Effect of Pelvic, Hip, and Knee Position on Ankle Joint Range of Motion
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pelvic Anatomyanatomy
PelvicPelvic AnatomyAnatomy RobertRobert E.E. Gutman,Gutman, MDMD ObjectivesObjectives UnderstandUnderstand pelvicpelvic anatomyanatomy Organs and structures of the female pelvis Vascular Supply Neurologic supply Pelvic and retroperitoneal contents and spaces Bony structures Connective tissue (fascia, ligaments) Pelvic floor and abdominal musculature DescribeDescribe functionalfunctional anatomyanatomy andand relevantrelevant pathophysiologypathophysiology Pelvic support Urinary continence Fecal continence AbdominalAbdominal WallWall RectusRectus FasciaFascia LayersLayers WhatWhat areare thethe layerslayers ofof thethe rectusrectus fasciafascia AboveAbove thethe arcuatearcuate line?line? BelowBelow thethe arcuatearcuate line?line? MedianMedial umbilicalumbilical fold Lateralligaments umbilical & folds folds BonyBony AnatomyAnatomy andand LigamentsLigaments BonyBony PelvisPelvis TheThe bonybony pelvispelvis isis comprisedcomprised ofof 22 innominateinnominate bones,bones, thethe sacrum,sacrum, andand thethe coccyx.coccyx. WhatWhat 33 piecespieces fusefuse toto makemake thethe InnominateInnominate bone?bone? PubisPubis IschiumIschium IliumIlium ClinicalClinical PelvimetryPelvimetry WhichWhich measurementsmeasurements thatthat cancan bebe mademade onon exam?exam? InletInlet DiagonalDiagonal ConjugateConjugate MidplaneMidplane InterspinousInterspinous diameterdiameter OutletOutlet TransverseTransverse diameterdiameter ((intertuberousintertuberous)) andand APAP diameterdiameter ((symphysissymphysis toto coccyx)coccyx) -

Systematic Approach to the Interpretation of Pelvis and Hip
Volume 37 • Number 26 December 31, 2014 Systematic Approach to the Interpretation of Pelvis and Hip Radiographs: How to Avoid Common Diagnostic Errors Through a Checklist Approach MAJ Matthew Minor, MD, and COL (Ret) Liem T. Bui-Mansfi eld, MD After participating in this activity, the diagnostic radiologist will be better able to identify the anatomical landmarks of the pelvis and hip on radiography, and become familiar with a systematic approach to the radiographic interpretation of the hip and pelvis using a checklist approach. initial imaging examination for the evaluation of hip or CME Category: General Radiology Subcategory: Musculoskeletal pelvic pain should be radiography. In addition to the com- Modality: Radiography plex anatomy of the pelvis and hip, subtle imaging fi ndings often indicating signifi cant pathology can be challenging to the veteran radiologist and even more perplexing to the Key Words: Pelvis and Hip Anatomy, Radiographic Checklist novice radiologist given the paradigm shift in radiology residency education. Radiography of the pelvis and hip is a commonly ordered examination in daily clinical practice. Therefore, it is impor- tant for diagnostic radiologists to be profi cient with its inter- The initial imaging examination for the evaluation pretation. The objective of this article is to present a simple of hip or pelvic pain should be radiography. but thorough method for accurate radiographic evaluation of the pelvis and hip. With the advent of cross-sectional imaging, a shift in residency training from radiography to CT and MR imag- Systematic Approach to the Interpretation of Pelvis ing has occurred; and as a result, the art of radiographic and Hip Radiographs interpretation has suffered dramatically. -

Applied Anatomy of the Hip RICARDO A
Applied Anatomy of the Hip RICARDO A. FERNANDEZ, MHS, PT, OCS, CSCS • Northwestern University The hip joint is more than just a ball-and- bones fuse in adults to form the easily recog- socket joint. It supports the weight of the nized “hip” bone. The pelvis, meaning bowl head, arms, and trunk, and it is the primary in Latin, is composed of three structures: the joint that distributes the forces between the innominates, the sacrum, and the coccyx pelvis and lower extremities.1 This joint is (Figure 1). formed from the articu- The ilium has a large flare, or iliac crest, Key PointsPoints lation of the proximal superiorly, with the easily palpable anterior femur with the innomi- superior iliac spine (ASIS) anterior with the The hip joint is structurally composed of nate at the acetabulum. anterior inferior iliac spine (AIIS) just inferior strong ligamentous and capsular compo- The joint is considered to it. Posteriorly, the crest of the ilium ends nents. important because it to form the posterior superior iliac spine can affect the spine and (PSIS). With respect to surface anatomy, Postural alignment of the bones and joints pelvis proximally and the PSIS is often marked as a dimple in the of the hip plays a role in determining the femur and patella skin. Clinicians attempting to identify pelvic functional gait patterns and forces associ- distally. The biomechan- or hip subluxations, leg-length discrepancies, ated with various supporting structures. ics of this joint are often or postural faults during examinations use There is a relationship between the hip misunderstood, and the these landmarks. -

2019 Radiology Cpt Codes
2019 RADIOLOGY CPT CODES BONE DENSITOMETRY 1 Bone Density/DEXA 77080 CT 1 CT Abd & Pelvis W/ Contrast 74177 1 CT Enterography W/ Contrast 74177 1 CT Max/Facial W/O Contrast 70486 # CT Sinus Complete W/O Contrast 70486 1 CT Abd & Pelvis W W/O Contrast 74178 1 CT Extremity Lower W/ Contrast 73701 1 CT Neck W/ Contrast 70491 # CT Sinus Limited W/O Contrast 76380 1 CT Abd & Pelvis W/O Contrast 74176 1 CT Extremity Lower W/O Contrast 73700 1 CT Neck W/O Contrast 70490 # CT Spine Cervical W/ Contrast 72126 1 CT Abd W/ Contrast 74160 1 CT Extremity Upper W/ Contrast 73201 1 CT Orbit/ IAC W/ Contrast 70481 # CT Spine Cervical W/O Contrast 72125 1 CT Abd W/O Contrast 74150 1 CT Extremity Upper W/O Contrast 73200 1 CT Orbit/ IAC W/O Contrast 70480 # CT Spine Lumbar W/ Contrast 72132 1 CT Abd W W/O Contrast 74170 1 CT Head W/ Contrast 70460 1 CT Orbit/ IAC W W/O Contrast 70482 # CT Spine Lumbar W/O Contrast 72131 1 CT Chest W/ Contrast 71260 1 CT Head W/O Contrast 70450 1 CT Pelvis W/ Contrast 72193 # CT Spine Thoracic W/ Contrast 72129 1 CT Chest W/O Contrast 71250 1 CT Head W W/O Contrast 70470 1 CT Pelvis W/O Contrast 72192 # CT Spine Thoracic W/O Contrast 72128 1 CT Chest W W/O Contrast 71270 1 CT Max/Facial W/ Contrast 70487 1 CT Pelvis W W/O Contrast 72194 # CT Stone Protocol W/O Contrast 74176 CTA 1 Cardiac Calcium Score only 75571 1 CT Angiogram Abd & Pelvis W W/O Contrast 74174 1 CT Angiogram Head W W/O Contrast 70496 # CT / CTA Heart W Contrast 75574 1 CT Angiogram Abdomen W W/O Contrast 74175 1 CT Angiogram Chest W W/O Contrast 71275 -

Clinical Pelvic Anatomy
SECTION ONE • Fundamentals 1 Clinical pelvic anatomy Introduction 1 Anatomical points for obstetric analgesia 3 Obstetric anatomy 1 Gynaecological anatomy 5 The pelvic organs during pregnancy 1 Anatomy of the lower urinary tract 13 the necks of the femora tends to compress the pelvis Introduction from the sides, reducing the transverse diameters of this part of the pelvis (Fig. 1.1). At an intermediate level, opposite A thorough understanding of pelvic anatomy is essential for the third segment of the sacrum, the canal retains a circular clinical practice. Not only does it facilitate an understanding cross-section. With this picture in mind, the ‘average’ of the process of labour, it also allows an appreciation of diameters of the pelvis at brim, cavity, and outlet levels can the mechanisms of sexual function and reproduction, and be readily understood (Table 1.1). establishes a background to the understanding of gynae- The distortions from a circular cross-section, however, cological pathology. Congenital abnormalities are discussed are very modest. If, in circumstances of malnutrition or in Chapter 3. metabolic bone disease, the consolidation of bone is impaired, more gross distortion of the pelvic shape is liable to occur, and labour is likely to involve mechanical difficulty. Obstetric anatomy This is termed cephalopelvic disproportion. The changing cross-sectional shape of the true pelvis at different levels The bony pelvis – transverse oval at the brim and anteroposterior oval at the outlet – usually determines a fundamental feature of The girdle of bones formed by the sacrum and the two labour, i.e. that the ovoid fetal head enters the brim with its innominate bones has several important functions (Fig. -
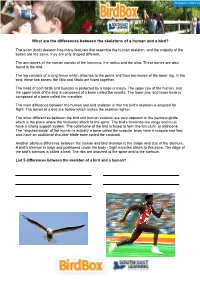
What Are the Differences Between the Skeletons of a Human and a Bird?
What are the differences between the skeletons of a human and a bird? The avian (bird) skeleton has many features that resemble the human skeleton, and the majority of the bones are the same, they are only shaped different. The arm bones of the human consist of the humerus, the radius and the ulna. These bones are also found in the bird. The leg consists of a long femur which attaches to the pelvis and then two bones of the lower leg. In the bird, these two bones: the tibia and fibula are fused together. The head of both birds and humans is protected by a large cranium. The upper jaw of the human, and the upper beak of the bird is composed of a bone called the maxilla. The lower jaw, and lower beak is composed of a bone called the mandible. The main difference between the human and bird skeleton is that the bird's skeleton is adapted for flight. The bones of a bird are hollow which makes the skeleton lighter. The other differences between the bird and human skeleton are very apparent in the pectoral girdle, which is the place where the forelimbs attach to the spine. The bird's forelimbs are wings and must have a strong support system. The collarbone of the bird is fused to form the furculum, or wishbone. The "shoulderblade" of the human is actually a bone called the scapula, birds have a scapula and they also have an additional shoulder blade bone called the corocoid. Another obvious difference between the human and bird skeleton is the shape and size of the sternum. -

Covariation Between Human Pelvis Shape, Stature, and Head Size Alleviates the Obstetric Dilemma
Covariation between human pelvis shape, stature, and head size alleviates the obstetric dilemma Barbara Fischera,b,1 and Philipp Mitteroeckerb aCentre for Ecological and Evolutionary Synthesis, Department of Biosciences, University of Oslo, NO-0316 Oslo, Norway; and bDepartment of Theoretical Biology, University of Vienna, 1090 Vienna, Austria Edited by Robert G. Tague, Louisiana State University, Baton Rouge, Louisiana, and accepted by the Editorial Board March 25, 2015 (received for review October 24, 2014) Compared with other primates, childbirth is remarkably difficult in response to changes in nutrition, poor food availability, and infec- humans because the head of a human neonate is large relative to tious disease burden, among others, might influence the severity of the birth-relevant dimensions of the maternal pelvis. It seems the obstetric dilemma (17–19). puzzling that females have not evolved wider pelvises despite the Despite the effect of environmental factors, pelvic dimensions high maternal mortality and morbidity risk connected to child- are highly heritable in human populations (most pelvic traits birth. Despite this seeming lack of change in average pelvic have heritabilities in the range of 0.5–0.8) (20) (SI Text and Table morphology, we show that humans have evolved a complex link S1). It has further been claimed that low levels of integration in between pelvis shape, stature, and head circumference that was the pelvis enable high evolvability (14, 21, 22), yet pelvis shape not recognized before. The identified covariance patterns contribute has seemingly not sufficiently responded to the strong selection to ameliorate the “obstetric dilemma.” Females with a large head, pressure imposed by childbirth. -

Knee Pain Program Targeting Hip, Pelvis, and Trunk Perform ____ Sets of ______Repetitions for Each Exercise
Knee Pain Program Targeting Hip, Pelvis, and Trunk Perform ____ sets of ______ repetitions for each exercise. I. Side Lying Straight Leg Raise Lying on side, kick leg back then raise straightened leg, hold, then lower to starting position. Ankle weights can also be added. II. Clam Shells With band around knees and keeping heels touching, move knees apart, with the action coming from the hip. III. Fire Hydrants Starting on all fours with band around knees, lift knee out to the side while keeping the hips stable and in place. IV. Bridges with Knee Extension Lying on back, lift hips off of table, then extend leg, and return to starting position. Repeat with opposite leg. Advanced position: Place arms across chest then complete as described. V. Standing Abduction/Extension Standing with band around effected leg, balance on one foot and move straight leg against the resistance of the band. VI. Lateral Step Downs Standing on 4-8 step with effected leg, lower body at the hip, keeping knees straight and hips level. Then raise up to return to the starting position. VII. Leg Press Perform leg press with addition of A Theraband around the knees. VIII. Wall Squat With a Theraband around the knees, perform a wall sit/squat. An exercise stability ball may be added to increase difficulty. IX. Kick Backs Standing in running stance on effected leg, with Theraband around opposite ankle, kick back, keeping effected knee bent. . -

Chapter 21: the Thigh, Hip, Groin, and Pelvis
Chapter 17: The Thigh, Hip, Groin, and Pelvis Anatomy of the Pelvis, Thigh, and Hip Bony Anatomy • Pelvic Girdle –Ilium • Iliac crest • Anterior superior iliac spine • Posterior superior iliac spine • Anterior inferior iliac spine • Ischium –Ischial tuberosity –Hamstring or bursa problems –Should sit on this area of pelvis • Pubis –Pubic symphysis • Acetabulum • Femur –Head –Neck –Greater trochanter –Lesser trochanter –Shaft –Medial condyle –Lateral condyle Ligaments - Major source of strength –Ligamentum teres-head of femur –Iliofemoral ligament • Y ligament • Strongest in the body • Prevents hyperextension, external rotation, abduction • Pubofemoral ligament –Prevents abduction • Ischiofemoral ligament –Prevents medial rotation Bursa • 18 in hip • Ischial bursa • Greater trochanteric bursa –Found at attachment of gluteus maximus and IT band • Iliopsoas Muscles • Flexors –Iliopsoas –Rectus femoris (quad) –Sartorius • Anterior thigh (quads) –Vastus medialis –Vastus lateralis –Vastus intermedialis • Extensors –Gluteus maximus –Semitendonosis (hamstring) –Semimembranosis (hamstring) –Biceps femoris (hamstring) • Abductors –Gluteus medius –Gluteus minimus –Tensor fascia latae (Iliotibial band) • Adductors –Adductor magnus –Adductor brevis –Adductor longus –Pectineus –Gracilis • External Rotators –Oburator externus –Obturator internus –Quadratus femoris –Piriformis – sciatic nerve goes through it. –Gamellus superior –Gamellus inferior –Gluteus maximus • Internal Rotators –Gluteus minimus –Tensor fascia Latae –Gluteus medius Assessment of the -

HUMAN PELVIS HEIGHT IS ASSOCIATED with OTHER PELVIS MEASUREMENTS of OBSTETRIC VALUE Munabi Ian G
ORIGINAL COMMUNICATION Anatomy Journal of Africa. 2015. Vol 4 (1): 457 – 465 HUMAN PELVIS HEIGHT IS ASSOCIATED WITH OTHER PELVIS MEASUREMENTS OF OBSTETRIC VALUE Munabi Ian G. *, Mirembe Florence, Luboga Sam A *Corresponding author; Munabi Ian G, Department of Anatomy, School of Biomedical Sciences, Makerere University College of Health Sciences, P.O. Box 7072 Kampala Uganda East Africa Telephone: +256772485474 Email: [email protected] ABSTRACT In low resource settings, perinatal death remains a major challenge, yet some of the key anthropometric measures used for screening have been found to be inappropriate. These calls for additional anatomically related measurements to act as a basis for the design of: easy-to-use, low technology accurate tools to enhance obstetric care quality in these settings. This study set out to determine the associations between the various pelvis anthropometric measurements of obstetric importance with pelvis height. The study made use of 30 complete rearticulated Adult pelvic bonesets of known sex. The some of the thirteen measurements made on each boneset included: Pelvis height, Sacral Anterior Orientation (SAO), pubic bone length, total pelvis height and inlet medial-lateral diameter. All measurements were taken thrice and the average used for comparisons with pelvis height. The non-parametric Mann-Whitney test and multilevel regression analysis test to control for gender was used. Pelvis height had significant associations with SAO (-0.36, P<0.01), pubic bone length (0.41, P<0.01), total pelvis height (0.21, P=0.04) and inlet medial-lateral diameter (0.46, P=0.02). Additional significant associations were observed with the diameters of the mid and outlet diameters of the birth canal. -

Getting the Maximus from Your Gluteus
Medically Speaking C he C k in g in feet contribute to injury risk as well—but in almost all cases of lower-body injury, the butt muscles are the weakest link. How does this work? There are two kinds of stability: dynamic and static. Pelvic stability is due largely to dynamic stability. What this means is that the stability around the pelvis is due to the muscular forces that act directly on it. Since muscle forces are dynamic entities, the stability they provide is, you guessed it, dynamic. If the muscles are strong, there is more pelvic stability. If they are weak, there is less. In contrast, the ankle joint, for example, is largely stabilized through static stability. This means that both ligaments around the joint and bones that comprise the joint, both of which are fixed or static types of stability, stabilize the ankle. Dynamic stability plays a much smaller role in the ankle than it does in the pelvis. I bet you’re wondering if you have a stable pelvis. If so, it’s easy to test. Stand in front of the mirror, balance on one leg and squat halfway to the floor. Try one leg, then the other. Does your pelvis stay level, or does it tilt on one side more than the other? The side where the pelvis tilts is your weaker side. Aside from the shock of seeing your pelvis tilt, the main issue here is injury risk. When the pelvis tilts, it means that it is unstable and the risk of the injuries mentioned is substantial. -

Three-Dimensional Kinematics of the Pelvis and Hind Limbs in Chimpanzee (Pan Troglodytes) and Human Bipedal Walking
Journal of Human Evolution 86 (2015) 32e42 Contents lists available at ScienceDirect Journal of Human Evolution journal homepage: www.elsevier.com/locate/jhevol Three-dimensional kinematics of the pelvis and hind limbs in chimpanzee (Pan troglodytes) and human bipedal walking Matthew C. O'Neill a, b, Leng-Feng Lee c, Brigitte Demes b, Nathan E. Thompson b, * Susan G. Larson b, Jack T. Stern Jr b, Brian R. Umberger c, a Department of Basic Medical Sciences, University of Arizona College of Medicine-Phoenix, Phoenix, AZ 85004, USA b Department of Anatomical Sciences, Stony Brook University School of Medicine, Stony Brook, NY 11794, USA c Department of Kinesiology, University of Massachusetts, Amherst, MA 01003, USA article info abstract Article history: The common chimpanzee (Pan troglodytes) is a facultative biped and our closest living relative. As such, Received 6 September 2014 the musculoskeletal anatomies of their pelvis and hind limbs have long provided a comparative context Accepted 20 May 2015 for studies of human and fossil hominin locomotion. Yet, how the chimpanzee pelvis and hind limb Available online 17 July 2015 actually move during bipedal walking is still not well defined. Here, we describe the three-dimensional (3-D) kinematics of the pelvis, hip, knee and ankle during bipedal walking and compare those values to Keywords: humans walking at the same dimensionless and dimensional velocities. The stride-to-stride and intra- Chimpanzee specific variations in 3-D kinematics were calculated using the adjusted coefficient of multiple corre- Human Kinematics lation. Our results indicate that humans walk with a more stable pelvis than chimpanzees, especially in Pelvis tilt and rotation.