FOI 114/11 Crimes in Schools September 2010 – February 2011 Incident Premisies Name Town / City Current Offence Group Count Abbeywood Community School Bristol Theft And Handling Stolen Goods 4 Alexandra Park Beechen Cliff School Bath Criminal Damage 1 Alexandra Park Beechen Cliff School Bath Theft And Handling Stolen Goods 4 Alexandra Park Beechen Cliff School Bath Violence Against The Person 1 Allen School House Bristol Theft And Handling Stolen Goods 0 Archbishop Cranmer Community C Of E School Taunton Burglary 1 Ashcombe Cp School Weston-Super-Mare Theft And Handling Stolen Goods 2 Ashcombe Primary School Weston-Super-Mare Violence Against The Person 0 Ashcott Primary School Bridgwater Theft And Handling Stolen Goods 0 Ashill Primary School Ilminster Theft And Handling Stolen Goods 1 Ashley Down Infant School Bristol Theft And Handling Stolen Goods 2 Ashton Park School Bristol Other Offences 1 Ashton Park School Bristol Sexual Offences 1 Ashton Park School Bristol Theft And Handling Stolen Goods 1 Avon Primary School Bristol Burglary 2 Backwell School Bristol Burglary 3 Backwell School Bristol Theft And Handling Stolen Goods 1 Backwell School Bristol Violence Against The Person 1 Badminton School Bristol Violence Against The Person 0 Banwell Primary School Banwell Theft And Handling Stolen Goods 1 Bartletts Elm School Langport Criminal Damage 0 Barton Hill County Infant School & Nursery Bristol Burglary 1 Barton Hill Primary School Bristol Violence Against The Person 0 Barwick Stoford Pre School Yeovil Fraud Forgery 1 Batheaston Primary -

FACTS ABOUT DONATING Blood WHY SHOULD I DONATE BLOOD? HOW MUCH BLOOD DO I HAVE? Blood Donors Save Lives
FACTS ABOUT DONATING BLOOD WHY SHOULD I DONATE BLOOD? HOW MUCH BLOOD DO I HAVE? Blood donors save lives. Volunteer blood donors provide An adult has about 10–11 pints. 100 percent of our community’s blood supply. Almost all of us will need blood products. HOW MUCH BLOOD WILL I donate? Whole blood donors give 500 milliliters, about one pint. WHO CAN DONATE BLOOD? Generally, you are eligible to donate if you are 16 years of WHAT HAPPENS TO BLOOD AFTER I donate? age or older, weigh at least 110 pounds and are in good Your blood is tested, separated into components, then health. Donors under 18 must have written permission distributed to local hospitals and trauma centers for from a parent or guardian prior to donation. patient transfusions. DOES IT HURT TO GIVE BLOOD? WHAT ARE THE MAIN BLOOD COMPONENTS? The sensation you feel is similar to a slight pinch on the Frequently transfused components include red blood arm. The process of drawing blood should take less than cells, which replace blood loss in patients during surgery ten minutes. or trauma; platelets, which are often used to control or prevent bleeding in surgery and trauma patients; and HOW DO I PREPARE FOR A BLOOD DONATION? plasma, which helps stop bleeding and can be used to We recommend that donors be well rested, eat a healthy treat severe burns. Both red blood cells and platelets meal, drink plenty of fluids and avoid caffeine and are often used to support patients undergoing cancer alcohol prior to donating. treatments. WHAT CAN I EXPECT WHEN I DONATE? WHEN CAN I DONATE AGAIN? At every donation, you will fill out a short health history You can donate whole blood every eight weeks, platelets questionaire. -

515 Bus Service Valid from January 2019
.travelwest.info www BD11449 DesignedandprintedonsustainablysourcedmaterialbyBristolDesign,CityCouncil–January2019 on 0117 922 2910 922 0117 on CD-ROM or plain text please contact Bristol City Council Council City Bristol contact please text plain or CD-ROM Braille, audio tape, large print, easy English, BSL video, video, BSL English, easy print, large tape, audio Braille, If you would like this information in another language, language, another in information this like would you If Hartcliffe – Imperial Park Imperial – Hartcliffe Whitchurch – Hengrove Park – Park Hengrove – Whitchurch Stockwood – Hengrove – Hengrove – Stockwood Valid from January 2019 January from Valid Bus Service Bus 515 www.travelwest.info/bus other bus services in Bristol is available at: available is Bristol in services bus other Timetable, route and fares information for service 515 and and 515 service for information fares and route Timetable, Produced by Sustainable Transport. Sustainable by Produced www.bristolcommunitytransport.org.uk w: [email protected] e: contract by Bristol Community Transport. Community Bristol by contract 0117 941 3713 941 0117 t: under operated is and Council City Bristol please contact Bristol Community Transport: Community Bristol contact please Service 515 is financially supported by by supported financially is 515 Service enquiries property lost and information fares For 0 37 A SS PA holidays. public [email protected] Y e: B N O ST except Saturday to Monday operates service The A 2910 922 0117 t: G N LO Information